Peabody Developmental Motor Scale (PDMS-2)
Original Editor - Wanda van Niekerk
Top Contributors - Wanda van Niekerk, Jess Bell, Kim Jackson, Mariam Hashem and Robin Tacchetti
Introduction[edit | edit source]
The Peabody Developmental Motor Scale was first developed and published in 1983 by Rhonda Folio and Rebecca Fewell.[1] A second edition was published in 2000 by the same authors (PDMS-2)[2] which was a more accurate, broader and complete assessment of motor performance.[3]
Benefits of the PDMS-2[edit | edit source]
- The PDMS-2 is an excellent tool for evaluating the motor development of young children as it provides separate tests and grading scales for both gross motor skills and fine motor skills.[4]
- Test battery standardisation was carried out with a total of 2003 children in the USA and Canada; it was the first battery that was standardised on a national level.[2][4]
- It is the only tool of its kind that combines evaluation with the planned intervention. A planned programme of 104 motor teaching and therapy activities are included.[2][4]
- These activities are organised based on the child’s development. The programme can help a child's skill development, as long as the evaluation of a child's skills based on the test battery is completed.[4]
Application of the PDMS-2[edit | edit source]
The PDMS-2 was designed to identify developmental delays in children. It can be used in various populations and settings to achieve specific goals. These may include[2][5][6]:
- assessing a child's motor competence relative to their peers
- for example, in a clinical setting where children with various diagnoses and a wide range of neuromuscular impairments can be assessed and therapy provided
- identifying delays or disorders in development
- for example, in a school / preschool setting to identify children who may have a developmental delay, as well as their strengths and weaknesses
- evaluating a child's progress
- this test was developed to identify strengths and weaknesses in a child’s motor development
- administering the test before and after a physiotherapy intervention is a good way to document the child’s progress and to measure the efficacy of the intervention
- research purposes
- the PDMS-2 is the gold standard and is often used in research and literature to assess the nature of motor development in various populations of children
- using specific skill deficits to develop indiviualised goals
- this helps in the design of treatment goals and a treatment plan based on the child’s strengths and weaknesses in motor development
Administrator Qualification[edit | edit source]
A range of healthcare professionals can perform the PDMS-2, including:
- physiotherapists
- occupational therapists
- psychologists
- doctors
- physical education teachers
You do not need to complete a specific course or accreditation to use the PDMS-2, but it is valuable to have good knowledge of the stages of child development (including typical and atypical development).[5] It is also recommended you have a thorough understanding of:[7]
- test statistics
- the general procedure governing test administration
- scoring and interpretation of the score
- specific information about gross and fine motor skills testing
- development in children who are not progressing like their peers
Validity and Reliability of PDMS-2[edit | edit source]
The PDMS-2 has been shown to be a reliable and valid measurement tool in various paediatric populations, such as:
- children with autistic spectrum disorder[8]
- children with cerebral palsy[9]
- children and babies born prematurely[10][11]
- children receiving physiotherapy for various diagnoses[12][13]
Target Population[edit | edit source]
The PDMS-2 can be used for children from birth to 5 years (60 months) old.[2]
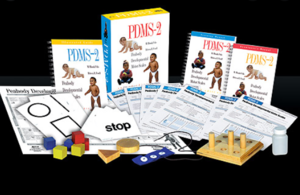
PDMS-2 Toolkit[edit | edit source]
The PDMS-2 Toolkit is available for online purchase and includes the following materials that are required to administer the test:
- Examiner's Manual
- includes the history of test development
- describes the validity and reliability of the test
- contains the various scoring charts
- The Guide to Item Administration
- includes a description and images of each of the activities or skills assessed
- Motor Activities Program Book
- includes various ways / options to teach a child the skills that they are having difficulty with
- the importance of various skills is also discussed and highlighted
- Profile / Summary Form
- a document where all raw data can be added to create a scoring graph
- Examiner's Record Booklet
- used by the therapist when administering the test to score all activities or skills assessed
- Test Manipulatives Document
- indicates what items are needed to administer the test, for example, an 8-inch ball, tennis ball, string, chair, tape measure, etc
- Peabody Motor Development Chart
Administration of the PDMS-2[edit | edit source]
Authors' Advice[edit | edit source]
- Read the manual beforehand
- Have someone assist who is familiar with the test
- Run the test three times before actually concluding a score
- Create a calm / nice environment
- Be sensitive to the child’s limitations – try to avoid the child becoming frustrated[2]
