Baastrup Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
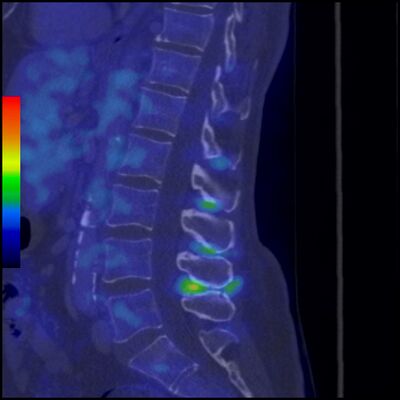
[[File:Baastrup-disease-1.jpeg|thumb|Baastrup syndrome with active inflammation (e.g. bursitis)|alt=|400x400px]] | [[File:Baastrup-disease-1.jpeg|thumb|Baastrup syndrome with active inflammation (e.g. bursitis)|alt=|400x400px]] | ||
Baastrup syndrome (also referred to as kissing spines) is a cause of low back pain characterized by interspinous bursitis and other degenerative changes of the bones and soft tissues where adjacent spinous processes in the lumbar spine rub against each other. | Baastrup syndrome (also referred to as kissing spines) is a cause of low back pain characterized by interspinous bursitis and other degenerative changes of the bones and soft tissues where adjacent spinous processes in the lumbar spine rub against each other.<ref name=":4">Radiopedia Basstrup Syndrome Available;https://radiopaedia.org/articles/baastrup-disease-1?lang=us (accessed 29.8.2022)</ref> | ||
Kissing Spine mainly affects the lumbar area of the spine, with L4-L5 being the most frequently affected level <ref name=":3">Filippiadis D.K. et al., Baastrup’s disease (kissing spines syndrome): a pictorial review, Springer, 2015, 6(1): 123–128</ref>, but it has also been reported in the cervical spine.<ref name=":8">Rajasekaran S. et al., Baastrup’s Disease as a Cause of Neurogenic Claudication: a case report, Lippincott Williams & Wilkins, 2003, 28(14): 273-275</ref> | Kissing Spine mainly affects the lumbar area of the spine, with L4-L5 being the most frequently affected level <ref name=":3">Filippiadis D.K. et al., Baastrup’s disease (kissing spines syndrome): a pictorial review, Springer, 2015, 6(1): 123–128</ref>, but it has also been reported in the cervical spine.<ref name=":8">Rajasekaran S. et al., Baastrup’s Disease as a Cause of Neurogenic Claudication: a case report, Lippincott Williams & Wilkins, 2003, 28(14): 273-275</ref> | ||
Clinically Relevant Anatomy: See [[Lumbar Anatomy]] | |||
Clinically Relevant Anatomy: See [[Lumbar Anatomy]] | |||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
Baastrup Syndrome tends to be more common in the elderly. Other suggested risk factors are:<ref name=":1">Kacki S. et al., Baastrup’s Sign (Kissing Spines): A neglected condition in paleopathology, International Journal of Paleopathology, 2011, 1(2): 104-110</ref> <ref name=":3" /> | |||
*Excessive lordosis which results in increased mechanical pressure | *Excessive lordosis which results in increased mechanical pressure | ||
*Repetitive strains of the interspinous ligament with subsequent degeneration and collapse | *Repetitive strains of the interspinous ligament with subsequent degeneration and collapse | ||
| Line 32: | Line 23: | ||
*Stiffening of the thoracic spine or the thoracolumbar transition | *Stiffening of the thoracic spine or the thoracolumbar transition | ||
*Obesity | *Obesity | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
[[File:Baastrup_3.png|alt=|thumb|400x400px|Basstrup or Kissing Spine]] | |||
Patients with Baastrup syndrome typically show an excessive lordosis.<ref name=":3" /> <ref name=":19">Jang E-C. et al., Posterior epidural fibrotic mass associated with Baastrup’s disease, Springer, 2010; 19(2): 165-168</ref> Patients with Kissing Spine often complain about back pain, more specifically, midline pain that radiates distally and proximally, increasing on extension and reducing on flexion.<ref name=":2">Singla A. et al., Baastrup’s disease: the kissing spine, World Journal of Clinical Cases, 2014, 2(2): 45-47.</ref> <ref name=":3" /> This abnormal contact between adjacent spinous processes can lead to neoarthrosis and formation of an adventitious bursa. This can be seen pathologically on MRI. <ref name=":0">Kwong Y. et al., MDCT Findings in Baastrup Disease: Disease or Normal Feature of the Aging Spine?,American Journal of Roentgenology, 2011, 196(5):1156-9.</ref> <ref name=":9">Maes R. et al., Lumbar Interspinous Bursitis (Baastrup Disease) in a Symptomatic Population: Prevalence on Magnetic Resonance Imaging, The Spine Journal, 2008, 33(7): 211-215</ref> <ref>FarinhaF. et al., Baastrup’s disease: a poorly recognized cause of back pain, ActaReumatol Port, 2015, 40:302-303</ref> | |||
