Pelvic Floor Dysfunction: Difference between revisions
(Add in overview) |
Amy McCarthy (talk | contribs) No edit summary |
||
| Line 67: | Line 67: | ||
[http://www.pelvicfloorfirst.org.au/pages/how-can-i-tellif-i-have-a-pelvic-floor-problem.html] | [http://www.pelvicfloorfirst.org.au/pages/how-can-i-tellif-i-have-a-pelvic-floor-problem.html] | ||
== | == Risk Factors == | ||
== Common misconeptions == | |||
'''It’s my fault isn’t it? (smith et al. 2007)''' | |||
* woman normalize symptoms – feel that it is part of being a woman and getting older especially after childbirth (mason et al 2001) | |||
* lack of self control- woman feel is it their own fault for not being able to control bladder | |||
* Woman experiencing POP and associated symptoms such as incontinence feel “deserving”, due to lack of consistency or failure to complete PFMT post childbirth. Woman, blame themselves for having these symptoms. | |||
* Lack of priority given to PFMT post childbirth due to occupation with new baby , lack of perineal sensitivity post delivery have left PFMT low on the priority list. Woman experience self blame for allowing his to occur | |||
* Shame associated with incontinence issues - woman are less willing to seek help from health care professionals as they feel they will be judged reprimanded or blamed for lack of consistency in PFMT | |||
* Lack of understanding – woman have revealed that lack of understanding about PFMT , such as how to actually do a PFM contraction has prevented them from PFMT effectively . Difficulty discussing this issue with healthcare professionals due to the sensitive nature of area. | |||
'''The silent private exercise (Neels et al. 2017)''' | |||
* The internal unseen nature of the PFM has led to difficulty for many woman understanding how to train the PFM | |||
* The mysterious nature of the PFMT seems in part due to the difficulty of finding appropriate yet explicit language to explain PFM exercises | |||
* Exercise using muscles that cannot be seen and are located in a private area of the body and are associated with private function not easily discussed | |||
* Study conducted to evaluate health care professionals skills in explaining the PFM contraction- patient described explanation as “sketchy “ | |||
* Woman feel silly as they may struggle to grasp technique | |||
* ERRORS – common errors made in an attempt to contract pelvic floor muscles .'''COMMOV-''' contraction of other muscles ( using rectus abdominus, glutes and adductors ) MOV- pelvic tilts , breath holding and straining performed in addition to or instead of an actual pelvic floor muscle contraction | |||
* 57% of woman show '''Commov''' when assessing technique. | |||
'''Will pelvic floor muscle training work? (Neels et al. 2018)''' | |||
* Lack of understanding – Lack of clarity, as to why PFM should be exercised . Woman are unsure as to why these exercises need to be done. Due to the lack of understanding , woman are unable to make informed decision to partake in PFMT | |||
* Waste of time- Woman may find it difficult to continue with PFMT in the absence of noticeable benefit. No immediate effect from training leads woman to feel as though there is no return for their efforts and that PFMT is waste of time | |||
* The nature of PFMT – woman have described PFM exercises as tedious, a daily battle, a nuisance and boring | |||
* Timing? This study conducted found that woman feel the PFMT is difficult to factor into their daily schedule. Due to the personal nature of the exercise need to be done alone and in a quiet place for concentration also many feel embarrassed to do exercises around others | |||
'''Prolapse and incontinence, it’s a female problem right?(Hirschhorn et al. 2013)''' | |||
* Study investigated male perceptions of incontinence and pelvic floor muscle training – 66% of men were unaware that males were required to do PFMT | |||
* Widely perceived as a female issue | |||
* Stigma and embarrassment – leads to under reporting of symptoms within the male population | |||
* Lack of research regarding male experiences in PFMT , body of research lies within the female population | |||
Add your content to this page here! | Add your content to this page here! | ||
== Treatment == | == Treatment == | ||
| Line 87: | Line 123: | ||
see [[Adding References|adding references tutorial]]. | see [[Adding References|adding references tutorial]]. | ||
<references /> | <references />6.HAY-SMITH, E., RYAN, K. and DEAN, S., 2007. The silent, private exercise: experiences of pelvic floor muscle training in a sample of women with stress urinary incontinence. ''Physiotherapy.'' vol. 93, no. 1, pp. 53-61. | ||
7.HIRSCHHORN, A.D., KOLT, G.S. and BROOKS, A.J., 2013. Barriers and enablers to the provision and receipt of preoperative pelvic floor muscle training for men having radical prostatectomy: a qualitative study. ''BMC Health Services Research.'' vol. 13, no. 1, pp. 305. | |||
8.MASON, L., GLENN, S., WALTON, I. and HUGHES, C., 2001. The instruction in pelvic floor exercises provided to women during pregnancy or following delivery. ''Midwifery.'' 2001, vol. 17, no. 1, pp. 55-64. | |||
9.NEELS, H., DE WACHTER, S., WYNDAELE, J., VAN AGGELPOEL, T. and VERMANDEL, A., 2018. Common errors made in attempt to contract the pelvic floor muscles in women early after delivery: A prospective observational study. ''European Journal of Obstetrics, Gynecology, and Reproductive Biology.'' 01, vol. 220, pp. 113-117. | |||
[[Category:Queen_Margaret_University_Project]] [[Category:Projects]] | [[Category:Queen_Margaret_University_Project]] [[Category:Projects]] | ||
Revision as of 19:56, 19 March 2018
Original Editors - Sarah Barnes, Chris Van Wyk, Amy McCarthy, Gina Mclaughlin, John Lavin, Claire Ramsden and Carolinne Cieslak.