Important Tips[edit | edit source]
- All assessment items should be presented in a precise manner with specific verbal cues and demonstrations
- Administer the test in an environment with minimal distractions
- The area where the test is administered should be set-up beforehand, areas marked out and pre-measured and equipment ready. This helps to avoid any disruptions during the test and allows the test to flow. Examples of areas to pre-measure include[5]:
- A line on the floor clearly marked (with spray paint or duct tape) – 4 inches wide and 8 feet long
- An area for the child to run should be marked out – 10 feet (3m) 30 feet (9m), 45 feet (13m)
- Jumping distances should be demarcated
- Jumping from different heights – have benches of the correct heights ready
Description of the PDMS-2[edit | edit source]
The PDMS-2 assesses fine and gross motor skills of children from birth to five years old relative to their peers. There are four subtests for gross motor skills and two subtests for fine motor skills. The gross motor subtests include[14][15]:
- Reflexes (birth to 11 months)
- Stationary performances (all ages)
- Locomotion (all ages)
- Object manipulation (12 months and older)
The fine motor skills subtests include:
- Grasping (all ages)
- Visual-motor integration (all ages)
The total score is determined by the sum of the points of each subscale / item. Every item is rated on a 3-point rating scale. Internal consistency of the scale is very high (alpha = 0.97).[16]
Fine Motor Skills Subtests[edit | edit source]
The items per subtest for the fine motor skills part of the PDMS-2 are[2]:
- Grasping
- Grasping cubes
- Grasping a marker
- Buttoning/unbuttoning buttons
- Touching fingers
This video below by OT closet demonstrates how to score the fine motor portion of the test:
- Visual-motor integration
- Building tower / train / bridge / wall / steps / pyramid
- Snipping with scissors imitating a horizontal stroke
- Stringing beads
- Folding paper
- Copying a circle / cross / square
- Cutting paper / line / circle / square
- Lacing string
- Dropping pellets
- Tracing a line
- Connecting dots
- Colouring between lines
Administering the Gross Motor Function Part of the PDMS-2[edit | edit source]
Often in multidisciplinary teams, the physiotherapist assesses gross motor function and an occupational therapist focuses on the fine motor section. As already mentioned, the complete PDMS-2 has six subtests. The first four focus on gross motor skills and the last two on fine motor skills. For the purpose of this page, the focus will be on the gross motor skill subtests.
Reflexes:[edit | edit source]
- Investigates the child’s reaction to outside stimuli or the child's ability to automatically react to environmental events.
- This test is only administered to children under 1 year of age, as reflexes are typically integrated by the time a child is 12 months old.
- Eight different items are assessed under reflexes. Some of these are:
- Walking reflex
- Positioning reflex: Asymmetrical Tonic Neck Reflex (integrated)
- Landau reaction
- Protecting reaction - forward
- Protection reaction - side
- Right reaction - forward
- Protecting reaction - backward
Stationary[edit | edit source]
- This subtest assesses a child's ability to sustain control of their body within its centre of gravity and the ability to retain equilibrium
- Thirty different items are assessed under Stationary. These can include:
- rotating head
- stabilising trunk
- sitting
- raising to sit
- standing on 1 leg
- standing on toes
- initiation of movements such as:
- sit-ups
- push-ups
Locomotion[edit | edit source]
- This measures a child's ability to move from one place to another
- This is the largest section of the PDMS-2, assessing 89 items. Actions that are measured include:
- crawling
- walking
- running
- hopping
- jumping forward
- bearing weight
- rolling
- pushing up
- moving forward
- creeping
- scooting
- pivoting
- stairs climbing
- walking on a line
- jumping hurdles
- skipping
Object Manipulation[edit | edit source]
- This subtest measures a child's ability to manipulate balls, such as catching, throwing and kicking
- These skills are not apparent until a child is 11 months old, therefore this subtest is only administered in children aged 12 months and older
- This subtest includes 24 items. These include:
- catching a ball
- throwing a ball (overhand and underhand)
- kicking a ball
- hitting a target (overhand and underhand)
- bouncing a ball
- catching a bounced ball
Additional Comments[edit | edit source]
In addition, the therapist is encouraged to observe and record the following behaviours[7]:
- the child's interest in the task
- the child's approach to understanding the instructions
- the child's approach to problem-solving
- the child's comments or non-verbal response to the task
- the child's latency of response
- the child's use of self-corrections
- the child's preferred hand to use in throwing, grasping, etc
- the child's directionality in transferring materials
Grading and Scoring of the PDMS-2[edit | edit source]
The therapist will ask the child to do a specific item and observe how the child is doing the task. Items are scored as 2, 1 or 0.