Rotation and lateral flexion are usually painful with flexion being the least painful of all lumbar movements.<ref name=":12">Hertling D. et al., Management of common musculoskeletal disorders: Physical Therapy Principles and Methods, Lippincott Williams & Wilkins, 2006, 4th edition</ref> Baastrup’s disease can result in intraspinal cysts secondary to an interspinous bursitis which may, in rare cases, cause symptomatic spinal stenosis and neurogenic claudation <ref name=":0" /> | |||
Rotation and lateral flexion are usually painful with flexion being the least painful of all lumbar movements.<ref name=":12">Hertling D. et al., Management of common musculoskeletal disorders: Physical Therapy Principles and Methods, Lippincott Williams & Wilkins, 2006, 4th edition</ref> Baastrup’s disease can result in intraspinal cysts secondary to an interspinous bursitis which may, in rare cases, cause symptomatic spinal stenosis and neurogenic claudation <ref name=":0" /> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
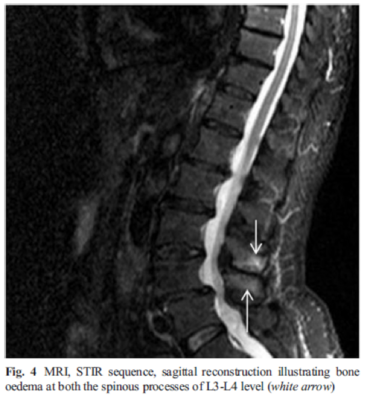
[[File:Baastrup_4.png|alt=|right|frameless|399x399px]] | |||
Baastrup Syndrome cannot be diagnosed by simply assessing the lumbar spine (see [[Lumbar Assessment|clinical examination]]), imaging modalities are required to prevent misdiagnosis. <ref name=":3" /> | |||
# '''CT and Xrays:''' Often shows close approximation and contact of adjacent spinous processes (kissing spines). Resultant enlargement, flattening, and reactive sclerosis of apposing interspinous surfaces | |||
# '''Magnetic Resonance Imaging MRI:''' May demonstrate interspinous bursal fluid and posterocentral epidural cyst(s). MRI can be very helpful in determining whether there is resulting posterior compression of the thecal sac. | |||
''' | |||
'''Magnetic Resonance Imaging MRI''' | |||
== Outcome Measures == | == Outcome Measures == | ||
| Line 106: | Line 41: | ||
*[[Quebec Back Pain Disability Scale]] | *[[Quebec Back Pain Disability Scale]] | ||
*[[Visual Analogue Scale]] | *[[Visual Analogue Scale]] | ||
*[[ | *[[Fingertips to Floor Distance - Special Test|Fingertip-to-Floor]] (FTF) Test | ||
== Examination == | == Examination == | ||
[[File:Baastrup_5.png|alt=|thumb|Stork Test]]Diagnosis of Baastrup’s disease is verified with clinical examination as well as imaging studies.<ref name=":3" /> Symptoms include low back pain with midline distribution that exacerbates when performing extension, relieved during flexion and is exaggerated upon finger pressure at the level of the pathologic interspinous ligament. Rotation and lateral flexion are also very painful. <ref name=":3" /> The pain can be described as a sharp or deep ache, often worse during physical activities that increase lumbar lordosis or compression of these structures.<ref name=":6">DePalma M.J., iSPINE Evidence Based Interventional Spine Care, Demos Medical, 2011, 4-8</ref> | |||
Throughout the physical examination, the physiotherapist uses active and passive techniques with the intention of evoking complaints. Active spinal extension can reproduce the symptoms. The stork test is very beneficial in the examination of this disease.<ref name=":6" /> When the patient bends forward, relief is also gained.<ref name=":12" /> | |||
Throughout the physical examination, the physiotherapist uses active and passive techniques with the intention of evoking complaints. Active spinal extension can reproduce the symptoms. The stork test is very beneficial in the examination of this disease.<ref name=":6" /> When the patient bends forward, relief is also gained.<ref name=":12" /> | |||
