Hyperparathyroidism
Original Editors - Suzette Austin & Erica Jezke from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Suzette Austin, Erica Jeszke, Lucinda hampton, Elaine Lonnemann, WikiSysop, 127.0.0.1, Kim Jackson and Admin
Introduction[edit | edit source]
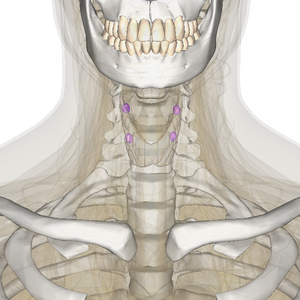
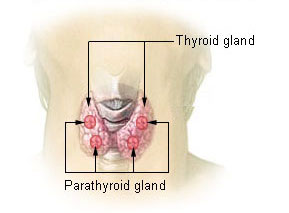
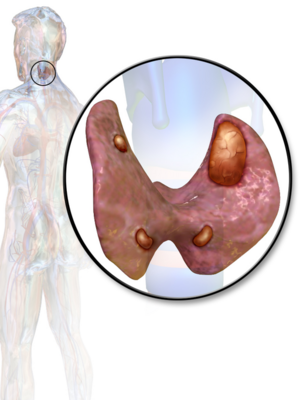
Hyperparathyroidism is a disorder caused by oversecretion of parathyroid hormone (PTH) by one or more of the four parathyroid glands.[1] This disorder can disrupt calcium, phosphate, and bone metabolism. [1]The parathyroid glands are located in the neck on the posterior surface of each lobe of the thyroid gland. [2][3] Each of the four parathyroid glands is about the size of a grain of rice.[3] As part of the endocrine system, these glands secrete parathyroid hormone (PTH), which regulates calcium and phosphorus. [2]
Even though the word “parathyroid” has the word “thyroid” in it, hyperparathyroidism has nothing to do with the thyroid gland, or with hypothyroidism or hyperthyroidism.
Watch this 5 minute video
Types[edit | edit source]
Hyperparathyroidism is classified into three groups: primary, secondary, or tertiary.[1]
- Primary hyperparathyroidism (most common type):a problem in which the parathyroid gland is releasing too much PTH, even though there is enough calcium already in the blood. Most of the time, this is caused by an adenoma (a non-malignant growth) of the parathyroid gland.[4]
- Secondary hyperparathyroidism occurs when the glands have become enlarged due to malfunction of another organ system.[1] Causes of secondary hyperparathyroidism include; severe deficiency in vitamin D, severe deficiency in calcium, and chronic renal failure. Chronic renal failure is the most common cause of secondary hyperparathyroidism.[5]
- Tertiary hyperparathyroidism is seen in dialysis clients who have chronic secondary hyperparathyroidism.[1] Dialysis clients who suffer from chronic renal failure lack the ability to absorb and convert vitamin D into a form that can be used by the body. This decline in vitamin D decreases the amount of calcium that can be absorbed.[5]
Epidemiology[edit | edit source]
Hyperparathyroidism may be a problem for roughly two or three women in 1,000, and primarily affects women over the age of 65. It is most common in post-menopausal women, but it can occur in males and females of any age.[4]
Most cases (80%) of hyperparthyroidism are discovered accidental during routine blood tests.[6]
Characteristics/Clinical Presentation[edit | edit source]
Hyperparathyroidism is supported biochemically by either an elevated serum parathyroid hormone level or an inappropriately normal level in the setting of hypercalcaemia.
Most people don’t experience any direct symptoms from their hyperparathyroidism. However, sometimes it may cause symptoms like the following: Fatigue; Weakness; Anxiety or depression; Lack of appetite; Abdominal pain; Nausea and vomiting; Constipation; Excessive thirst; Bone pain; Heart rhythm problems (rarely).
Symptoms may also occur from the complications of hyperparathyroidism. For example, hyperparathyroidism puts one at an increased risk of bone breaks, due to worsened osteoporosis. It also increases the chance of having kidney stones.[4]
Diagnosis[edit | edit source]
May include: Blood tests to check for calcium, phosphorus, magnesium and PTH levels; bone x-rays; kidney scans; biopsy.
