Musculoskeletal Effects Of Down Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| (103 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
''' | <div class="editorbox"> | ||
'''Original Editors ''' - [[User:Nore Boulpaep|Nore Boulpaep]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Introduction == | |||
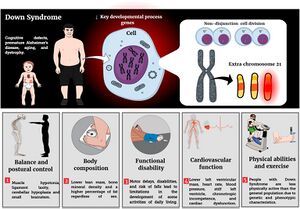
[[Down Syndrome (Trisomy 21)|Down syndrome]] is a chromosomal condition characterised by the presence of an extra copy of genetic material on the 21st chromosome, either in whole (trisomy 21) or part (such as due to translocations).<ref>Roizen NJ, Patterson D. Down's syndrome. The Lancet. 2003 Apr 12;361(9365):1281-9. </ref><ref>Patterson, D (Jul 2009). "Molecular genetic analysis of Down syndrome". ''Human Genetics''. '''126''' (1): 195–214</ref>Factors that are responsible for developmental challenges in children with Down syndrome are hypotonia, ligament laxity, decreased muscle strength, insufficient muscular co-contraction, atlantoaxial instability, balance dysfunction, disturbed proprioception, skeletal deformities(scoliosis, foot deformities), hip and patellar instability.<ref name=":0">Jain, P. D., Nayak, A., Karnad, S. D., & Doctor, K. N. [https://www.e-cep.org/journal/view.php?doi=10.3345/cep.2021.00479 Gross motor dysfunction and balance impairments in children and adolescents with Down syndrome: a systematic review.] Clinical and experimental paediatrics. 2022;65(3):142–149. </ref><ref name=":1">Sheilds, N. [https://www.sciencedirect.com/science/article/pii/S1836955321000965 Physiotherapy management of Down syndrome.] Journal of physiotherapy. 2021;67(4):243–251.</ref> | |||
== Diagnosis == | |||
Down syndrome is diagnosed in two ways, during pregnancy or shortly after birth. The diagnosis is always based on the presence of an extra number 21 chromosome on a karyotype<ref>Wapner RJ, Martin CL, Levy B, Ballif BC, Eng CM, Zachary JM, Savage M, Platt LD, Saltzman D, Grobman WA, Klugman S. Chromosomal microarray versus karyotyping for prenatal diagnosis. New England Journal of Medicine. 2012 Dec 6;367(23):2175-84.</ref>.<ref>Prenatal Screening for Down Syndrome. Available from: http://www.ds-health.com/prenatal.htm (last accessed 17.11.2019)</ref><ref>Skotko B, Bedia RC. Postnatal support for mothers of children with Down syndrome. Mental Retardation. 2005 Jun;43(3):196-212.</ref> In the postnatal period, diagnosis is also indicated by physical features such as epicanthic folds, depressed nasal bridge, abundant neck skin, macroglossia, hypotonia, and single palmar crease. In addition to delayed milestones, intellectual disability also becomes evident in early childhood<ref>Stanislavsky A, Alwalid O, Fahrenhorst-Jones T, et al. [https://radiopaedia.org/articles/down-syndrome Down syndrome.] (Accessed on 19 Nov 2023) [Internet]. Radiopaedia.org. 2011 [cited 2022 Nov 19]. </ref>. | |||
[[File:Fphys-13-948439-g001.jpg|center|thumb|Down syndrome]] | |||
== Prevalence of Musculoskeletal Disorders in Down Syndrome == | |||
* Thoracotomy aims to treat congenital heart disease and the incidence of scoliosis increases from 2% in children to 7% in adolescents and young adults. | |||
* 1-7% and 1-4% hip and patellar instability occur due to bony anomalies. | |||
* Flat feet are 76%common in individuals with Down syndrome. According to recent studies, shorter and wider feet make shoe fitting difficult<ref name=":1" />. | |||
< | == Effects on the Musculoskeletal System == | ||
Inadequate co-contraction of flexor and extensor muscle lead to balance impairments and the development of inefficient compensatory strategies<ref>Jain, Preyal D, Nayak, Akshatha, Karnad, Shreekanth D Doctor, Kaiorisa N. [https://www.e-cep.org/journal/view.php?doi=10.3345/cep.2021.00479 Gross motor dysfunction and balance impairments in children and adolescents with Down syndrome: a systematic review.] Clinical and Experimental Pediatrics. 2021 Jun;65(3):142–149.</ref>. | |||
{| class="wikitable" | |||
|+Compensatory Strategies | |||
!Static Balance | |||
!Dynamic Balance | |||
|- | |||
|Wider step width | |||
|Increase reaction time | |||
|- | |||
