Cardiac Implantable Electronic Devices (CIEDs): Difference between revisions
Justin Bryan (talk | contribs) No edit summary |
Justin Bryan (talk | contribs) No edit summary |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
[[File:Pacemaker.jpeg|right|frameless|399x399px]] | [[File:Pacemaker.jpeg|right|frameless|399x399px]] | ||
[[Anatomy of the Human Heart|Cardiac]] implantable electronic devices or CIEDs, are a very common medical device<ref name=":1">Stevenson I, Voskoboinik A. Cardiac rhythm management devices. Australian Journal of General Practice 2018; 47(5): n.p. Availible from:https://www1.racgp.org.au/ajgp/2018/may/cardiac-rhythm-management-devices</ref> | [[Anatomy of the Human Heart|Cardiac]] implantable electronic devices or CIEDs, or Cardiac Rhythm Management Devices, are a very common medical device. The number of implanted cardiovascular devices has dramatically increased in recent years. Many people utilize "Pacemaker" as general term for these devices, but in actuality, a pacemaker is a specific type of CIED. Additionally, there is a variety of other devices that that fall under this general umbrella.<ref name=":1">Stevenson I, Voskoboinik A. Cardiac rhythm management devices. Australian Journal of General Practice 2018; 47(5): n.p. Availible from:https://www1.racgp.org.au/ajgp/2018/may/cardiac-rhythm-management-devices</ref> | ||
There are several major types of cardiac rhythm management devices: | |||
There are | |||
# Pacemakers | # Pacemakers | ||
# Automatic implantable [[Cardioversion|cardioverter-defibrillators]] (AICD/ICD) (may be co-implanted as an ICD-pacemaker combination) | # Defibrillators - Automatic implantable [[Cardioversion|cardioverter-defibrillators]] (AICD/ICD) (may be co-implanted as an ICD-pacemaker combination) | ||
# Loop Recorders | |||
Leadless cardiac pacemakers (LLPM) are a recently introduced type of cardiac conduction device. These pacemakers are self-contained right ventricular single-chamber pacemakers<ref name=":0" />. Outcomes have generally been positive for cases where LLPM has been utilized and initially the safety and efficacy appears promising. For this reason, their use has been on the rise resulting is a shift that now marks a new era of cardiac pacing. <ref>Curnis A, Salghetti F, Cerini M, Fabbricatore D, Ghizzoni G, Arrigoni L, Generati G, Arabia G, Maiolo V, Aboelhassan M, Bontempi L. [https://onlinelibrary.wiley.com/doi/10.1111/pace.14097 Leadless pacemaker: State of the art and incoming developments to broaden indications]. Pacing and Clinical Electrophysiology. 2020 Oct 22.Available from:https://onlinelibrary.wiley.com/doi/10.1111/pace.14097 (accessed 29.4.2021)</ref> | Leadless cardiac pacemakers (LLPM) are a recently introduced type of cardiac conduction device. These pacemakers are self-contained right ventricular single-chamber pacemakers<ref name=":0">Radiopedia [https://radiopaedia.org/articles/cardiac-conduction-devices Cardiac conduction devices] Available:https://radiopaedia.org/articles/cardiac-conduction-devices (accessed 29.4.2021)</ref>. Outcomes have generally been positive for cases where LLPM has been utilized and initially the safety and efficacy appears promising. For this reason, their use has been on the rise resulting is a shift that now marks a new era of cardiac pacing. <ref>Curnis A, Salghetti F, Cerini M, Fabbricatore D, Ghizzoni G, Arrigoni L, Generati G, Arabia G, Maiolo V, Aboelhassan M, Bontempi L. [https://onlinelibrary.wiley.com/doi/10.1111/pace.14097 Leadless pacemaker: State of the art and incoming developments to broaden indications]. Pacing and Clinical Electrophysiology. 2020 Oct 22.Available from:https://onlinelibrary.wiley.com/doi/10.1111/pace.14097 (accessed 29.4.2021)</ref> | ||
== Why | == Why Cardiac Rhythm Management Devices are Used == | ||
'''Pacemakers:''' Used primarily to control the rhythm or pace of the beating heart, generally in cases where the concern is symptomatic bradycardia due to medication, heart block, heart failure, or abnormal cardiac rhythm. Pacemakers help control the inherent beating of the heart, or in some cases, may be solely responsible for generating and maintaining rhythm in a heart that does not produce any inherent beating (i.e. total health block).<ref name=":1" /> | |||
There are many different variations of pacemakers, each of which can be used to address a specific condition or symptom. Pacing requirements can fall on a spectrum from entirely dependent, where the heart does not produce any rhythm, to intermittent pacing where the device senses rhythm changes or deficiencies and "assists" only when needed.<ref name=":1" /> | |||
