Prolonged Labor: Difference between revisions
No edit summary |
No edit summary |
||
| Line 15: | Line 15: | ||
Passenger: The passenger is referred to the fetus travelling down the birth canal. When the fetal head is large in proportion to the mother's pelvis, or not in proper position. In this situation, spontaneous vaginal delivery will be difficult and there will be need for assisted delivery or a caesarean section. | Passenger: The passenger is referred to the fetus travelling down the birth canal. When the fetal head is large in proportion to the mother's pelvis, or not in proper position. In this situation, spontaneous vaginal delivery will be difficult and there will be need for assisted delivery or a caesarean section. | ||
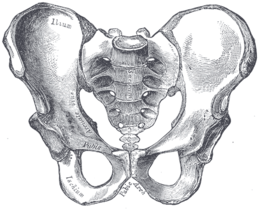
[[File:The pelvis.png|thumb|pelvis]] | |||
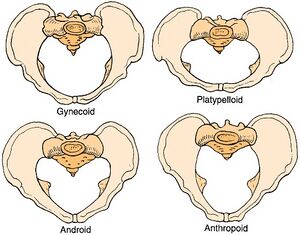
[[Pelvis]] or passage size: The shape and deformity of the pelvis has been implicated in labor dystocia. he female pelvis has four shapes. Caldwell and Moloy grouped the female pelvis into four different types gynoid, android, anthropoid, and platypelloid. Each has peculiar characteristics regarding the width of the sub-pubic angle, the height of the pelvis, the transverse diameters of the three pelvic planes (inlet, mid pelvis, outlet), and the shape of the circumference of the upper pelvic narrow.<ref>SWENSON PC. Anatomical variations in the female pelvis; the Caldwell-Moloy classification. Radiology. 1947 May;48(5):527.</ref> The commonest (50%) and most favorable in Caucasian women is the gynoid it is described to be ovoid in shape and has a round inlet (Anteroposterior diameter of 11 cm and transverse diameter of 13 cm) fetal head to engage and descend through its wide subpubic arch. The second and third pelvic shapes increase the incidence of occipito-posterior positions. Engagement of the fetal head always almost impossible with a platypelloid pelvis.<ref>Asma Gharaibeh, Tahir Mahmood, | [[File:Female-pelvis.jpg|thumb|Types of female pelvis]] | ||
[[Pelvis]] or passage size: The shape and deformity of the pelvis has been implicated in labor dystocia. he female pelvis has four shapes. Caldwell and Moloy grouped the female pelvis into four different types gynoid, android, anthropoid, and platypelloid. Each has peculiar characteristics regarding the width of the sub-pubic angle, the height of the pelvis, the transverse diameters of the three pelvic planes (inlet, mid pelvis, outlet), and the shape of the circumference of the upper pelvic narrow.<ref>SWENSON PC. Anatomical variations in the female pelvis; the Caldwell-Moloy classification. Radiology. 1947 May;48(5):527.</ref> The commonest (50%) and most favorable in Caucasian women is the gynoid it is described to be ovoid in shape and has a round inlet (Anteroposterior diameter of 11 cm and transverse diameter of 13 cm) fetal head to engage and descend through its wide subpubic arch. The second and third pelvic shapes increase the incidence of occipito-posterior positions. Engagement of the fetal head always almost impossible with a platypelloid pelvis.<ref name=":0">Asma Gharaibeh, Tahir Mahmood, | |||
Abnormal labour,Obstetrics, Gynaecology & Reproductive Medicine,Volume 29, Issue 5, | Abnormal labour,Obstetrics, Gynaecology & Reproductive Medicine,Volume 29, Issue 5, | ||
| Line 24: | Line 25: | ||
<nowiki>https://doi.org/10.1016/j.ogrm.2019.02.006</nowiki>.</ref> | <nowiki>https://doi.org/10.1016/j.ogrm.2019.02.006</nowiki>.</ref> | ||
Power (uterine contractility): This refers to the strength of the uterine contractions in the first and second stage of [[Labour|labor]]. The strength of uterine contractions plays an important role in the progress of | Power (uterine contractility): This refers to the strength of the uterine contractions in the first and second stage of [[Labour|labor]]. The strength of uterine contractions plays an important role in the progress of labor. Asma and Tahir stated that in 20% of cases the occiput is posterior at the beginning of labor and with good uterine contractions, in almost 90% of these cases the vertex will rotate to an occipito-anterior position.<ref name=":0" /> During the second stage of labor, more strength are required by the mother to push ineffective maternal pushing efforts in the second stage of [[Labour|labor]] might lead to labor dystocia | ||