|Increase in sway in the medial-lateral and anterior-posterior direction. | |||
|Increase sway in the medial-lateral direction | |||
decrease sway in the anterior-posterior direction(stiffening of trunk) | |||
|} | |||
== Down syndrome in | === Delayed milestones === | ||
[[Down Syndrome Developmental Milestones and Physical Activity|Delayed milestones]] are observed in children with Down syndrome, they are slow in learning to roll/ turn over, sit, stand, walk or do other activities. At a later stage, the child will reach the same basic gross motor skills as those without Down syndrome that are necessary for activities of daily living.<ref>[[Down Syndrome Developmental Milestones and Physical Activity]]</ref> | |||
=== Reduced Muscle Strength === | |||
Bone mass and bone geometry are influenced by growth and muscle development in children and adolescents. This process is further modified by hormonal signals. | |||
Motor function in individuals with Down syndrome is characterised by hypotonia<ref>Frith, U., & Frith, C. D. (1974). ''SPECIFIC MOTOR DISABILITIES IN DOWNS SYNDROME. Journal of Child Psychology and Psychiatry, 15(4), 293–301''</ref>and hyperflexibility, which results in an increased risk of joint dislocation and retarded motor skills. | |||
Hypotonia, decreased muscle tone, has a negative effect on the proprioceptive feedback from muscle and joint sensory structures and can have a detrimental effect on the efficiency of co - contractions and postural reactions. | |||
The | People with Down syndrome have hyperflexibility and more joint mobility than the average. The increased joint mobility may contribute to the lack of posture control. Together with the failure of co-contraction, it can have a negative impact on joint stability. This joint laxity is found in several parts of the body<ref>Down Syndrome: Health Issues. Available from: http://www.ds-health.com/ortho.htm (last accessed 17.11.2019)</ref>due to the abnormal collagen found in Down syndrome. <u></u> | ||
=== Vitamin D Deficiency === | |||
There is a damaging effect of vitamin D insufficiency on musculoskeletal health in children and adolescents during the critical time of bone-mass accrual.<ref>Del Arco C, Riancho JA, Luzuriaga C, Gonzalez‐Macias J, Florez J. Vitamin D status in children with Down's syndrome. Journal of Intellectual Disability Research. 1992 Jun;36(3):251-7.</ref> Vitamin D is not only essential for the normal growth of children but also for the preservation of the bones. Vitamin D is also important for other functions such as muscle tone, immune defence and even cancer. | |||
Vitamin D, per oral absorbed through food or created under the influence of sunlight, is a precursor of the hormone 1,25 – dihydroxy vitamin D. The latter stimulates the small intestine absorption and kidney reabsorption of calcium and thus ensures a better bone. | |||
In patients with Down syndrome, risk factors, such as inadequate exposure to sun, inadequate vitamin D intake and malabsorption or increased breakdown of vitamin D that accompanies anticonvulsant therapy, contribute to vitamin D insufficiency. Down syndrome patients usually have osteoporosis and fractures as a result of this deficiency. | |||
== | === Kirner deformity === | ||
A mild deformity at birth, in which curvature of the distal phalanx of the 5th digit in both a volar and radial direction is characterised, some may present with swelling and erythema. It presents in late childhood to early adolescence and can be managed by splinting, stretching and osteotomy of the deformed distal phalanx.<ref>Sargent M, Bell D, Gaillard F, et al. [https://radiopaedia.org/articles/Kirner deformity. Kirner deformity.] [Internet]. Radiopaedia.org. 2009 [cited 2023 Nov 18]. </ref> | |||
=== Bone Mass === | |||
The accrual of bone mass during childhood is a key determinant of bone health in adulthood, and a low peak skeletal mass is considered an important risk factor for osteoporosis in adult life. | |||
Multivariate analysis showed that Down syndrome was associated with low Bone mineral density (BMD) of the spine. Lack of physical exercise, low muscle strength, insufficient exposure to the sun, low levels of vitamin D and prolonged use of anticonvulsants are all additional risk factors for low BMD. | |||
