Bladder Anatomy: Difference between revisions
No edit summary |
No edit summary |
||
| (2 intermediate revisions by one other user not shown) | |||
| Line 10: | Line 10: | ||
It can accommodate about 1000 ml of urine with an average of about 400-600 ml which varies from one to another. The outer layer of the bladder wall is formed of smooth involuntary muscle fibers (detrusor muscles), it contracts at urination to empty the bladder. | It can accommodate about 1000 ml of urine with an average of about 400-600 ml which varies from one to another. The outer layer of the bladder wall is formed of smooth involuntary muscle fibers (detrusor muscles), it contracts at urination to empty the bladder. | ||
== | == Anatomical Surface of The Bladder == | ||
When it is filled it is like an oval, formed of four | When it is filled it is like an oval, formed of four surfaces. The neck is the constricted part, located inferiorly, and leads to the urethra. The apex is anterosuperior and points to the abdominal wall. The base/ fundus is located posteriorly, it is triangular-shaped its tip points backward. The body of the bladder is the main part of the bladder and is located between the apex and fundus<ref>Shermadou ES, Rahman S, Leslie SW. Anatomy, abdomen and pelvis, bladder.2018.</ref>. | ||
'''The trigon''' is a triangular region at the base of the bladder, lined with smooth muscle, collagen, and elastin to a lesser degree. Located between the internal-urethral meatus and the two ureteral orifices<ref>Hickling DR, Sun TT, Wu XR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4566164/ Anatomy and physiology of the urinary tract: relation to host defense and microbial infection. Urinary tract infections]: Molecular pathogenesis and clinical management. 2017 Feb 15:1-25.</ref>. | '''The trigon''' is a triangular region at the base of the bladder, lined with smooth muscle, collagen, and elastin to a lesser degree. Located between the internal-urethral meatus and the two ureteral orifices<ref>Hickling DR, Sun TT, Wu XR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4566164/ Anatomy and physiology of the urinary tract: relation to host defense and microbial infection. Urinary tract infections]: Molecular pathogenesis and clinical management. 2017 Feb 15:1-25.</ref>. | ||
| Line 17: | Line 17: | ||
. Available from: http://www.youtube.com/watch?v=UkTG6ncnZFg [last accessed 3/2/2023]</ref> | . Available from: http://www.youtube.com/watch?v=UkTG6ncnZFg [last accessed 3/2/2023]</ref> | ||
=== '''Urethral | === '''Urethral Sphincters''' === | ||
'''Internal urethral sphincter''' | '''Internal urethral sphincter''' | ||
| Line 38: | Line 38: | ||
Small branches from the obturator and inferior gluteal artery. | Small branches from the obturator and inferior gluteal artery. | ||
=== Lymphatic | === Lymphatic Drainage === | ||
The neck and fundus of the bladder through internal, sacral, and common iliac lymph nodes. | The neck and fundus of the bladder through internal, sacral, and common iliac lymph nodes. | ||
The superolateral aspect of the bladder is through the external iliac lymph nodes. | The superolateral aspect of the bladder is through the external iliac lymph nodes. | ||
== Clinical | == Clinical Relevance == | ||
[[Urinary Incontinence|Urinary incontinence]] | [[Urinary Incontinence|Urinary incontinence]] an involuntary loss of urine it is divided into subtypes; stress incontinence in which patients loss control when there is an increase in intraabdominal pressure, or sudden need to urinate as in urg incontinence and [[Overactive Bladder Syndrome|overactive bladder OAB]] that is associated with increase frequency of urination than normal and may be associated with urgency and named wet OAB. | ||
Atonic bladder(overflow incontinence) there is continuous loss of urine when there is insufficient contraction of detrusor muscle. | |||
Automatic (a spastic bladder) associated with spinal cord injury above the sacral level and associated with frequent urination. | |||
Neurogenic bladder | [[Detrusor Sphincter Dyssynergia|Detrusor sphincter dyssynergia]] (DSD), there is a spontaneous contraction of both urethral sphincter and detrusor muscle<ref>Dorsher PT, McIntosh PM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3287034/ Neurogenic bladder.] Advances in urology. 2012 Oct;2012.</ref>. | ||
[[Interstitial Cystitis|Interstitial cystitis]] | [[Interstitial Cystitis|Interstitial cystitis or bladder pain syndrome]], a chronic bladder health problem cause painful urinary tract symptoms; lower abdominal pain, pelvic pain, sudden need to evacuate, or an increase in urination frequency at night. | ||
== | == Physical Therapy == | ||
[[Pelvic Floor Exercises|Pelvic floor physical therapist]] concerned to deal with different conditions associated with urinary bladder or any pelvic floor disorders. Every condition even every case has its own program. Pelvic rehabilitation program will vary between biofeedback training, electrotherapy modalities, exercise programs and mainly concentrate on [[Pelvic Floor Anatomy|pelvic floor muscle]], [[Bladder and bowel management in individuals with SCI|bladder training.]] | |||
== Resources == | == Resources == | ||
Latest revision as of 18:44, 29 June 2023
Original Editor - Khloud Shreif
Top Contributors - Khloud Shreif and David Olukayode
Description[edit | edit source]
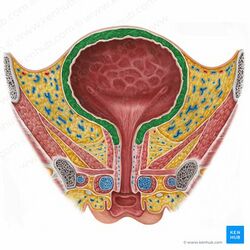
It is a hollow muscular, elastic, subperitoneal organ, , located at the lesser pelvic cavity, it collects the urine that is filtered through the kidney through ureters to be evacuated/ voided later on.