== Medical Management == | == Medical Management == | ||
The main goal of any therapy is to reduce the lower back pain as well as a return to normal ADLs. Medical treatment can be conservative or surgical and an accurate diagnosis of the disease is necessary for determining appropriate treatment. | The main goal of any therapy is to reduce the lower back pain as well as a return to normal ADLs. Medical treatment can be conservative or surgical and an accurate diagnosis of the disease is necessary for determining appropriate treatment. Local steroid injection into the interspinous processes/ligament region may often ease the back pain 8. Surgical options include interspinous process decompression devices.<ref name=":4" /><ref name=":13">Lamer T.J. et al., Fluoroscopically-Guided Injections to Treat “Kissing Spine” Disease, Pain Physician, 2008; 11: 549-554</ref> | ||
An interspinous processes spacer (also known as a decompression spacer or interspinous posterior device) is a device implanted between spinous processes to open narrowed exiting foraminal nerve channels to treat lumbar radiculopathy caused by spinal stenosis. The process of implantation is usually minimally invasive, performed under local anesthesia. <ref>Radiopedia Interspinous processes spacer Available:https://radiopaedia.org/articles/interspinous-processes-spacer?lang=us (accessed 29.8.2022)</ref> | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
As alluded to, the main goal is the reduction of pain as well as hyperlordosis and to improve spinal function. Once the pain is managed, physical therapy management can begin, involving education, strengthening and stretching of the abdominal and spinal muscles.<ref name=":0" /> <ref name=":16" /> | As alluded to, the main goal is the reduction of pain as well as hyperlordosis and to improve spinal function. Once the pain is managed, physical therapy management can begin, involving education, strengthening and stretching of the abdominal and spinal muscles.<ref name=":0" /> <ref name=":16">Cohen S.T. et al., Management of Low Back Pain, British Medical Journal, 2008, 338: 100-106</ref> | ||
Treating the hyperlordosis is a key aspect, hence strengthening of the trunk muscles is recommended, along with postural education and hip flexor stretches. <ref>Scannell J.P. et al., Lumbar posture--should it, and can it, be modified? A study of passive tissue stiffness and lumbar position during activities of daily living, 2003, 83(10): 907-917</ref> | Treating the hyperlordosis is a key aspect, hence strengthening of the trunk muscles is recommended, along with postural education and hip flexor stretches. <ref>Scannell J.P. et al., Lumbar posture--should it, and can it, be modified? A study of passive tissue stiffness and lumbar position during activities of daily living, 2003, 83(10): 907-917</ref> | ||
| Line 151: | Line 71: | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Kissing spines is characterised by the close approximation and contact of adjoining spinous processes'. It is often treated with injections as pain relief in the first instance. Physical therapy should include stretching and strengthening exercises to reduce the mechanical pressure on the spine and any hyperlordosis. Baastrup’s syndrome is still relatively unknown and is often misdiagnosed and consequently treated incorrectly. <ref name=":14" /><br><br>Baastrup syndrome is more common in the lumbar spine with L4-L5 being the most affected region.