Some experts hypothesise that the extra copy of chromosome 21 could be responsible for the short stature, skeletal abnormalities and early ageing that are seen in patients with Down syndrome.<ref>McKelvey KD, Fowler TW, Akel NS, Kelsay JA, Gaddy D, Wenger GR, Suva LJ. Low bone turnover and low bone density in a cohort of adults with Down syndrome. Osteoporosis International. 2013 Apr 1;24(4):1333-8.</ref><ref>Hawli Y, Nasrallah M, Fuleihan GE. Endocrine and musculoskeletal abnormalities in patients with Down syndrome. Nature Reviews Endocrinology. 2009 Jun;5(6):327. </ref> | |||
=== Gait Problems === | |||
Children with Down syndrome typically learn to walk with their feet wide apart, their knees stiff and their feet turned out. They do so because hypotonia, ligamentous laxity and weakness make their legs less stable. Physiotherapy should start with teaching the child with Down syndrome the proper standing posture when he is still very young. So, feet positioned under the hips and pointing straight ahead with a slight bend in the knees. With appropriate physiotherapy, gait problems can be minimised or avoided.<ref>Winders, PC. The goal and Opportunity of Physical Therapy for Children with Down Syndrome, 2001. </ref> | |||
{{#ev:youtube |OeSUSECYnIQ}} <ref>https://www.youtube.com/watch?v=OeSUSECYnIQ</ref> | |||
< | === Pelvis === | ||
The Outward flaring of iliac wings known as the "Mickey Mouse pelvis"<ref name=":2">Lall N,. [https://radiopaedia.org/cases/down-syndrome-mickey-mouse-pelvis-1?lang=us Down syndrome - “mickey mouse” pelvis.] Case study, [Internet]. Radiopaedia.org. 2016 [cited 2023 Nov 18]. </ref>, they learn to sit with posterior pelvic tilt. Physiotherapy can help DS children to develop proper posture and gait patterns. | |||
=== Posture === | |||
Children with Down syndrome typically learn to sit with a posterior pelvic tilt, the trunk rounded and the head resting back on the shoulders. Physiotherapy must teach the child the proper sitting posture by providing support at the proper level even before the child can sit independently. Appropriate physical therapy can minimise problems with trunk posture. | |||
== | === Balance === | ||
It is common for children with DS to be delayed in reaching common milestones such as sitting independently, standing and walking. One of the contributing factors to the delay of these specific milestones is poor balance. It is well known that persons with DS are often considered floppy, clumsy, uncoordinated and have awkward movement patterns due to balance issues. These balance challenges often follow the child into the teen years and sometimes into adulthood <ref>Malak R, Kostiukow A, Wasielewska A, Mojs E, Samborski W. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4500597/ Delays in motor development in children with Down syndrome.] Medical Science Monitor 2015;21:1904-1910. (last accessed18 March 2018).</ref> | |||
{{#ev:youtube|https://www.youtube.com/watch?v=4JP1epzbZqc|width}}<ref>[https://www.youtube.com/watch?v=4JP1epzbZqc ExtrachromieVeda Balance exercises, Core Strengthening] | Veda at therapy | Down Syndrome India Available from: https://www.youtube.com/watch?v=4JP1epzbZqc (last accessed 16.11.2019)</ref> | |||
< | === Atlantoaxial Instability === | ||
Neck pain, spasticity, gait difficulties and hyperreflexia may indicate atlantoaxial subluxation. Misalignment of the first and second vertebrae occurs in 1-2% of children with Down syndrome. Cervical radiography is recommended and participation in sports should be restricted, as it increases the risk of spinal cord injury.<ref>Antonarakis, S. E., Skotko, B. G., Rafii, M. S., Strydom, A., Pape, S. E., Bianchi, D. W., Sherman, S. L., & Reeves, R. H. . [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8428796/ Down syndrome]. Nature Reviews Disease Primers,. 2020;6(1):9. </ref> | |||
< | == Quality of life == | ||