Types of therapies pacemakers can provide include those that may address bradycardia originating in either the atria or ventricle. Another therapy cardiac resynchronization therapy (CRT) use in the treatment of heart failure. CRT provides pacing to both ventricles, which often become paced out of sync in heart failure patients. Correcting this using CRT will then result in improved cardiac functioning. Anti-tachycardia pacing (ATP) in a treatment used for those with arrhythmia that increase the rate that a chamber is paced (i.e. ventricular tachycardia or Atrial fibrillation). These pacemakers may disrupt the arrhythmia by inducing the heart to be temporarily paced at a rate greater than that created by the arrhythmia. Pacemakers may also be set up to monitor for certain rhythm changes such as missed beats, and provide pacing as appropriate.<ref name=":1" /> | |||
'''Defibrillators:''' Automatic implantable [[Cardioversion|cardioverter-defibrillators]] (AICD/ICD) are utilized in patients with conditions including reduced ventricular function or ventricular arrhythmia (i.e. ventricular tachycardia), which can put them at risk for sudden cardiac death. Defibrillators can utilize one to three leads to monitor different chamber (similar to pacemakers), or they may utilize no leads, monitoring rhythm from the subcutaneous unit only. When a life threatening condition is sensed, the defibrillator will provide an electric shock intended to restore the hearts normal rhythm.<ref name=":1" /> | |||
'''Loop Recorders:''' These devices are purely monitoring devices and are not utilized to provide any therapy. They are used as part of the diagnostic process in cases where the cause of a specific cardiac event is unable to be determined after it occurs. Loop recorders can then provide information regarding heart rhythm that can be used to provide insight on potential underlying causes of such events. Common events that may warrant a loop recorder include syncope or palpitations that occur without an obvious cause.<ref name=":1" /> | |||
== Major components == | == Major components == | ||
There are many variations of Cardiac Rhythm Management Devices depending on their application and manufacturer. Generally though, the two main components of these devices are a pulse generator and leads (except leadless pacemakers) | |||
# A pulse generator: A small metal disk or box commonly implanted in an area of the chest wall just below the clavicle. The generator contains a battery used to produce the electrical current that controls rhythm, as well as power the small computer chip that interprets inherent rhythms and controls the activation and production of impulses used for various therapies.<ref name=":2">John Hopkins [https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pacemaker-insertion Pacemake]r Available from:https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pacemaker-insertion (accessed 30.4.2021)</ref><ref name=":4">Lak HM, Goyal A. Pacemaker Types and Selection. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. Available from: <nowiki>https://www.ncbi.nlm.nih.gov/books/NBK556011/</nowiki></ref> | |||
# A pulse generator: | # The lead(s) are wires used for both sensing of inherent rhythm and conduction of impulses from the pulse generator to the heart. The lead(s) of most modern pacemakers are routed transvenously, or travel through a vein starting near the pulse generator and ending up inside the heart chambers. The tip of each lead is embedded in the tissue of the corresponding chamber that it controls.<ref name=":2" /><ref name=":4" /> | ||
== Pacemakers == | == Pacemakers == | ||
[[File:Pakemaker leads.png|right|frameless|503x503px]] | [[File:Pakemaker leads.png|right|frameless|503x503px]] | ||
Categorization depends on the number of electrodes and location of pacing: | |||
* Single chamber cardiac pacers: lead terminates in the right ventricle | * Single chamber cardiac pacers: lead terminates in the right ventricle | ||
| Line 43: | Line 43: | ||
== Automatic implantable cardioverter defibrillators == | == Automatic implantable cardioverter defibrillators == | ||
[[File:AICD.jpeg|right|frameless]] | [[File:AICD.jpeg|right|frameless]] | ||
