Falls Risk Assessment Tool (FRAT): Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
[[File:Falling.png|right|frameless]] | |||
[[Falls in elderly|Falls]] are problematic within the elderly population. Falls are the second leading cause of accidental injury deaths worldwide. Each year an estimated 684 000 individuals die from falls worldwide. Adults older than 60 years of age experience the greatest number of fatal falls.<ref>WHO Falls Available:https://www.who.int/news-room/fact-sheets/detail/falls (accessed 2.11.2022)</ref> | [[Falls in elderly|Falls]] are problematic within the elderly population. Falls are the second leading cause of accidental injury deaths worldwide. Each year an estimated 684 000 individuals die from falls worldwide. Adults older than 60 years of age experience the greatest number of fatal falls.<ref>WHO Falls Available:https://www.who.int/news-room/fact-sheets/detail/falls (accessed 2.11.2022)</ref> | ||
Revision as of 05:58, 2 November 2022
Original Editor - Shaun Jackson as part of the Northumbria University Innovation and Contemporary Physiotherapy Project
Top Contributors - Kim Jackson, Shaimaa Eldib, Lucinda hampton, Vidya Acharya, Shaun Jackson and Momina Khalid
Introduction[edit | edit source]
Falls are problematic within the elderly population. Falls are the second leading cause of accidental injury deaths worldwide. Each year an estimated 684 000 individuals die from falls worldwide. Adults older than 60 years of age experience the greatest number of fatal falls.[1]
A range of tools are available to health care providers to identify those at risk of falling. Tools include: Falls Risk Assessment Tool (FRAT); Berg Balance Scale; Timed Up and Go Test (TUG); The Balance Outcome Measure for Elder Rehabilitation (BOOMER).
FRAT[edit | edit source]
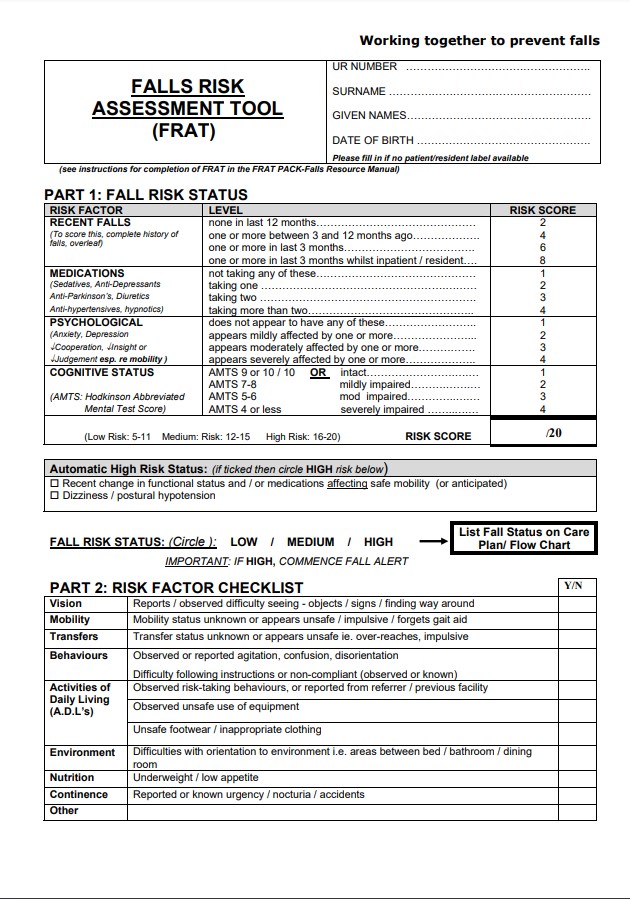
It is a 4-item falls-risk screening tool for sub-acute and residential care. The FRAT has three sections:
- Part 1 - falls risk status.
- Part 2 – risk factor checklist.
- Part 3 – action plan[2].