Moderate to favourable QOL has been observed in individuals with Down syndrome and is affected by a variety of factors. Resolving musculoskeletal disorders, use of orthotics or assistive devices and inclusive physical activities (sports/ recreational activities) can improve social and emotional well-being. It is significant to provide education and support to individuals with Down syndrome, their families, and caregivers. Early intervention and holistic approach is crucial to improve quality of life<ref>Lee, A, Knafl, G, Knafl, K, Van Riper, M. [https://pubmed.ncbi.nlm.nih.gov/32997835/ Quality of life in individuals with Down syndrome aged 4 to 21 years.] Child Care Health Dev. 2021;47:85–93. </ref>. | |||
== | == Evidence for Physiotherapy Intervention == | ||
Without physical therapy, a child with Down syndrome could end up having postural, gait and orthopaedic problems later in life from using their muscles incorrectly. They also are at greater risk of joint problems if muscles are not strengthened. The importance of early intervention should be emphasised. | |||
One of the major goals of physiotherapy is to minimise the development of the compensatory movement patterns that children with Down syndrome are prone to develop. Working with their muscles and movements will help children reach some of their motor milestones and will prevent them from developing problems, such as bad trunk posture and gait problems. treatment aims to assist people to live as independently as possible <ref>CSP. What is physiotherapy? 2018. www.csp.org.uk/your-health/what-physiotherapy (last accessed 14 April 2018).</ref>Physiotherapy at an early age strengthens the muscles, enabling children with Down syndrome to keep their bodies in proper alignment and prevent future health problems<ref>Early Intervention Support Available from: http://www.earlyinterventionsupport.com/diagnosis/List/Down-Syndrome.aspx (last accessed November 29, 2011) </ref> | |||
< | An example of a '''training programme'''<ref>Shields N, Taylor NF, Dodd KJ. Effects of a community-based progressive resistance training program on muscle performance and physical function in adults with Down syndrome: a randomized controlled trial. Archives of physical medicine and rehabilitation. 2008 Jul 1;89(7):1215-20.</ref> titled "Effects of a community – based progressive resistance training programme on muscle performance and physical function in adults with Down syndrome: a randomised controlled trial, 2008" aimed to improve muscle strength with progressive resistance training. In conclusion, the trial concluded that progressive resistance training is a safe and feasible fitness option that can improve upper-limb muscle endurance in adults with Down syndrome. | ||
Various other studies illustrate also positive effects on motor skills. | |||
== References == | == References == | ||
<references /> | |||
[[Category:Paediatrics]] | |||
<references /> | [[Category:Paediatrics - Conditions]] | ||
[[Category:Down Syndrome - Trisomy 21]] | |||
[[Category: | |||
Latest revision as of 14:13, 2 February 2024
Original Editors - Nore Boulpaep
Top Contributors - Nore Boulpaep, Memoona Awan, Lucinda hampton, Kim Jackson, Admin, Naomi O'Reilly and Meaghan Rieke
Introduction[edit | edit source]
Down syndrome is a chromosomal condition characterised by the presence of an extra copy of genetic material on the 21st chromosome, either in whole (trisomy 21) or part (such as due to translocations).[1][2]Factors that are responsible for developmental challenges in children with Down syndrome are hypotonia, ligament laxity, decreased muscle strength, insufficient muscular co-contraction, atlantoaxial instability, balance dysfunction, disturbed proprioception, skeletal deformities(scoliosis, foot deformities), hip and patellar instability.[3][4]
Diagnosis[edit | edit source]
Down syndrome is diagnosed in two ways, during pregnancy or shortly after birth. The diagnosis is always based on the presence of an extra number 21 chromosome on a karyotype[5].[6][7] In the postnatal period, diagnosis is also indicated by physical features such as epicanthic folds, depressed nasal bridge, abundant neck skin, macroglossia, hypotonia, and single palmar crease. In addition to delayed milestones, intellectual disability also becomes evident in early childhood[8].