It can accommodate about 1000 ml of urine with an average of about 400-600 ml which varies from one to another. The outer layer of the bladder wall is formed of smooth involuntary muscle fibers (detrusor muscles), it contracts at urination to empty the bladder.
Anatomical Surface of The Bladder[edit | edit source]
When it is filled it is like an oval, formed of four surfaces. The neck is the constricted part, located inferiorly, and leads to the urethra. The apex is anterosuperior and points to the abdominal wall. The base/ fundus is located posteriorly, it is triangular-shaped its tip points backward. The body of the bladder is the main part of the bladder and is located between the apex and fundus[1].
The trigon is a triangular region at the base of the bladder, lined with smooth muscle, collagen, and elastin to a lesser degree. Located between the internal-urethral meatus and the two ureteral orifices[2].
Urethral Sphincters[edit | edit source]
Internal urethral sphincter
It is formed of smooth involuntary muscle fibbers under the control of the autonomic nervous system, it contains alpha-adrenergic receptors its stimulation helps to fill the bladder. In females, it is formed by the bladder neck and the proximal urethra (the urethra in females is about 4 -5 cm while in males it is bout 20cm in length)[4].
External urethral sphincter
It is consisted of skeletal muscle fibers, it is under voluntary control, and contains nicotinic receptors[4].
Innervation[edit | edit source]
Nerve[edit | edit source]
Parasympathetic (s2-s4): responds to stretch receptors of the bladder wall and it is responsible for detrusor contraction to empty the bladder. The pudendal nerve is a somatic parasympathetic that innervates the external urethral sphincter and helps to voluntary control the emptying of the bladder.
Sympathetic (t12-l2): store the urine as it causes relaxation of the detrusor muscle of the bladder.
Artery[edit | edit source]
Branches from internal iliac artery; superior and inferior vesicle arteries.
Small branches from the obturator and inferior gluteal artery.
Lymphatic Drainage[edit | edit source]
The neck and fundus of the bladder through internal, sacral, and common iliac lymph nodes.
The superolateral aspect of the bladder is through the external iliac lymph nodes.
Clinical Relevance[edit | edit source]
Urinary incontinence an involuntary loss of urine it is divided into subtypes; stress incontinence in which patients loss control when there is an increase in intraabdominal pressure, or sudden need to urinate as in urg incontinence and overactive bladder OAB that is associated with increase frequency of urination than normal and may be associated with urgency and named wet OAB.
Atonic bladder(overflow incontinence) there is continuous loss of urine when there is insufficient contraction of detrusor muscle.
Automatic (a spastic bladder) associated with spinal cord injury above the sacral level and associated with frequent urination.
Detrusor sphincter dyssynergia (DSD), there is a spontaneous contraction of both urethral sphincter and detrusor muscle[5].
Interstitial cystitis or bladder pain syndrome, a chronic bladder health problem cause painful urinary tract symptoms; lower abdominal pain, pelvic pain, sudden need to evacuate, or an increase in urination frequency at night.
Physical Therapy[edit | edit source]
Pelvic floor physical therapist concerned to deal with different conditions associated with urinary bladder or any pelvic floor disorders. Every condition even every case has its own program. Pelvic rehabilitation program will vary between biofeedback training, electrotherapy modalities, exercise programs and mainly concentrate on pelvic floor muscle, bladder training.
Resources[edit | edit source]
- ↑ Shermadou ES, Rahman S, Leslie SW. Anatomy, abdomen and pelvis, bladder.2018.
- ↑ Hickling DR, Sun TT, Wu XR. Anatomy and physiology of the urinary tract: relation to host defense and microbial infection. Urinary tract infections: Molecular pathogenesis and clinical management. 2017 Feb 15:1-25.
- ↑ Anatomic Wisdom. General Features of the Urinary Bladder . Available from: http://www.youtube.com/watch?v=UkTG6ncnZFg [last accessed 3/2/2023]
- ↑ 4.0 4.1 Sam P, Jiang J, LaGrange CA. Anatomy, abdomen and pelvis, sphincter urethrae. InStatPearls [Internet] 2021 Nov 5. StatPearls Publishing.
- ↑ Dorsher PT, McIntosh PM. Neurogenic bladder. Advances in urology. 2012 Oct;2012.