Top Contributors - Sarah Barnes, Carolinne Cieslak, Gina McLoughlin, Kim Jackson, Claire Ramsden, Chris Van Wyk, Amy McCarthy, John Lavin, Vidya Acharya, Rachael Lowe and Nicole Hills
Learning Outcomes[edit | edit source]
Add your content to this page here!
Overview[edit | edit source]
Ted Ex Talk [1]
What is the Pelvic Floor?
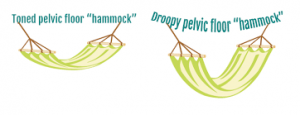
The pelvic floor is made up of a layer of muscles spanning the bottom of the pelvis that support our internal pelvic organs (bladder and bowel in males [1] and bladder, bowel and uterus/womb in women). These muscles run like a hammock front to back from the pubic bone to the tailbone and side-to-side from one sitting bone to the other [2].
These muscles are similar to a trampoline, as they have the ability to move up and down. This occurs during breathing as when we inhale theme shaped diaphragm pulls down to open our lungs. This pushes down of our internal organs. To avoid squashing these organs our pelvic floor and abdominal muscle relax and create more space for the organs to move down. When we exhale the diaphragm springs back to its normal position and as it does so the abdominals and pelvic floor muscles return to their resting position. A common problem experienced by people is holding their breath during lifting activities or bowel movements, which can lead to pelvic floor dysfunctions by adding excess stress on these muscles.[3]
Our pelvic organs sit on top of this layer of muscle. The muscles also have holes through which the urethra and anus pass through in males and urethra, anus and vagina pass through in females. The muscles are snug against these structures in order to hold the passages closed. Both the anus and urethra have extra circular muscles (called sphincters) that help to keep the passages closed and prevent leakage.[4]
Pelvic floor muscles may be hidden but we do have voluntary control of them and therefore they can be trained like muscles in our arms or legs.
Functions of the pelvic floor muscles:
- Support internal pelvic organs in the correct positions (Bladder, bowel and vagina)
- Allow conscious control of bladder and bowel habits using the sphincter muscles. This allows us to control the release of urine, faeces and gas and to delay emptying until a convenient time. This works as the pelvic floor muscles contract the organs are lifted up and the sphincter tighten around the openings of the urethra and anus.
- Allow the passage of urine and faeces out of the body due to the pelvic floor muscles relaxing and allowing the passages to open.
- Sexual function
- In males the pelvic floor muscles are important in erectile function by increasing rigidity and ejaculation by improving control and coordination between circulation, pelvic floor muscles.[5]
- In females voluntary contraction of the pelvic floor muscles can contribute to sexual sensation
- Additionally in pregnant women the pelvic floor offers support to the foetus during pregnancy and also assists in the childbirth process.
Strong pelvic floor muscles are important when we cough, laugh, sneeze or during lifting activities as there is extra force added to the abdomen and therefore additional pressure down onto the pelvic floor. If these muscles are weak, stretched or not working as they should, pressure may be felt in the pelvic region or some urinary or faecal leaking may occur during these activities.
Signs and Symptoms[edit | edit source]
Men:[edit | edit source]
- Constipation or bowel strains
- Ongoing pain in your pelvic region, genitals or rectum.
- A prolapse – may feel as though there is a bulge/ pressure in the rectum or a feeling of needing to use your bowels without actually needing to go. - Accidentally leaking urine when you exercise, laugh, cough or sneeze.
- Feelings of urgency in needing to the bathroom, or not making it there in time.
- Frequent need to urinate.
- Difficultly emptying your bladder (discontinuous urination – stop and start multiple times) and bowels.
- The feeling of needing to have several bowel movements during a short period of time.
- Accidentally passing wind.
- Pain in your lower back that cannot be explained by other causes.
- Pain in the testicles, penis (referred pain from the pelvic floor) or pelvis during intercourse.
- Erectile dysfunction.
- Painful ejaculation.
For further information on the male pelvic floor go to: [2]
Women:[edit | edit source]
- Pain or numbness during intercourse.
- Ongoing pain in your pelvic region, genitals or rectum.
- A prolapse – may be felt as a bulge in the vagina (feeling or seeing a bulge or lump in or coming out of your vagina) or a feeling of heaviness, discomfort, pulling, dragging or dropping sensation.
- Accidentally leaking urine when you exercise, laugh, cough or sneeze (stress incontinence).
- Feelings of urgency in needing to the bathroom, or not making it there in time.
- Frequent need to urinate.
- Difficultly emptying your bladder (discontinuous urination – stop and start multiple times) and bowels.
- The feeling of needing to have several bowel movements during a short period of time.