Prevalence of Musculoskeletal Disorders in Down Syndrome[edit | edit source]
- Thoracotomy aims to treat congenital heart disease and the incidence of scoliosis increases from 2% in children to 7% in adolescents and young adults.
- 1-7% and 1-4% hip and patellar instability occur due to bony anomalies.
- Flat feet are 76%common in individuals with Down syndrome. According to recent studies, shorter and wider feet make shoe fitting difficult[4].
Effects on the Musculoskeletal System[edit | edit source]
Inadequate co-contraction of flexor and extensor muscle lead to balance impairments and the development of inefficient compensatory strategies[9].
| Static Balance | Dynamic Balance |
|---|---|
| Wider step width | Increase reaction time |
| Increase in sway in the medial-lateral and anterior-posterior direction. | Increase sway in the medial-lateral direction
decrease sway in the anterior-posterior direction(stiffening of trunk) |
Delayed milestones[edit | edit source]
Delayed milestones are observed in children with Down syndrome, they are slow in learning to roll/ turn over, sit, stand, walk or do other activities. At a later stage, the child will reach the same basic gross motor skills as those without Down syndrome that are necessary for activities of daily living.[10]
Reduced Muscle Strength[edit | edit source]
Bone mass and bone geometry are influenced by growth and muscle development in children and adolescents. This process is further modified by hormonal signals.
Motor function in individuals with Down syndrome is characterised by hypotonia[11]and hyperflexibility, which results in an increased risk of joint dislocation and retarded motor skills.
Hypotonia, decreased muscle tone, has a negative effect on the proprioceptive feedback from muscle and joint sensory structures and can have a detrimental effect on the efficiency of co - contractions and postural reactions.
People with Down syndrome have hyperflexibility and more joint mobility than the average. The increased joint mobility may contribute to the lack of posture control. Together with the failure of co-contraction, it can have a negative impact on joint stability. This joint laxity is found in several parts of the body[12]due to the abnormal collagen found in Down syndrome.
Vitamin D Deficiency[edit | edit source]
There is a damaging effect of vitamin D insufficiency on musculoskeletal health in children and adolescents during the critical time of bone-mass accrual.[13] Vitamin D is not only essential for the normal growth of children but also for the preservation of the bones. Vitamin D is also important for other functions such as muscle tone, immune defence and even cancer.
Vitamin D, per oral absorbed through food or created under the influence of sunlight, is a precursor of the hormone 1,25 – dihydroxy vitamin D. The latter stimulates the small intestine absorption and kidney reabsorption of calcium and thus ensures a better bone.
In patients with Down syndrome, risk factors, such as inadequate exposure to sun, inadequate vitamin D intake and malabsorption or increased breakdown of vitamin D that accompanies anticonvulsant therapy, contribute to vitamin D insufficiency. Down syndrome patients usually have osteoporosis and fractures as a result of this deficiency.
Kirner deformity[edit | edit source]
A mild deformity at birth, in which curvature of the distal phalanx of the 5th digit in both a volar and radial direction is characterised, some may present with swelling and erythema. It presents in late childhood to early adolescence and can be managed by splinting, stretching and osteotomy of the deformed distal phalanx.[14]
Bone Mass[edit | edit source]
The accrual of bone mass during childhood is a key determinant of bone health in adulthood, and a low peak skeletal mass is considered an important risk factor for osteoporosis in adult life.
Multivariate analysis showed that Down syndrome was associated with low Bone mineral density (BMD) of the spine. Lack of physical exercise, low muscle strength, insufficient exposure to the sun, low levels of vitamin D and prolonged use of anticonvulsants are all additional risk factors for low BMD.