<ref name=":3" /> People who are most likely to suffer from Kissing Spine are particularly elderly patients with a degenerative disc disease or hyperlordosis. Both of these conditions may lead to chronic contact between adjacent spinous processes. <ref>Pinto P.S. et al., Spinous Process Fractures associated with Baastrup disease, Clinical Imaging, 2004, 28(3): 219-222</ref> | Kissing spines is characterised by the close approximation and contact of adjoining spinous processes'. It is often treated with injections as pain relief in the first instance. Physical therapy should include stretching and strengthening exercises to reduce the mechanical pressure on the spine and any hyperlordosis. Baastrup’s syndrome is still relatively unknown and is often misdiagnosed and consequently treated incorrectly. <ref name=":14">Chen C.K.H. et al., Intraspinal Posterior Epidural Cysts Associated with Baastrup's Disease: Report of 10 patients, American Journal of Roentgenology, 2004, 182(1): 191-194</ref><br><br>Baastrup syndrome is more common in the lumbar spine with L4-L5 being the most affected region.<ref name=":3" /> People who are most likely to suffer from Kissing Spine are particularly elderly patients with a degenerative disc disease or hyperlordosis. Both of these conditions may lead to chronic contact between adjacent spinous processes. <ref>Pinto P.S. et al., Spinous Process Fractures associated with Baastrup disease, Clinical Imaging, 2004, 28(3): 219-222</ref> | ||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 06:43, 29 August 2022
Original Editors - Fien Selderslaghs, Mirabella Smolders, Matthias Steenwerckx, Wout Theys as part of the Vrije Universiteit Brussel Evidence-Based Practice Project
Top Contributors - Sofie Bourdinon, Scott Cornish, Nikki Rommers, Admin, Arno Vrambout, Kim Jackson, Lucinda hampton, Fien Selderslaghs, Uchechukwu Chukwuemeka, Vidya Acharya, Ceulemans Lisa, Aarti Sareen, 127.0.0.1 and WikiSysop
Introduction[edit | edit source]
Baastrup syndrome (also referred to as kissing spines) is a cause of low back pain characterized by interspinous bursitis and other degenerative changes of the bones and soft tissues where adjacent spinous processes in the lumbar spine rub against each other.[1]
Kissing Spine mainly affects the lumbar area of the spine, with L4-L5 being the most frequently affected level [2], but it has also been reported in the cervical spine.[3]
Clinically Relevant Anatomy: See Lumbar Anatomy
Epidemiology /Etiology[edit | edit source]
Baastrup Syndrome tends to be more common in the elderly. Other suggested risk factors are:[4] [2]
- Excessive lordosis which results in increased mechanical pressure
- Repetitive strains of the interspinous ligament with subsequent degeneration and collapse
- Incorrect posture
- Traumatic injuries
- Tuberculous spondylitis
- Bilateral forms of congenital hip dislocation
- Stiffening of the thoracic spine or the thoracolumbar transition
- Obesity
Characteristics/Clinical Presentation[edit | edit source]
Patients with Baastrup syndrome typically show an excessive lordosis.[2] [5] Patients with Kissing Spine often complain about back pain, more specifically, midline pain that radiates distally and proximally, increasing on extension and reducing on flexion.[6] [2] This abnormal contact between adjacent spinous processes can lead to neoarthrosis and formation of an adventitious bursa. This can be seen pathologically on MRI. [7] [8] [9]
Rotation and lateral flexion are usually painful with flexion being the least painful of all lumbar movements.[10] Baastrup’s disease can result in intraspinal cysts secondary to an interspinous bursitis which may, in rare cases, cause symptomatic spinal stenosis and neurogenic claudation [7]
Diagnostic Procedures[edit | edit source]
Baastrup Syndrome cannot be diagnosed by simply assessing the lumbar spine (see clinical examination), imaging modalities are required to prevent misdiagnosis. [2]
- CT and Xrays: Often shows close approximation and contact of adjacent spinous processes (kissing spines). Resultant enlargement, flattening, and reactive sclerosis of apposing interspinous surfaces
- Magnetic Resonance Imaging MRI: May demonstrate interspinous bursal fluid and posterocentral epidural cyst(s). MRI can be very helpful in determining whether there is resulting posterior compression of the thecal sac.