- 0 = child cannot or will not attempt an item or the attempt does not indicate that the specific skill is emerging
- 1 = child's performance shows a clear resemblance to item mastery criteria but does not fully meet the criteria or there are signs of an emerging skill
- 2 = child performs item according to the criteria specified for mastering the skill
It is too time-consuming to administer the complete Examiner's Booklet for every child, so it is recommended to begin or enter the test at the entry point appropriate for the age of the child as marked in the scoring sheet. In the Examiner's Booklet, the different ages are marked in dark blue - this is where the test is "entered" and continued from. The test will begin at the basal level. This is the level where a child receives a score of 2 on three items in a row. The test will be stopped at the ceiling level. This is the level where a child scores 0 on each of three items in a row. This will be done for each subtest.[2]
Note that the skills to be assessed are all in chronological order. For example, if a child is not standing yet, the assessment will focus on activities such as rolling or crawling.[5]
The duration of the test is normally around 45 - 60 minutes. Some therapists prefer to do the gross motor and fine motor sections on different days, as doing them back to back may be too much for the child.
At any point of the PDMS-2, three gross motor subsets will be assessed. If the child is younger than 11 months, the three subsets included will be reflexes, stationary and locomotion. If the child is over 1 year, the three subsets to be assessed will be stationary, locomotion and object manipulation.
Examples of Scoring Subtest Items[edit | edit source]
Reflexes[edit | edit source]
When assessing the walking or stepping reflex in a child younger than 11 months, the therapist holds the child from under his chest up on a table. Allow the child to take some automatic steps. If the child is able to lift one foot and then the other in forward walking within three seconds, a score of 2 can be documented. If the child lifts one foot, but cannot take the steps within three seconds, a score of 1 can be documented. If the child's legs remain still and no steps are taken, a score of 0 can be documented.[5]
Locomotion[edit | edit source]
The child is asked to walk on a line, four inches wide and 8 feet long. If the child is able to walk on the line for six feet, a score of 2 is allocated.[5]
Scoring of the PDMS-2[edit | edit source]
Scoring of the PDMS-2 is documented on the scoring profile or summary form. This is done after the administration of the test. The raw data scores are used in conjunction with the various appendices available in the PDMS-2 reference guide and the following standardised scores can be calculated from these[2]:
- age equivalents
- percentiles
- standard scores
- gross motor quotients
Raw Score[edit | edit source]
The raw score is the sum of the various scores (0, 1 and 2) on each of the items. As the test is "entered" at the basal level (where child scores three 2s in a row), it may be assumed (and this assumption is built into the test) that the child also scored 2s on all the items before the start (basal level) of the test. These items also needed to be added as part of the raw score.
Profile Summary[edit | edit source]
The raw data scores are added to the profile summary form. It is key to know the child's age before commencing with the assessment, and with prematurely born children, the corrected age will be used up until 2 years old.
In the Examiner's Manual, Table A is used to determine the child's percentile rank for the various subtests, based on the raw score achieved. This percentile score can be used as an indication of whether physiotherapy is needed. The standard score of the various subtests is also extracted from Table A and also added to the profile summary document.