Some experts hypothesise that the extra copy of chromosome 21 could be responsible for the short stature, skeletal abnormalities and early ageing that are seen in patients with Down syndrome.[15][16]
Gait Problems[edit | edit source]
Children with Down syndrome typically learn to walk with their feet wide apart, their knees stiff and their feet turned out. They do so because hypotonia, ligamentous laxity and weakness make their legs less stable. Physiotherapy should start with teaching the child with Down syndrome the proper standing posture when he is still very young. So, feet positioned under the hips and pointing straight ahead with a slight bend in the knees. With appropriate physiotherapy, gait problems can be minimised or avoided.[17]
Pelvis[edit | edit source]
The Outward flaring of iliac wings known as the "Mickey Mouse pelvis"[19], they learn to sit with posterior pelvic tilt. Physiotherapy can help DS children to develop proper posture and gait patterns.
Posture[edit | edit source]
Children with Down syndrome typically learn to sit with a posterior pelvic tilt, the trunk rounded and the head resting back on the shoulders. Physiotherapy must teach the child the proper sitting posture by providing support at the proper level even before the child can sit independently. Appropriate physical therapy can minimise problems with trunk posture.
Balance[edit | edit source]
It is common for children with DS to be delayed in reaching common milestones such as sitting independently, standing and walking. One of the contributing factors to the delay of these specific milestones is poor balance. It is well known that persons with DS are often considered floppy, clumsy, uncoordinated and have awkward movement patterns due to balance issues. These balance challenges often follow the child into the teen years and sometimes into adulthood [20]
Atlantoaxial Instability[edit | edit source]
Neck pain, spasticity, gait difficulties and hyperreflexia may indicate atlantoaxial subluxation. Misalignment of the first and second vertebrae occurs in 1-2% of children with Down syndrome. Cervical radiography is recommended and participation in sports should be restricted, as it increases the risk of spinal cord injury.[22]
Quality of life[edit | edit source]
Moderate to favourable QOL has been observed in individuals with Down syndrome and is affected by a variety of factors. Resolving musculoskeletal disorders, use of orthotics or assistive devices and inclusive physical activities (sports/ recreational activities) can improve social and emotional well-being. It is significant to provide education and support to individuals with Down syndrome, their families, and caregivers. Early intervention and holistic approach is crucial to improve quality of life[23].
Evidence for Physiotherapy Intervention[edit | edit source]
Without physical therapy, a child with Down syndrome could end up having postural, gait and orthopaedic problems later in life from using their muscles incorrectly. They also are at greater risk of joint problems if muscles are not strengthened. The importance of early intervention should be emphasised.
One of the major goals of physiotherapy is to minimise the development of the compensatory movement patterns that children with Down syndrome are prone to develop. Working with their muscles and movements will help children reach some of their motor milestones and will prevent them from developing problems, such as bad trunk posture and gait problems. treatment aims to assist people to live as independently as possible [24]Physiotherapy at an early age strengthens the muscles, enabling children with Down syndrome to keep their bodies in proper alignment and prevent future health problems[25]
An example of a training programme[26] titled "Effects of a community – based progressive resistance training programme on muscle performance and physical function in adults with Down syndrome: a randomised controlled trial, 2008" aimed to improve muscle strength with progressive resistance training. In conclusion, the trial concluded that progressive resistance training is a safe and feasible fitness option that can improve upper-limb muscle endurance in adults with Down syndrome.
Various other studies illustrate also positive effects on motor skills.
References[edit | edit source]
- ↑ Roizen NJ, Patterson D. Down's syndrome. The Lancet. 2003 Apr 12;361(9365):1281-9.
- ↑ Patterson, D (Jul 2009). "Molecular genetic analysis of Down syndrome". Human Genetics. 126 (1): 195–214
- ↑ Jain, P. D., Nayak, A., Karnad, S. D., & Doctor, K. N. Gross motor dysfunction and balance impairments in children and adolescents with Down syndrome: a systematic review. Clinical and experimental paediatrics. 2022;65(3):142–149.
- ↑ 4.0 4.1 Sheilds, N. Physiotherapy management of Down syndrome. Journal of physiotherapy. 2021;67(4):243–251.
- ↑ Wapner RJ, Martin CL, Levy B, Ballif BC, Eng CM, Zachary JM, Savage M, Platt LD, Saltzman D, Grobman WA, Klugman S. Chromosomal microarray versus karyotyping for prenatal diagnosis. New England Journal of Medicine. 2012 Dec 6;367(23):2175-84.