AICDs are common cardiac devices designed for both patient monitoring and therapy in case of ventricular tachycardia or [[Atrial Fibrillation|fibrillation]]. AICDs consist of various combinations of sensing and shocking electrodes. They are frequently combined with a pacemaker, treating both the patient’s established arrhythmia and also acting as a fail-safe system should ventricular fibrillation or ventricular tachycardia occur. | AICDs are common cardiac devices designed for both patient monitoring and therapy in case of ventricular tachycardia or [[Atrial Fibrillation|fibrillation]]. AICDs consist of various combinations of sensing and shocking electrodes. They are frequently combined with a pacemaker, treating both the patient’s established arrhythmia and also acting as a fail-safe system should ventricular fibrillation or ventricular tachycardia occur.<ref name=":1" /> | ||
== Activation == | == Activation == | ||
| Line 65: | Line 65: | ||
* This bionic pacemaker follows the natural change in heart rhythm that occurs with breathing, and causes a steep improvement in the efficiency at which the heart supplies blood to the body. The normal heartbeat is a dynamic phenomenon. With every intake of [[Breathing Pattern Disorders|breath]], it can be felt to speed up, only to slow down with exhalation – a fascinating change in speed and rhythm called respiratory sinus arrhythmia. There are also several more minor other body processes which modulate the heart rate, causing normal heart rate variability. | * This bionic pacemaker follows the natural change in heart rhythm that occurs with breathing, and causes a steep improvement in the efficiency at which the heart supplies blood to the body. The normal heartbeat is a dynamic phenomenon. With every intake of [[Breathing Pattern Disorders|breath]], it can be felt to speed up, only to slow down with exhalation – a fascinating change in speed and rhythm called respiratory sinus arrhythmia. There are also several more minor other body processes which modulate the heart rate, causing normal heart rate variability. | ||
* Most automatic pacemakers generate a metronome-like rhythm when the patient is at rest, irrespective of the body’s other operations. This doesn’t take advantage of the natural changes that occur in the body. | * Most automatic pacemakers generate a metronome-like rhythm when the patient is at rest, irrespective of the body’s other operations. This doesn’t take advantage of the natural changes that occur in the body. | ||
* This new bionic pacemaker represent a novel therapy in addition to those already available for the treatment of heart failure.<ref name=":3" /> | * This new bionic pacemaker represent a novel therapy in addition to those already available for the treatment of heart failure.<ref name=":3">News Medical New type of bionic pacemaker Available:https://www.news-medical.net/news/20191114/New-type-of-bionic-pacemaker.aspx (accessed 30.4.2021)</ref> | ||
== Physiotherapy == | == Physiotherapy == | ||
Revision as of 22:31, 24 March 2023
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Justin Bryan and Kim Jackson
Introduction[edit | edit source]
Cardiac implantable electronic devices or CIEDs, or Cardiac Rhythm Management Devices, are a very common medical device. The number of implanted cardiovascular devices has dramatically increased in recent years. Many people utilize "Pacemaker" as general term for these devices, but in actuality, a pacemaker is a specific type of CIED. Additionally, there is a variety of other devices that that fall under this general umbrella.[1]
There are several major types of cardiac rhythm management devices:
- Pacemakers
- Defibrillators - Automatic implantable cardioverter-defibrillators (AICD/ICD) (may be co-implanted as an ICD-pacemaker combination)
- Loop Recorders
Leadless cardiac pacemakers (LLPM) are a recently introduced type of cardiac conduction device. These pacemakers are self-contained right ventricular single-chamber pacemakers[2]. Outcomes have generally been positive for cases where LLPM has been utilized and initially the safety and efficacy appears promising. For this reason, their use has been on the rise resulting is a shift that now marks a new era of cardiac pacing. [3]
Why Cardiac Rhythm Management Devices are Used[edit | edit source]
Pacemakers: Used primarily to control the rhythm or pace of the beating heart, generally in cases where the concern is symptomatic bradycardia due to medication, heart block, heart failure, or abnormal cardiac rhythm. Pacemakers help control the inherent beating of the heart, or in some cases, may be solely responsible for generating and maintaining rhythm in a heart that does not produce any inherent beating (i.e. total health block).[1]