Table B in the Examiner's Manual will provide the gross motor score. The gross motor score is the sum of the standard scores of each of the subtests. Based on the gross motor score, the percentile rank of the child's gross motor abilities is determined.
Table C in the Examiner's Manual provides the age proficiency of the child for each of the separate subtests such as reflexes, stationary, locomotion and object manipulation.
On the Profile summary page, a graph can then be drawn up, based on all the various scores obtained from Tables A, B and C in the Examiner's Manual.
Score Interpretation[edit | edit source]
It is important to note that children from different countries may score differently from the scores provided in the PDMS-2. For example, in India, it has been shown that the children's gross motor skill norms are lower than in America.[28] Or in Israel, where baseball is not really played, throwing a tennis ball overhand and underhand might be a bit more difficult for children. Cultural differences may play a part in administering the test and the choice of objects used.
In premature babies, the gross motor deficit may become stronger over time.[10] For example, at 18 months, there may not be much of a deficit, and the child's score may fall within the wide developmental norm. However, at the age of 5, the deficits may be more obvious. Therapists are recommended to consider this in their assessment and treatment of the child and re-evaluate on a regular basis to ensure that the gross motor skill development gap is not getting larger, but getting smaller.
Therapy Goals and Planning[edit | edit source]
The Motor Activities Program Book is a very useful tool to consult in the planning of therapy and goal setting. It provides reasons for the child to be able to perform the various skills. It also provides useful ways to address developmental delays associated with each of the items and gives examples of progressions. It can provide the therapist with good ideas on how to start off with therapy and address the specific developmental issues. It can also help with the planning of a home programme where parents or caregivers can also be involved in helping the child.[5]
Ultimately, our goal of therapy is to be able to help the child with developmental delays to be a happier, productive, motor proficient and moving child in their environment.[5]
References[edit | edit source]
- ↑ Folio MR, Fewell RR. Peabody developmental motor scales and activity cards. DLM Teaching Resources; 1983.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Folio MR, Fewell RR. PDMS-2 Peabody developmental motor scales second edition. Austin: PRO-ED Inc. 2000.
- ↑ Valentini NC, Zanella LW. Peabody Developmental Motor Scales-2: The Use of Rasch Analysis to Examine the Model Unidimensionality, Motor Function, and Item Difficulty. Frontiers in Pediatrics. 2022 Apr 20;10:852732-.
- ↑ 4.0 4.1 4.2 4.3 Dourou E, Komessariou A, Riga V, Lavidas K. Assessment of gross and fine motor skills in preschool children using the Peabody Developmental Motor Scales Instrument. Eur Psychomotricity J. 2017;9:89-113.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 Taragin, A. Administration and Scoring of the Peabody Developmental Motor Scale - 2. Course, Plus2020.
- ↑ Zanella LW, Valentini NC, Copetti F, Nobre GC. Peabody Developmental Motor Scales-(PDMS-2): Reliability, content and construct validity evidence for Brazilian children. Research in Developmental Disabilities. 2021 Apr 1;111:103871.
- ↑ 7.0 7.1 Peabody Developmental Motor Scales (PDMS)– 2 Erin Chang, OTS, Karinette Leano, OTS, Thanh Luong, OTS, and Lisa Mireles, OTS. Presentation on Slideshare. Available from https://www.slideshare.net/stanbridge/peabody-developmental-motor-scales-pdms-2 (last accessed 27 August 2020).
- ↑ Holloway JM, Long TM, Biasini F. Relationships between gross motor skills and social function in young boys with an autism spectrum disorder. Pediatric physical therapy: the official publication of the Section on Pediatrics of the American Physical Therapy Association. 2018 Jul;30(3):184.
- ↑ Clutterbuck GL, Auld ML, Johnston LM. High‐level motor skills assessment for ambulant children with cerebral palsy: a systematic review and decision tree. Developmental Medicine & Child Neurology. 2020 Jun;62(6):693-9.
