Whipple Disease
Original Editor - Aya Alhindi
Top Contributors - Aya Alhindi
Introduction[edit | edit source]
Whipple's disease is a rare, chronic, systemic infectious disorder caused by a gram-positive intracellular bacterium, Tropheryma whipplei (TW).[1][2]The disorder can affect any system in the body but most commonly with prominent intestinal manifestations.[3] The patient exhibits the classically described signs of malabsorption caused by gastrointestinal colonization. However, it can exhibit clinically overlapping signs and symptoms with rheumatic diseases, potentially leading to misdiagnosis.[4]
Epidemiology[edit | edit source]
The epidemiology of WD is still unknown. It is a rare disease, with the majority of reports coming from North America and Europe.[5]So far, only about 1000 cases have been reported in the literature.[6] Whipple disease affects approximately one to three people out of every million. The disease reportedly primarily affects middle-aged/elderly men (the majority of reported cases are in men over the age of 55), with a 4:1 ratio, due to its association with wastewater workers and farmers (who are predominantly male) and the smoldering disease course, which can take many years to manifest and correctly diagnose.[4]
Pathophysiology[edit | edit source]
Chronic T whipplei infection appears to occur only in predisposed patients who have a lifetime susceptibility to T whipplei infection; on the one hand, Whipple's disease is extremely rare and usually develops over many years or even decades (insidious replication), while on the other hand, asymptomatic T whipplei carriage is common.[7] The host's genetic factors are thought to be a major factor in susceptibility, facilitating the development of familial clusters of cases. [4]HLA associations (HLA alleles DRB1*13 and DQB1*06) that interfere with antigen presentation,39 IL16 gene polymorphisms, and other polymorphisms that polarise cytokine production towards T-helper-2 (Th2)-cell activity are examples of a specific genetic predisposition. This specific genetic predisposition most likely explains the lifetime susceptibility of Whipple's disease patients as well as the clinically significant relapses in some individuals.[7]
It has been proposed that the genetic pattern of regulatory genes involved in the expression of inflammatory cytokines predisposes to infection.The immune system plays a critical role in the development of clinically visible disease. Infection may be eliminated or limited to asymptomatic colonisation of the gastrointestinal tract in the presence of fully functional immunity. [4]
The immune system plays a critical role in the development of clinically visible disease. Infection may be eliminated or limited to asymptomatic colonisation of the gastrointestinal tract in the presence of fully functional immunity. Tropheryma whipplei most commonly infects the small intestine. The bacterium produces an anti-inflammatory environment. The bacterium is phagocytosed by macrophages, but the cells are unable to kill the internalised bacteria due to the bacteria's ability to suppress the inflammatory response. This phenomenon is also linked to inappropriate antigen presentation and impaired macrophagic phagosome maturation. All of these factors contributed to a decrease in T cell response and an impaired immune response to infection.[4]
Signs and Symptoms[edit | edit source]
Whipple’s disease is characterized by a heterogeneous clinical picture and a plethora of symptoms and signs.[4]The disorder can affect any system in the body, including the brain, eyes, heart, joints, and lungs, but it most commonly affects the digestive system.Neurological symptoms may appear without gastrointestinal symptoms in rare cases and can mimic symptoms of nearly any neurological disease.[3]
Neurological symptoms may include:
- Dementia.
- Abnormalities of eye and facial muscle movements.
- Headaches.
- Seizures.
- Loss of muscle control.
- Memory loss.
- Weakness.
- Vision problems.
Gastrointestinal symptoms may include:
- Diarrhea.
- Weight loss.
- Fatigue.
- Weakness.
- Abdominal bleeding and pain.
Other symptoms:
- Fever.
- Cough.
- Anemia.
- Heart and lung damage.
- Darkening of the skin.
- Joint soreness.