There are many different variations of pacemakers, each of which can be used to address a specific condition or symptom. Pacing requirements can fall on a spectrum from entirely dependent, where the heart does not produce any rhythm, to intermittent pacing where the device senses rhythm changes or deficiencies and "assists" only when needed.[1]
Types of therapies pacemakers can provide include those that may address bradycardia originating in either the atria or ventricle. Another therapy cardiac resynchronization therapy (CRT) use in the treatment of heart failure. CRT provides pacing to both ventricles, which often become paced out of sync in heart failure patients. Correcting this using CRT will then result in improved cardiac functioning. Anti-tachycardia pacing (ATP) in a treatment used for those with arrhythmia that increase the rate that a chamber is paced (i.e. ventricular tachycardia or Atrial fibrillation). These pacemakers may disrupt the arrhythmia by inducing the heart to be temporarily paced at a rate greater than that created by the arrhythmia. Pacemakers may also be set up to monitor for certain rhythm changes such as missed beats, and provide pacing as appropriate.[1]
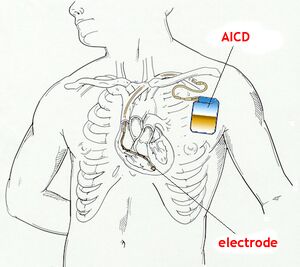
Defibrillators: Automatic implantable cardioverter-defibrillators (AICD/ICD) are utilized in patients with conditions including reduced ventricular function or ventricular arrhythmia (i.e. ventricular tachycardia), which can put them at risk for sudden cardiac death. Defibrillators can utilize one to three leads to monitor different chamber (similar to pacemakers), or they may utilize no leads, monitoring rhythm from the subcutaneous unit only. When a life threatening condition is sensed, the defibrillator will provide an electric shock intended to restore the hearts normal rhythm.[1]
Loop Recorders: These devices are purely monitoring devices and are not utilized to provide any therapy. They are used as part of the diagnostic process in cases where the cause of a specific cardiac event is unable to be determined after it occurs. Loop recorders can then provide information regarding heart rhythm that can be used to provide insight on potential underlying causes of such events. Common events that may warrant a loop recorder include syncope or palpitations that occur without an obvious cause.[1]
Major components[edit | edit source]
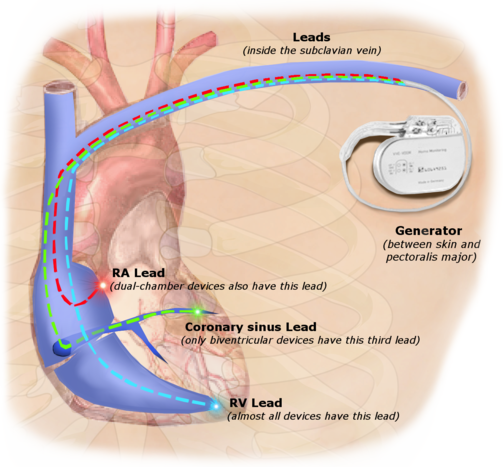
There are many variations of Cardiac Rhythm Management Devices depending on their application and manufacturer. Generally though, the two main components of these devices are a pulse generator and leads (except leadless pacemakers)
- A pulse generator: A small metal disk or box commonly implanted in an area of the chest wall just below the clavicle. The generator contains a battery used to produce the electrical current that controls rhythm, as well as power the small computer chip that interprets inherent rhythms and controls the activation and production of impulses used for various therapies.[4][5]
- The lead(s) are wires used for both sensing of inherent rhythm and conduction of impulses from the pulse generator to the heart. The lead(s) of most modern pacemakers are routed transvenously, or travel through a vein starting near the pulse generator and ending up inside the heart chambers. The tip of each lead is embedded in the tissue of the corresponding chamber that it controls.[4][5]
Pacemakers[edit | edit source]
Categorization depends on the number of electrodes and location of pacing:
- Single chamber cardiac pacers: lead terminates in the right ventricle
- Dual-chamber (DDD) pacemakers have two leads (one in the right atrium, one in the right ventricle), each capable of sensing intrinsic electrical activity to determine the need for pacing in each chamber. For “on-demand” dual-chamber pacemakers—the most common types—atrial pacing is determined by the lower rate limit while ventricular pacing is determined by the separately programmed maximum AV delay.[6]
- Biventricular pacers (also known as cardiac resynchronisation therapy): Inserted in the same fashion as a standard pacemaker via the subclavian vein. The major distinguishing feature of a biventricular pacemaker is the insertion of a left ventricular lead to accomplish left ventricular pacing, in addition to the right ventricular lead for right ventricular pacing . Biventricular pacing is an excellent option for certain patients with advanced HF[7].