- ↑ 10.0 10.1 Tavasoli A, Azimi P, Montazari A. Reliability and validity of the Peabody Developmental Motor Scales-for assessing motor development of low birth weight preterm infants. Pediatric neurology. 2014 Oct 1;51(4):522-6.
- ↑ Wang M, Mei H, Liu C, Zhang Y, Huixian LI, Yan F. Application of the Peabody developmental motor scale in the assessment of neurodevelopmental disorders in premature infants. Chinese Pediatric Emergency Medicine. 2017 Jan 1;24(10):760-3.
- ↑ Phillips D. Concurrent Validity and Responsiveness of the Peabody Developmental Motor Scales-2 (PDMS-2) in Infants and Children with Pompe Disease undergoing Enzyme Replacement Therapy.
- ↑ Parmar Sanjay KS. Applicability of Peabody developmental Motor Scales PDMS-2 as a developmental assessment scale for Indian children. Occup Ther Int. 2008;2:1-3.
- ↑ Karimi H, Aliabadi F, Hosseini Jam M, Afsharkhas L. Evaluation of motor skills in high-risk infants based on Peabody Developmental Motor Scales (PDMS-2). International Journal of Children and Adolescents. 2016 Jan 10;2(1):4-7.
- ↑ Fay D, Wilkinson T, Anderson AD, Hanyzewski M, Hellwig K, Meador C, Schultz K, Wong J. Effects of Modified Instructions on Peabody Developmental Motor Scales, Gross Motor Scores in Children with Typical Development. Physical & occupational therapy in pediatrics. 2019 Jul 4;39(4):433-45.
- ↑ Minoliti R, Crepaldi M, Antonietti A. Identifying Developmental Motor Difficulties: A Review of Tests to Assess Motor Coordination in Children. Journal of Functional Morphology and Kinesiology. 2020 Mar;5(1):16.
- ↑ Mary Gavacs. MNE OTA 59 mo. # 7. Available from https://www.youtube.com/watch?v=HS6cdiNozmE (last accessed 17 November 2020)
- ↑ Mary Gavacs. MNE OTA Peabody Developmental Motor Scales: Fine Motor Subtest, 48 mo, #8.(last accessed 17 November 2020)
- ↑ Mary Gavacs. MNE OTA PDMS 59 months #10. (last accessed 17 November 2020
- ↑ Mary Gavacs. MNE OTA PDMS 59 mo #9. (last accessed 17 November 2020)
- ↑ Nicole Edmonds. Spontaneous Stepping Reflex. Published on 22 October 2018. Available from https://www.youtube.com/watch?v=cn7XPS21avE (last accessed 30 August 2020)
- ↑ Healthy Life. Postural Reflexes - Landau. Newborn Reactions (6 months). Published on 16 November 2014. Avaialable from https://www.youtube.com/watch?v=Q5pZNd93qEw. (last accessed 30 August 2020)
- ↑ Kaitlyn Morley. Stationary subset of PDMS-2. Published on 3 June 2015. Available from https://www.youtube.com/watch?v=rlo0gKpQ-ig&t=8s. (last accessed 30 August 2020)
- ↑ RP. Peabody Motor Skills Basal and Ceiling EXPLAINED!!!! Available from https://www.youtube.com/watch?v=XCrz-JwtRts. (last accessed 17 November 2020)
- ↑ Robby Carson. PDMS-2 Scoring. Available from https://www.youtube.com/watch?v=H6I0mxriCAU. (last accessed 17 November 2020)
- ↑ Robby Carson. Calculation and Interpretation of Scores of the Peabody. Available from https://www.youtube.com/watch?v=9iO5MqHKgxo&t=11s. (last accessed 17 November 2020)
- ↑ Cheyann Walters. Peabody Developmental Motor Scales - 2nd Edition. Published on 16 September 2019. Available from https://www.youtube.com/watch?v=cVW1NrFrs08. (last accessed 30 August 2020)
- ↑ Tripathi R, Joshua AM, Kotian MS, Tedla JS. Normal motor development of Indian children on Peabody developmental motor scales-2 (PDMS-2). Pediatric Physical Therapy. 2008 Jul 1;20(2):167-72.