Outcome Measures[edit | edit source]
The following tests can be used to objectively determine the progress and efficacy of treatment:
Examination[edit | edit source]
Diagnosis of Baastrup’s disease is verified with clinical examination as well as imaging studies.[2] Symptoms include low back pain with midline distribution that exacerbates when performing extension, relieved during flexion and is exaggerated upon finger pressure at the level of the pathologic interspinous ligament. Rotation and lateral flexion are also very painful. [2] The pain can be described as a sharp or deep ache, often worse during physical activities that increase lumbar lordosis or compression of these structures.[11]
Throughout the physical examination, the physiotherapist uses active and passive techniques with the intention of evoking complaints. Active spinal extension can reproduce the symptoms. The stork test is very beneficial in the examination of this disease.[11] When the patient bends forward, relief is also gained.[10]
Medical Management[edit | edit source]
The main goal of any therapy is to reduce the lower back pain as well as a return to normal ADLs. Medical treatment can be conservative or surgical and an accurate diagnosis of the disease is necessary for determining appropriate treatment. Local steroid injection into the interspinous processes/ligament region may often ease the back pain 8. Surgical options include interspinous process decompression devices.[1][12]
An interspinous processes spacer (also known as a decompression spacer or interspinous posterior device) is a device implanted between spinous processes to open narrowed exiting foraminal nerve channels to treat lumbar radiculopathy caused by spinal stenosis. The process of implantation is usually minimally invasive, performed under local anesthesia. [13]
Physical Therapy Management[edit | edit source]
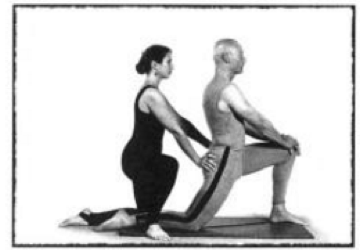
As alluded to, the main goal is the reduction of pain as well as hyperlordosis and to improve spinal function. Once the pain is managed, physical therapy management can begin, involving education, strengthening and stretching of the abdominal and spinal muscles.[7] [14]
Treating the hyperlordosis is a key aspect, hence strengthening of the trunk muscles is recommended, along with postural education and hip flexor stretches. [15]
When the abdominal muscles are weak, the hip flexors are mainly responsible in shaping the lumbar spine.[16] Furthermore the rectus femoris muscle is a continuation of the hip flexor complex so it is important to stretch these muscles. The hip flexors can become shorter through long-term sitting or resting. When these muscles shorten, it can affect the function of the gluteal and the spinal muscles.[17]
The stretch below is one example of how to lengthen these muscles. Resting the weight on the knee and the front foot, push the hips forward until a stretch is felt, keeping the trunk upright. Maintain this position for at least 20 seconds, and repeat this 3-5 times on each side.[16]
Figure 6: Stretching the hip flexors [16]
Motion of the gluteus maximus muscle during the flexion-extension cycle is decreased in patients with chronic low back pain, which is why strengthening of this muscle should be part of the physical management program [18]
Physical therapy is also suggested to be helpful for reducing the neuromuscular damage that is provoked by the disease and other treatments such as, heat therapy, ergotherapy and muscle relaxation techniques can be helpful [7]
Clinical Bottom Line[edit | edit source]