=== Definition === | |||
WHO defined labor dystocia as the "onset of regular, rhythmical painful contractions accompanied by cervical dilation where [[Labour|labor]] is longer than 24 hours".<ref>World Health Organization. Education material for teachers of midwifery : midwifery education modules. – 2nd ed. Available from https://cdn.who.int/media/docs/default-source/mca-documents/maternal-nb/midwifery/midwifery-education-module_3_managing-prolonged-and-obstructed-labour.pdf?sfvrsn=51584b42_1&download=true[Accessed 25th November 2022</ref> | |||
==== Diagnosis ==== | |||
It is essential to diagnose labor dystocia early so that prompt interventions can be offered to improve progress of labor and therefore reduce maternal and fetal morbidities that may be caused by LD. The partograph is used in establishing a diagnosis of labor dystocia. Recommended by the World Health Organization,<ref name=":1">World Health Organization. World Health Organization partograph in management of labour. World Health Organization Maternal Health and Safe Motherhood Programme. ''Lancet.'' 1994;343:1399-404.</ref><ref name=":1" /> a partograph (or partogram) is a tool used for monitoring labor wellbeing and progress<ref>Bedwell, C., Levin, K., Pett, C. ''et al.'' A realist review of the partograph: when and how does it work for labour monitoring?. ''BMC Pregnancy Childbirth'' 17, 31 (2017). <nowiki>https://doi.org/10.1186/s12884-016-1213-4</nowiki></ref>can as well be used to prevent<ref>MATHAI, MATTHEWS MD, MObstet, PhD. The Partograph for the Prevention of Obstructed Labor. Clinical Obstetrics and Gynecology: June 2009 - Volume 52 - Issue 2 - p 256-269 | |||
doi: 10.1097/GRF.0b013e3181a4f163 </ref> labor dystocia. | |||
Labor progress is said to be abnormal when the rate of dilatation falls to the right of the projected normal labor curve plotted on the partograph. Delay in the first stage of labor is suspected if there is cervical dilatation of less than 2 cm in 4 h. Delay in the second stage of labor is diagnosed once the stage is more than 2 hours in Nulliparous or less than 1hour per descent in multiparous women. | |||
or | |||
=== Managements of labor dystocia === | |||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 12:23, 26 November 2022
Original Editor - User:Temitope Olowoyeye
Top Contributors - Temitope Olowoyeye, Gold Oluleye, Kim Jackson, Lucinda hampton and Khloud Shreif
Introduction[edit | edit source]
Labor dystocia is a labor complication common in nulliparous women that may disrupt the the process of vaginal delivery making it a major indication for instrumental deliveries or/ and cesarean section (CS).[1] It may increase the risk for maternal and neonatal infection, fetal distress, neonatal hypoxia, uterine rupture, and postpartum hemorrhage it may also increase the risk of maternal pelvic floor and genital trauma.[2]
Labor dystocia(LD) can not be described without describing the process of normal labor process. Normal labor is described as uterine contractions that leads to progressive dilation and effacement of the cervix. Labor dystocia (LD) caused by fetal malposition, inadequate contractions, poor maternal efforts, or true cephalopelvic disproportion.[3] Management of LD can significantly affect the outcome of the delivery process.
Pathophysiology[edit | edit source]
Labor dystocia can be the result of problems with one of the following three P' s:
Passenger: The passenger is referred to the fetus travelling down the birth canal. When the fetal head is large in proportion to the mother's pelvis, or not in proper position. In this situation, spontaneous vaginal delivery will be difficult and there will be need for assisted delivery or a caesarean section.