- Constipation or bowel strains.
- Accidentally passing wind.
- Pain in your lower back that cannot be explained by other causes.
Helpful websites for further information: [3] [4]
Risk Factors[edit | edit source]
Common misconeptions[edit | edit source]
It’s my fault isn’t it? (smith et al. 2007)
- woman normalize symptoms – feel that it is part of being a woman and getting older especially after childbirth (mason et al 2001)
- lack of self control- woman feel is it their own fault for not being able to control bladder
- Woman experiencing POP and associated symptoms such as incontinence feel “deserving”, due to lack of consistency or failure to complete PFMT post childbirth. Woman, blame themselves for having these symptoms.
- Lack of priority given to PFMT post childbirth due to occupation with new baby , lack of perineal sensitivity post delivery have left PFMT low on the priority list. Woman experience self blame for allowing his to occur
- Shame associated with incontinence issues - woman are less willing to seek help from health care professionals as they feel they will be judged reprimanded or blamed for lack of consistency in PFMT
- Lack of understanding – woman have revealed that lack of understanding about PFMT , such as how to actually do a PFM contraction has prevented them from PFMT effectively . Difficulty discussing this issue with healthcare professionals due to the sensitive nature of area.
The silent private exercise (Neels et al. 2017)
- The internal unseen nature of the PFM has led to difficulty for many woman understanding how to train the PFM
- The mysterious nature of the PFMT seems in part due to the difficulty of finding appropriate yet explicit language to explain PFM exercises
- Exercise using muscles that cannot be seen and are located in a private area of the body and are associated with private function not easily discussed
- Study conducted to evaluate health care professionals skills in explaining the PFM contraction- patient described explanation as “sketchy “
- Woman feel silly as they may struggle to grasp technique
- ERRORS – common errors made in an attempt to contract pelvic floor muscles .COMMOV- contraction of other muscles ( using rectus abdominus, glutes and adductors ) MOV- pelvic tilts , breath holding and straining performed in addition to or instead of an actual pelvic floor muscle contraction
- 57% of woman show Commov when assessing technique.
Will pelvic floor muscle training work? (Neels et al. 2018)
- Lack of understanding – Lack of clarity, as to why PFM should be exercised . Woman are unsure as to why these exercises need to be done. Due to the lack of understanding , woman are unable to make informed decision to partake in PFMT
- Waste of time- Woman may find it difficult to continue with PFMT in the absence of noticeable benefit. No immediate effect from training leads woman to feel as though there is no return for their efforts and that PFMT is waste of time
- The nature of PFMT – woman have described PFM exercises as tedious, a daily battle, a nuisance and boring
- Timing? This study conducted found that woman feel the PFMT is difficult to factor into their daily schedule. Due to the personal nature of the exercise need to be done alone and in a quiet place for concentration also many feel embarrassed to do exercises around others
Prolapse and incontinence, it’s a female problem right?(Hirschhorn et al. 2013)
- Study investigated male perceptions of incontinence and pelvic floor muscle training – 66% of men were unaware that males were required to do PFMT
- Widely perceived as a female issue
- Stigma and embarrassment – leads to under reporting of symptoms within the male population
- Lack of research regarding male experiences in PFMT , body of research lies within the female population
Add your content to this page here!
Treatment [edit | edit source]
Pelvic floor exercises for beginners:[5]
Pelvic floor exercises for men: [6]
Progressive pelvic floor exercises: Episode 1: [7] Episode 2:[8] Episode 3: [9] Episode 4: [10] Episode 5: [11]
References[edit | edit source]
see adding references tutorial.
- ↑ https://www.continence.org.au/pages/pelvic-floor-men.html
- ↑ http://www.pelvicfloorfirst.org.au/pages/the-pelvic-floor.html
- ↑ https://www.pelvicpainrehab.com/low-tone-pelvic-floor-dysfunction/4587/pelvic-floor-movement/
- ↑ http://pogp.csp.org.uk/publications/pelvic-floor-muscle-exercises-men
- ↑ https://prostate.net/articles/erectile-dysfunction-pelvic-floor-connection
6.HAY-SMITH, E., RYAN, K. and DEAN, S., 2007. The silent, private exercise: experiences of pelvic floor muscle training in a sample of women with stress urinary incontinence. Physiotherapy. vol. 93, no. 1, pp. 53-61.
7.HIRSCHHORN, A.D., KOLT, G.S. and BROOKS, A.J., 2013. Barriers and enablers to the provision and receipt of preoperative pelvic floor muscle training for men having radical prostatectomy: a qualitative study. BMC Health Services Research. vol. 13, no. 1, pp. 305.
8.MASON, L., GLENN, S., WALTON, I. and HUGHES, C., 2001. The instruction in pelvic floor exercises provided to women during pregnancy or following delivery. Midwifery. 2001, vol. 17, no. 1, pp. 55-64.
9.NEELS, H., DE WACHTER, S., WYNDAELE, J., VAN AGGELPOEL, T. and VERMANDEL, A., 2018. Common errors made in attempt to contract the pelvic floor muscles in women early after delivery: A prospective observational study. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 01, vol. 220, pp. 113-117.