Medical Management[edit | edit source]
Treatment for primary hyperparathyroidism is surgical removal of affected parathyroid gland, management of any bone or organ damage, and use of medication to protect bones prior to surgery or when parathyroidectomy is not an option. [1]
The treatment for secondary hyperparathyroidism will vary based on its cause.
- If secondary hyperparathyroidism is related to kidney disease a eg nephrologist may recommend: tic use, which mimics calcium circulating in the blood and may trick the parathyroid glands into releasing less parathyroid hormone; limit protein intake and take calcium supplements[7].
- Other causes of secondary hyperparathyroidism require different treatments. eg, avoid foods containing gluten if secondary hyperparathyroidism is from from celiac disease; take vitamin D supplements if secondary hyperparathyroidism is from a vitamin D deficiency[4].
Physical Therapy Management[edit | edit source]
Therapists may observe skeletal, articular and neuromuscular impairments associated with hyperparathyroidism. [1][3]
- In the acute phase, therapists should exercise caution with patients as they are at an increased risk for bone fracture.[1]
- After surgery, patients should be encouraged to ambulate as soon as possible to prevent further demineralization.[1]
- Encourage and aid patients in setting up their homes to avoid or minimise fall risks.[1]
Case Reports/ Case Studies[edit | edit source]
- A patient with persistent primary hyperparathyroidism due to a second ectopic adenoma.[8] A 33 year old woman was diagnosed with hyperparathyroidism and treated with parathyroidectomy. Post-operatively the patient’s serum calcium and PTH levels decreased but did not normalize and continued to present with kidney stones.
- Diplopia associated with hyperparathyroidism: report of a case.[9] A 60 year old man presented with diplopia as well as common symptoms of hyperparathyroidism. He was diagnosed with primary hyperparathyroidism and a search for the cause of the diplopia continued. After undergoing thyroidectomy his double vision was relieved as his serum calcium levels returned to normal.
- Primary hyperparathyroidism presenting as recurrent acute pancreatitis: A case report and review of literature[1] A 32 year old man presents with repetitive episodes of pancreatitis. Patient was treated by parathyroidectomy and recurrence of abdominal pain ceased and serum calcium levels normalized.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Goodman C, Fuller K.. Pathology: Implications for the Physical Therapist, 3rd ed. St. Louis, Missouri: Saunders Elsevir; 2007.
- ↑ 2.0 2.1 Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral, 5th ed. St. Louis, Missouri: Saunders Elsevir; 2013.
- ↑ 3.0 3.1 3.2 Mayo Clinic Staff. Diseases-conditions/hyperparathyroidism/basics/symptoms. http://www.mayoclinic.org (accessed January 16, 2014).
- ↑ 4.0 4.1 4.2 4.3 Very well health Hyperparathyroidism Available:https://www.verywellhealth.com/hyperparathyroidism-symptoms-causes-diagnosis-and-treatment-4688580 (accessed 3.4.20220
- ↑ 5.0 5.1 Mayo Clinic Staff. Diseases/conditions/hyperparathyroidism/basics/causes/ http://www.mayoclinic.org (accessed January 16, 2014)
- ↑ Skugor, M. Milas, M. Hypercalcemia [Internet].Accessed 2014 Apr 3. Available from: http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/endocrinology/hypercalcemia/
- ↑ Mayo Clinic Staff. Diseases-conditions/hyperparathyroidism/treatment. http://www.mayoclinic.org (accessed January 16, 2014).
- ↑ Hamdy N. A patient with persistent primary hyperparathyroidism due to a second ectopic adenoma. Natural Clinical Practice Endocrinology and Metabolism. [Serial on the Internet].2007 [cited 2014 Jan. 17];3:311-315. Available from:fckLRhttp://www.nature.com/nrendo/journal/v3/n3/full/ncpendmet0448.html
- ↑ Forman B.H., Ciardiello K., Landau S.J., Freedman J.K. (1995) 'Diplopia associated with hyperparathyroidism: report of a case', Yale J Biol Med, 68(5-6), pp. 215-217 [Online]. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2588946/ (Accessed: 17th January 2014).