Pelvis or passage size: The shape and deformity of the pelvis has been implicated in labor dystocia. he female pelvis has four shapes. Caldwell and Moloy grouped the female pelvis into four different types gynoid, android, anthropoid, and platypelloid. Each has peculiar characteristics regarding the width of the sub-pubic angle, the height of the pelvis, the transverse diameters of the three pelvic planes (inlet, mid pelvis, outlet), and the shape of the circumference of the upper pelvic narrow.[4] The commonest (50%) and most favorable in Caucasian women is the gynoid it is described to be ovoid in shape and has a round inlet (Anteroposterior diameter of 11 cm and transverse diameter of 13 cm) fetal head to engage and descend through its wide subpubic arch. The second and third pelvic shapes increase the incidence of occipito-posterior positions. Engagement of the fetal head always almost impossible with a platypelloid pelvis.[5]
Power (uterine contractility): This refers to the strength of the uterine contractions in the first and second stage of labor. The strength of uterine contractions plays an important role in the progress of labor. Asma and Tahir stated that in 20% of cases the occiput is posterior at the beginning of labor and with good uterine contractions, in almost 90% of these cases the vertex will rotate to an occipito-anterior position.[5] During the second stage of labor, more strength are required by the mother to push ineffective maternal pushing efforts in the second stage of labor might lead to labor dystocia
Definition[edit | edit source]
WHO defined labor dystocia as the "onset of regular, rhythmical painful contractions accompanied by cervical dilation where labor is longer than 24 hours".[6]
Diagnosis[edit | edit source]
It is essential to diagnose labor dystocia early so that prompt interventions can be offered to improve progress of labor and therefore reduce maternal and fetal morbidities that may be caused by LD. The partograph is used in establishing a diagnosis of labor dystocia. Recommended by the World Health Organization,[7][7] a partograph (or partogram) is a tool used for monitoring labor wellbeing and progress[8]can as well be used to prevent[9] labor dystocia.
Labor progress is said to be abnormal when the rate of dilatation falls to the right of the projected normal labor curve plotted on the partograph. Delay in the first stage of labor is suspected if there is cervical dilatation of less than 2 cm in 4 h. Delay in the second stage of labor is diagnosed once the stage is more than 2 hours in Nulliparous or less than 1hour per descent in multiparous women.
Managements of labor dystocia[edit | edit source]
References[edit | edit source]
- ↑ (Lowe NK: A Review of factors associated with dystocia and Cesarean section in nulliparous women. J Midwifery womens health. 2007,52(3):216-228, American College of Obstetrics and Gynecology. ACOG practice bulletin number 49, December 2003: dystocia and augmentation of labor. Obstet Gynecol. 2003;102:1445–54.
- ↑ Sheiner E, Levy A, Feinstein U, et al. Risk factors and outcome of failure to progress during the first stage of labor: a population-based study. Acta Obstet Gynecol Scand. 2002 Mar;81(3):222–6. PMID: 11966478.
- ↑ Shields SG, Ratcliffe SD, Fontaine P, Leeman L. Dystocia in nulliparous women. Am Fam Physician. 2007 Jun 1;75(11):1671-8. PMID: 17575657.
- ↑ SWENSON PC. Anatomical variations in the female pelvis; the Caldwell-Moloy classification. Radiology. 1947 May;48(5):527.
- ↑ 5.0 5.1 Asma Gharaibeh, Tahir Mahmood, Abnormal labour,Obstetrics, Gynaecology & Reproductive Medicine,Volume 29, Issue 5, 2019,Pages 129-135,ISSN 1751-7214, https://doi.org/10.1016/j.ogrm.2019.02.006.
- ↑ World Health Organization. Education material for teachers of midwifery : midwifery education modules. – 2nd ed. Available from https://cdn.who.int/media/docs/default-source/mca-documents/maternal-nb/midwifery/midwifery-education-module_3_managing-prolonged-and-obstructed-labour.pdf?sfvrsn=51584b42_1&download=true[Accessed 25th November 2022
- ↑ 7.0 7.1 World Health Organization. World Health Organization partograph in management of labour. World Health Organization Maternal Health and Safe Motherhood Programme. Lancet. 1994;343:1399-404.
- ↑ Bedwell, C., Levin, K., Pett, C. et al. A realist review of the partograph: when and how does it work for labour monitoring?. BMC Pregnancy Childbirth 17, 31 (2017). https://doi.org/10.1186/s12884-016-1213-4
- ↑ MATHAI, MATTHEWS MD, MObstet, PhD. The Partograph for the Prevention of Obstructed Labor. Clinical Obstetrics and Gynecology: June 2009 - Volume 52 - Issue 2 - p 256-269 doi: 10.1097/GRF.0b013e3181a4f163