A full copy of the FRAT tool can be accessed via the following link: [1]
How Does Medication Affect Falls?[edit | edit source]
Impact of Cognitive Status on Falls[edit | edit source]
The motor and sensory systems are linked by higher-order neurological processes and cognition.[3] Research demonstrates that cognition has a key role in the regulation of gait and balance in older adults.[4] Additionally increased levels of cognition are required for movement planning and adapting to environmental changes.[5] Impairments in the cognition then can increase risk of falling.[6]
The cognitive test included in the FRAT is the Hodkinson Abbreviated Mental Test Score (ABTS). This test is used to assess for the possibility of dementia and is now sometimes used for other cognitive impairments[7]. Scores indicate the level of impairment, however more rigorous cognitive testing is required to confirm this.
Criticism of FRAT[edit | edit source]
Include:
- Risk Factor Checklist (Part 2) fails to appreciate balance specifically. If this was a self-reported concern of the patient, areas of proprioception and the vestibular system could be objectively looked at in more depth within specialist physiotherapy. assessment.
- Lacks context – eludes to being objective however fails to provide any guidance on questioning to obtain further information. Area for development – extended box to record subjective and objective measures.
- NICE guidelines state the FRAT does not assess all the risk variables highlighted in their guidelines for falls prevention. Furthermore, NICE state it should not be relied solely on to assess risk of falls and requires further investigation[8]. If high falls risk is identified, more extensive assessment is required – e.g. Elderly Mobility Scale to provide objective measures that guide physiotherapy treatment.
- Nowhere to record a collateral history. Having an area to collect information would allow for exploration into issues and areas highlighted in Part 2.
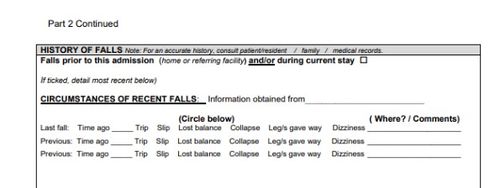
- ‘History of Falls’ section lacks ability to record detailed mechanics of fall. Tick boxes can be supported by a descriptive component. (See ‘Potential Modifications to the FRAT’).
- Cognitive test included is rather outdated and cannot be relied on to confirm cognitive impairment.
- Recommendation: carry out with several members of MDT present to incorporate areas of expertise.
Potential Modifications to the FRAT[edit | edit source]
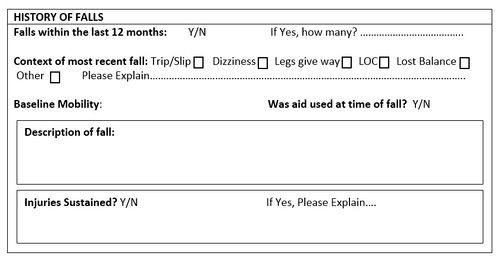
During the process of evaluating the FRAT, there is a perceived lack of depth pertaining to the falls section. It is proposed that some amendments could be made to this in order to improve clarity and increase information and reliability.
Current ‘History of Falls’ Section:
Potential Developments:
References[edit | edit source]
- ↑ WHO Falls Available:https://www.who.int/news-room/fact-sheets/detail/falls (accessed 2.11.2022)
- ↑ Stapleton C, Hough P, Oldmeadow L, Bull K, Hill K, Greenwood K. Four‐item fall risk screening tool for subacute and residential aged care: The first step in fall prevention. Australasian Journal on Ageing. 2009 Sep;28(3):139-43.
- ↑ Purves D, Cabeza R, Huettel SA, LaBar KS, Platt ML, Woldorff MG, Brannon EM. Cognitive neuroscience. Sunderland: Sinauer Associates, Inc; 2008.
- ↑ Herman T, Mirelman A, Giladi N, Schweiger A, Hausdorff JM. Executive control deficits as a prodrome to falls in healthy older adults: a prospective study linking thinking, walking, and falling. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2010 May 19;65(10):1086-92.
- ↑ Muir SW, Gopaul K, Montero Odasso MM. The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age and ageing. 2012 Feb 27;41(3):299-308.
- ↑ Gleason CE, Gangnon RE, Fischer BL, Mahoney JE. Increased risk for falling associated with subtle cognitive impairment: secondary analysis of a randomized clinical trial. Dementia and geriatric cognitive disorders. 2009;27(6):557-63.
- ↑ Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age and ageing. 1972 Nov 1;1(4):233-8.
- ↑ Centre for Clinical Practice at NICE (UK. Falls: Assessment and prevention of falls in older people. 2013.https://www.nice.org.uk/guidance/cg161