- Leadless cardiac pacers: implanted into the right ventricle with no leads, introduced in 2015. Not everyone is a candidate for a leadless pacemaker. Currently, the device is available only for patients with certain medical conditions and a slow heart rate (bradycardia) who need single-chamber pacing only. Because there are no wires or generator, there is no need for recipient to limit upper body activity after the implant[8].[2]
Automatic implantable cardioverter defibrillators[edit | edit source]
AICDs are common cardiac devices designed for both patient monitoring and therapy in case of ventricular tachycardia or fibrillation. AICDs consist of various combinations of sensing and shocking electrodes. They are frequently combined with a pacemaker, treating both the patient’s established arrhythmia and also acting as a fail-safe system should ventricular fibrillation or ventricular tachycardia occur.[1]
Activation[edit | edit source]
If the heart's rate is slower than the programmed limit, an electrical impulse is sent through the lead to the electrode and causes the heart to beat at a faster rate.
When the heart beats at a rate faster than the programmed limit, the pacemaker generally monitors the heart rate and will not pace. Modern pacemakers are programmed to work on demand only, so they do not compete with natural heartbeats. Generally, no electrical impulses will be sent to the heart unless the heart's natural rate falls below the pacemaker's lower limit.
A biventricular pacemaker (used in the treatment of specific types of heart failure) is used when the two ventricles do not pump in a normal manner (ie ventricular dyssynchrony). When this happens, less blood is pumped by the heart. A biventricular pacemaker paces both ventricles at the same time, increasing the amount of blood pumped by the heart. This type of treatment is called cardiac resynchronization therapy or CRT[4].
Landmark Innovations[edit | edit source]
- Cardiologists at Monash Health have implanted the world’s first totally leadless, physiologic pacemaker system, designed to improve cardiac function in a patient with a severe cardiomyopathy, otherwise known as heart failure. This unique procedure has, for the first time, used two innovative medical devices to resynchronise the pumping of the heart without requiring any wires to be implanted inside the patient’s heart.
- In contrast to transvenous systems, the ‘leadless’ devices used in this patient can be implanted directly inside the heart’s ventricles without any connecting wires.
- The procedure utilises keyhole access through a vein, where an ingenious, ultrasonically activated pacemaker the size of a grain of rice was implanted in the left ventricle. Using the same access, the latest generation, leadless right ventricular pacemaker was also implanted.
Using a new synchronisation method described as ‘physiological pacing’, the right-sided device can sense and track the activity of the atrium above, where the heart’s normal rhythm originates. Working in combination, these devices will provide physiologic, cardiac resynchronisation therapy without the need for wires inside the heart[9].
2.A new study published in the Journal of Physiology on November 14, 2019, reports the development of a radically different type of cardiac pacemaker which could change the prognosis of patients with heart failure.
- This bionic pacemaker follows the natural change in heart rhythm that occurs with breathing, and causes a steep improvement in the efficiency at which the heart supplies blood to the body. The normal heartbeat is a dynamic phenomenon. With every intake of breath, it can be felt to speed up, only to slow down with exhalation – a fascinating change in speed and rhythm called respiratory sinus arrhythmia. There are also several more minor other body processes which modulate the heart rate, causing normal heart rate variability.
- Most automatic pacemakers generate a metronome-like rhythm when the patient is at rest, irrespective of the body’s other operations. This doesn’t take advantage of the natural changes that occur in the body.
- This new bionic pacemaker represent a novel therapy in addition to those already available for the treatment of heart failure.[10]
Physiotherapy[edit | edit source]
There are no specific international policies regarding the administration of physiotherapy modalities in cardiac rhythm device patients and, thus, there are no specific guidelines to be implemented at the local level. Review of the literature and of recommendations from CRD manufacturers suggests that TENS, Diathermy, and Interferential Electrical Current Therapy are best avoided in patients with CRDs[11].
Use of upper limbs For 6 to 8 weeks (with device with leads):
• Avoid upper arm movement on the side of your pacemaker such as reaching high, raking, hanging things and swinging a golf club. • Do shoulder rolls daily on the side of the pacemaker to prevent shoulder stiffness. • You can have sex when you feel comfortable. • Ask your doctor when you can drive. • Do not do any heavy lifting. This means do not lift anything over kilograms or 10 pounds such as a bag of groceries, small suitcase or small child.