Kissing spines is characterised by the close approximation and contact of adjoining spinous processes'. It is often treated with injections as pain relief in the first instance. Physical therapy should include stretching and strengthening exercises to reduce the mechanical pressure on the spine and any hyperlordosis. Baastrup’s syndrome is still relatively unknown and is often misdiagnosed and consequently treated incorrectly. [19]
Baastrup syndrome is more common in the lumbar spine with L4-L5 being the most affected region.[2] People who are most likely to suffer from Kissing Spine are particularly elderly patients with a degenerative disc disease or hyperlordosis. Both of these conditions may lead to chronic contact between adjacent spinous processes. [20]
References[edit | edit source]
- ↑ 1.0 1.1 Radiopedia Basstrup Syndrome Available;https://radiopaedia.org/articles/baastrup-disease-1?lang=us (accessed 29.8.2022)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Filippiadis D.K. et al., Baastrup’s disease (kissing spines syndrome): a pictorial review, Springer, 2015, 6(1): 123–128
- ↑ Rajasekaran S. et al., Baastrup’s Disease as a Cause of Neurogenic Claudication: a case report, Lippincott Williams & Wilkins, 2003, 28(14): 273-275
- ↑ Kacki S. et al., Baastrup’s Sign (Kissing Spines): A neglected condition in paleopathology, International Journal of Paleopathology, 2011, 1(2): 104-110
- ↑ Jang E-C. et al., Posterior epidural fibrotic mass associated with Baastrup’s disease, Springer, 2010; 19(2): 165-168
- ↑ Singla A. et al., Baastrup’s disease: the kissing spine, World Journal of Clinical Cases, 2014, 2(2): 45-47.
- ↑ 7.0 7.1 7.2 7.3 Kwong Y. et al., MDCT Findings in Baastrup Disease: Disease or Normal Feature of the Aging Spine?,American Journal of Roentgenology, 2011, 196(5):1156-9.
- ↑ Maes R. et al., Lumbar Interspinous Bursitis (Baastrup Disease) in a Symptomatic Population: Prevalence on Magnetic Resonance Imaging, The Spine Journal, 2008, 33(7): 211-215
- ↑ FarinhaF. et al., Baastrup’s disease: a poorly recognized cause of back pain, ActaReumatol Port, 2015, 40:302-303
- ↑ 10.0 10.1 Hertling D. et al., Management of common musculoskeletal disorders: Physical Therapy Principles and Methods, Lippincott Williams & Wilkins, 2006, 4th edition
- ↑ 11.0 11.1 DePalma M.J., iSPINE Evidence Based Interventional Spine Care, Demos Medical, 2011, 4-8
- ↑ Lamer T.J. et al., Fluoroscopically-Guided Injections to Treat “Kissing Spine” Disease, Pain Physician, 2008; 11: 549-554
- ↑ Radiopedia Interspinous processes spacer Available:https://radiopaedia.org/articles/interspinous-processes-spacer?lang=us (accessed 29.8.2022)
- ↑ Cohen S.T. et al., Management of Low Back Pain, British Medical Journal, 2008, 338: 100-106
- ↑ Scannell J.P. et al., Lumbar posture--should it, and can it, be modified? A study of passive tissue stiffness and lumbar position during activities of daily living, 2003, 83(10): 907-917
- ↑ 16.0 16.1 16.2 Laughlin K., Overcome Neck and Back Pain, Simon & Schuster, 1998, 58-61
- ↑ Ross M., Stretching the Hip Flexors, National Strength & Conditioning Association, 1999, 21(3): 71-72
- ↑ Leinonen V. et al., Back an Hip Extensor Activities During Trunk Flexion/Extension: Effects of Low Back Pain and Rehabilitation, American Congress of Rehabilitation Medicine and the American Academy of Physical Medicine and Rehabilitation, 200, 81: 32-37
- ↑ Chen C.K.H. et al., Intraspinal Posterior Epidural Cysts Associated with Baastrup's Disease: Report of 10 patients, American Journal of Roentgenology, 2004, 182(1): 191-194
- ↑ Pinto P.S. et al., Spinous Process Fractures associated with Baastrup disease, Clinical Imaging, 2004, 28(3): 219-222