Diagnosis[edit | edit source]
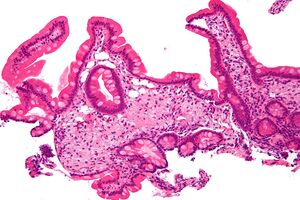
When WD is suspected, biopsy specimens collected from duodenal or other involved tissues showing positivity for periodic acid Shiff (PAS) staining and non-acid-fast in Ziehl-Neelsen staining can be used to confirm the diagnosis . The discovery of polymerase chain reaction (PCR), which can be used in a variety of biological samples, has made diagnosis more accessible in recent decades.[8]
The diagnosis is made based on the clinical characteristics, the presence of PAS-positive diastase-resistant granules in the small intestine macrophages, or species-specific polymerase chain reaction (PCR) using various T. whipplei genome sequences.[9]
This organism is phylogenetically related to the actinomycetes clade.It is a nonacid fast, Gram-positive rod-shaped bacillus. 1-2 P in length, thick walled, and stained with PAS dyes on the inside. The sequence of the 16s RNA gene was isolated from the intestine and then from pleural fluids, cardiac tissue, brain tissue, cerebrospinal fluid (CSF), and vitreous.[10]
Interleukin is used to deactivate macrophages during culture. PAS staining, electron microscopy, and genomic detection in biopsy materials, aspirated fluids, and other samples are currently available diagnostic tools.[10]
In the future, culture, monoclonal or polyclonal antibodies, and serology may be available.[6]
Treatment[edit | edit source]
Standard antibiotic treatment:
Because Whipple's disease is a rare systemic illness, controlled studies are unable to determine the best antibiotic regimens and treatment duration.Several antimicrobial drugs, including penicillin, penicillin combined with streptomycin, erythromycin, ampicillin, chloramphenicol, tetracycline, and trimethoprim-sulfamethoxazole, have been used successfully. The antibiotic resistance of Whipple's disease bacilli is also unknown. Clinical manifestations usually improve within a few weeks of starting antibiotic therapy. At the same time, positive PCR results may turn negative, indicating that the antibiotic treatment was effective. Histopathological findings, on the other hand, regress more slowly, and PAS-positive structures can persist for years. [11]
Alternative treatment regimens:
Oral-therapy-only with doxycycline plus hydroxychloroquine is now being tested against standard antibiotic therapy in a randomised controlled trial.Short-term treatment (ie, therapy duration of 3 months) was assessed retrospectively and prospectively.[7]
References[edit | edit source]
- ↑ El-Abassi R, Soliman MY, Williams F, England JD. Whipple’s disease. J Neurol Sci [Internet]. 2017;377:197–206.
- ↑ Tison A, Preuss P, Leleu C, Robin F, Le Pluart A, Vix J, et al. Rheumatological features of Whipple disease. Sci Rep [Internet]. 2021;11(1):12278.
- ↑ 3.0 3.1 1. Whipple’s Disease [Internet]. National Institute of Neurological Disorders and Stroke.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Kukull B, Mahlow J, Hale G, Perry LJ. Whipple’s disease: a fatal mimic. Autops Case Rep [Internet]. 2021;11:e2020237.
- ↑ Antunes C, Singhal M. Whipple Disease. StatPearls Publishing; 2023.
- ↑ 6.0 6.1 Chandra SR, Raj P, Pai AR, Reddy N. A case of Whipple’s disease: A very rare cause for rapidly progressive dementia. Indian J Psychol Med [Internet]. 2018;40(3):280–3.
- ↑ 7.0 7.1 7.2 1. Hujoel IA, Johnson DH, Lebwohl B, Leffler D, Kupfer S, Wu T-T, et al. Tropheryma whipplei infection (Whipple disease) in the USA. Dig Dis Sci [Internet]. 2019;64(1):213–23.
- ↑ Viegas AF, Lopes AM, Venade G, Rodrigues P, Tavares J. Why is Whipple’s disease still a challenging diagnosis? A case report and brief review of literature. Cureus [Internet]. 2023;15(1):e34029.
- ↑ Love S. Autopsy approach to infections of the CNS. Neuropathology: A Guide for Practising Pathologists. 2001 Jan 1:1-50.
- ↑ 10.0 10.1 Schoedon G, Goldenberger D, Forrer R, Gunz A, Dutly F, Höchli M, Altwegg M, Schaffner A. Deactivation of macrophages with interleukin-4 is the key to the isolation of Tropheryma whippelii. Journal of Infectious Diseases. 1997 Sep 1;176(3):672-7.
- ↑ Dutly F, Altwegg M. Whipple’s disease and “Tropheryma whippelii.” Clin Microbiol Rev [Internet]. 2001;14(3):561–83.