A patient's lifestyle is usually not modified to any great degree after the insertion of a pacemaker. There are a few activities that are unwise such as full contact sports and activities that involve intense magnetic fields (should be informed from treating Cardiologist)
- eg large and powerful magnets (MRI) affect pacemakers; do not use beds that vibrate; Large motors: the power from motors such as chain saws, cars, tractors, lawnmowers and recreational vehicles may confuse a pacemaker. If this happens, you will feel dizzy. This is related to how close you are. You need to be 1 foot or 30 centimetres from a working motor.[12]
Final Ending[edit | edit source]
A British charity wants to remove pacemakers from people who have died in the UK and send the devices to developing countries for re-use. Pace4Life says thousands of the life-saving devices, which cost thousands of pounds, are typically thrown away or buried with patients each year in the UK[13].
- Pacemaker reuse is feasible and safe and is a viable option for patients with bradyarrhythmias. Other than the expected lower battery life, reuse of pacemaker generators is noninferior to the use of new devices[14].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Stevenson I, Voskoboinik A. Cardiac rhythm management devices. Australian Journal of General Practice 2018; 47(5): n.p. Availible from:https://www1.racgp.org.au/ajgp/2018/may/cardiac-rhythm-management-devices
- ↑ 2.0 2.1 Radiopedia Cardiac conduction devices Available:https://radiopaedia.org/articles/cardiac-conduction-devices (accessed 29.4.2021)
- ↑ Curnis A, Salghetti F, Cerini M, Fabbricatore D, Ghizzoni G, Arrigoni L, Generati G, Arabia G, Maiolo V, Aboelhassan M, Bontempi L. Leadless pacemaker: State of the art and incoming developments to broaden indications. Pacing and Clinical Electrophysiology. 2020 Oct 22.Available from:https://onlinelibrary.wiley.com/doi/10.1111/pace.14097 (accessed 29.4.2021)
- ↑ 4.0 4.1 4.2 John Hopkins Pacemaker Available from:https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pacemaker-insertion (accessed 30.4.2021)
- ↑ 5.0 5.1 Lak HM, Goyal A. Pacemaker Types and Selection. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556011/
- ↑ Goldberger AL, Goldberger ZD, Shvilkin A. Clinical electrocardiography: a simplified approach e-book. Elsevier Health Sciences; 2017 Mar 19.Available from: https://www.sciencedirect.com/topics/nursing-and-health-professions/dual-chamber-pacemaker(accessed 30.4.2021)
- ↑ Helio Biventricular pacing Available from:https://www.healio.com/cardiology/learn-the-heart/cardiology-review/topic-reviews/biventricular-pacing (accessed 30.4.2021)
- ↑ Cleveland clinic LLPM Available :https://my.clevelandclinic.org/health/treatments/17166-pacemakers-leadless-pacemaker (accessed 30.4.2021)
- ↑ Monash Health Monash Health implants world-first leadless pacemaker treatment for heart failure. Available: https://monashhealth.org/latest-news/2020/10/15/monash-health-implants-world-first-leadless-pacemaker-treatment-for-heart-failure/ (accessed 30.4.2021)
- ↑ News Medical New type of bionic pacemaker Available:https://www.news-medical.net/news/20191114/New-type-of-bionic-pacemaker.aspx (accessed 30.4.2021)
- ↑ Digby GC, Daubney ME, Baggs J, Campbell D, Simpson CS, Redfearn DP, Brennan FJ, Abdollah H, Baranchuk A. Physiotherapy and cardiac rhythm devices: a review of the current scope of practice. Europace. 2009 Jul 1;11(7):850-9.Available from:https://academic.oup.com/europace/article/11/7/850/498953 (accessed 30.4.2021)
- ↑ St Joes You and your pacemakerAvailable from:https://www.stjoes.ca/patients-visitors/patient-education/p-t/PacemakerSJH-trh%20(2).pdf (accessed 30.4.2021)
- ↑ Mazumdar T. British Charity Calls for Reuse of Pacemakers Abroad. BBB News Health. 2013.Available: https://www.bbc.com/news/health-24828244(accessed 30.4.2021)
- ↑ Nava S, Morales JL, Márquez MF, Barrera F, Gómez J, Colín L, Brugada J, Iturralde P. Reuse of pacemakers: comparison of short and long-term performance. Circulation. 2013 Mar 19;127(11):1177-83.Available:https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.113.001584 (accessed 30.4.2021)