- ↑ Prenatal Screening for Down Syndrome. Available from: http://www.ds-health.com/prenatal.htm (last accessed 17.11.2019)
- ↑ Skotko B, Bedia RC. Postnatal support for mothers of children with Down syndrome. Mental Retardation. 2005 Jun;43(3):196-212.
- ↑ Stanislavsky A, Alwalid O, Fahrenhorst-Jones T, et al. Down syndrome. (Accessed on 19 Nov 2023) [Internet]. Radiopaedia.org. 2011 [cited 2022 Nov 19].
- ↑ Jain, Preyal D, Nayak, Akshatha, Karnad, Shreekanth D Doctor, Kaiorisa N. Gross motor dysfunction and balance impairments in children and adolescents with Down syndrome: a systematic review. Clinical and Experimental Pediatrics. 2021 Jun;65(3):142–149.
- ↑ Down Syndrome Developmental Milestones and Physical Activity
- ↑ Frith, U., & Frith, C. D. (1974). SPECIFIC MOTOR DISABILITIES IN DOWNS SYNDROME. Journal of Child Psychology and Psychiatry, 15(4), 293–301
- ↑ Down Syndrome: Health Issues. Available from: http://www.ds-health.com/ortho.htm (last accessed 17.11.2019)
- ↑ Del Arco C, Riancho JA, Luzuriaga C, Gonzalez‐Macias J, Florez J. Vitamin D status in children with Down's syndrome. Journal of Intellectual Disability Research. 1992 Jun;36(3):251-7.
- ↑ Sargent M, Bell D, Gaillard F, et al. Kirner deformity. [Internet]. Radiopaedia.org. 2009 [cited 2023 Nov 18].
- ↑ McKelvey KD, Fowler TW, Akel NS, Kelsay JA, Gaddy D, Wenger GR, Suva LJ. Low bone turnover and low bone density in a cohort of adults with Down syndrome. Osteoporosis International. 2013 Apr 1;24(4):1333-8.
- ↑ Hawli Y, Nasrallah M, Fuleihan GE. Endocrine and musculoskeletal abnormalities in patients with Down syndrome. Nature Reviews Endocrinology. 2009 Jun;5(6):327.
- ↑ Winders, PC. The goal and Opportunity of Physical Therapy for Children with Down Syndrome, 2001.
- ↑ https://www.youtube.com/watch?v=OeSUSECYnIQ
- ↑ Lall N,. Down syndrome - “mickey mouse” pelvis. Case study, [Internet]. Radiopaedia.org. 2016 [cited 2023 Nov 18].
- ↑ Malak R, Kostiukow A, Wasielewska A, Mojs E, Samborski W. Delays in motor development in children with Down syndrome. Medical Science Monitor 2015;21:1904-1910. (last accessed18 March 2018).
- ↑ ExtrachromieVeda Balance exercises, Core Strengthening | Veda at therapy | Down Syndrome India Available from: https://www.youtube.com/watch?v=4JP1epzbZqc (last accessed 16.11.2019)
- ↑ Antonarakis, S. E., Skotko, B. G., Rafii, M. S., Strydom, A., Pape, S. E., Bianchi, D. W., Sherman, S. L., & Reeves, R. H. . Down syndrome. Nature Reviews Disease Primers,. 2020;6(1):9.
- ↑ Lee, A, Knafl, G, Knafl, K, Van Riper, M. Quality of life in individuals with Down syndrome aged 4 to 21 years. Child Care Health Dev. 2021;47:85–93.
- ↑ CSP. What is physiotherapy? 2018. www.csp.org.uk/your-health/what-physiotherapy (last accessed 14 April 2018).
- ↑ Early Intervention Support Available from: http://www.earlyinterventionsupport.com/diagnosis/List/Down-Syndrome.aspx (last accessed November 29, 2011)
- ↑ Shields N, Taylor NF, Dodd KJ. Effects of a community-based progressive resistance training program on muscle performance and physical function in adults with Down syndrome: a randomized controlled trial. Archives of physical medicine and rehabilitation. 2008 Jul 1;89(7):1215-20.