Cervical Instability
Original Editor - Mary-Kate McCoy, Heather Lampe as part of the Temple University Evidence-Based Practice Project
Top Contributors - Vanbeylen Antoine, Mary-Kate McCoy, Rachael Lowe, Admin, Pieter Piron, Sara Evenepoel, David Herteleer, Kim Jackson, Lucinda hampton, Heather Lampe, Laura Ritchie, Nick Van Doorsselaer, Daniele Barilla, WikiSysop, Simisola Ajeyalemi, Tony Lowe, Scott A Burns, 127.0.0.1, Jess Bell, Olajumoke Ogunleye, Beth Potter and Evan Thomas
Definition/Description[edit | edit source]
Clinical instability of the cervical spine is defined as the inability of the spine under physiological loads to maintain its normal pattern of displacement so that there is no neurological damage or irritation, no development of deformity, and no incapacitating pain.[1]
Clinically Relevant Anatomy[edit | edit source]
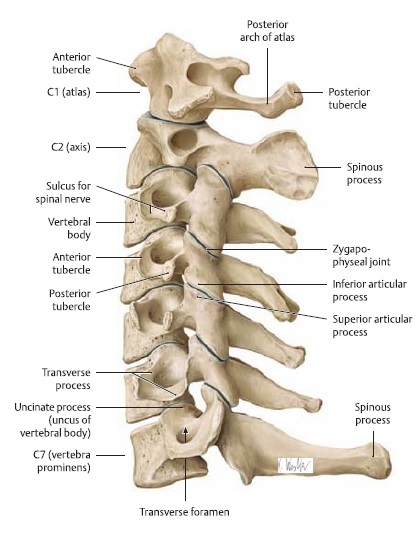
The cervical spine consist of 7 separate vertebrae. The first two vertebrae (referred as upper cervical spine) are highly specialised and differ from the other 5 cervical vertebrae (lower cervical) regarding anatomical structure and function.
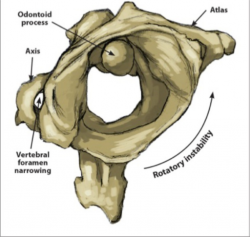
The upper cervical spine is made of the atlas (C1) and the axis (C2). It comprises of two joint structures: one in between os occipital and atlas (atlanto-occipital joint), the other one between atlas and axis, which forms the atlanto-axial joint. The atlantoaxial joint is responsible for 50% of all cervical rotation; the atlanto-occipital joint is responsible for 50% of flexion and extension. [2]
The craniocervical junction (atlanto-occipital joint), the lower atlanto-axial joint and other cervical segments are reinforced by internal as well as external ligaments. They secure the spinal stability of the cervical spine as a whole, together with surrounding postural muscles and allow cervical motion. They also provide proprioceptive information throughout the spinal nerve system to the brain.
The cervical spine has sacrificed stability for mobility and is therefore vulnerable to injury. The orientation of the cervical spine facet joints means the cervical spine is designed for a great deal of mobility, but it lacks stability. The nonlinear displacement curve of the spine, the total range of motion of a spinal segment may be divided into the neutral zone and the elastic zone[1]:
- Neutral zone: motion occurring in this zone is produced against a minimal passive resistance.
- Elastic zone: motion occurring in occurring near the end-range of spinal motion is produced against increased passive resistance.
There are many authors that identified common components of spinal stability. Panjabi[3] conceptualised the components into 3 functionally integrated subsystems of the spinal stabilising system[1][4]:
The passive subsystem:
- Consists of vertebral bodies, facet joints and capsules, spinal ligaments (lig. longitudinale anterius and posterius, ligamentum interspinosum, lig. Interspinosus and lig. Flavum).[5]
- Passive tension from spinal muscles and tendons.
- Provides significant stabilization of the elastic zone and limits the size of the neutral zone.
- Acts as a transducer and provides the neural control subsystem with information about vertebral position and motion
The active subsystem:
- Consists of spinal muscles and tendons, such as: multifidus cervicis, Longus capitis and the Longus Colli.[6]
- Generates forces required to stabilize the spine in response to changing loads.
- Controls the motion occurring within the neutral zone and contributes to maintain the size the size of the neutral zone.
- Acts also as a transducer by providing the neural control subsystem with information about the forces generated by each muscle.
The neural control subsystem:
- Consists of peripheral nerves and the central nervous system.
- Receives information from the transducers of the passive and active subsystems about vertebral position, vertebral motion, and forces generated by spinal muscles. The subsystem determines the requirements for spinal stability and acts on the spinal muscles to produce the required forces.
Clinical instability of the spine occurs when the neutral zone increases relative to the total ROM, the stabilizing subsystems are unable to compensate for this increase, which causes a poor and uncontrolled quality of motion in the neutral zone. [7][8][9] Degeneration and mechanical injury of the spinal stabilisation components are the primary causes of increases in neutral zone size.
Epidemiology /Etiology[edit | edit source]
It is generally accepted that cervical instability is caused by trauma (one major trauma or repetitive microtrauma). Cervical instability can also be a cause of delayed or missed diagnosis of cervical spine injury occurred after trauma (car accident, high impact on the neck) . The traumatic flexion-extension moment exerted on the spine can cause ligamentous disruption with subsequent atlantoaxial instability (AAI) also known as upper cervical instability[10]. Although this occurs in very rare case its incidence is between 4.9 to 20%.[10]
Cervical instability is often diagnosed in patients with rheumatoid arthritis, due to the progressive destruction of the cervical skeletal structures. The most affected region is the upper cervical spine and C4-C5. [11]
Congenital deviation (eg, down syndrome) also can cause upper cervical spine instability. The atlanto-axial instability (AAI) is considered as a developmental anomaly often occurring in patient with the down’s syndrome (DS). It affects 6.8 to 27% of the population with DS.[12] Usually, persons with congenital anomalies do not become symptomatic before midlife adulthood. The spine is assumed to be able to accommodate differing regions of hypermobility and fusions. With time, the degenerative changes occurring in the lower cervical spine increase rigidity and alter the balance. This gradual loss of motion places increasing loads on the atlantoaxial articulation
The following risk factors are associated with the potential for bony or ligamentous compromise of the upper cervical spine[13]:
- History of trauma (e.g. whiplash, rugby neck injury)
- Throat infection
- Congenital collagenous compromise (e.g. syndromes: Down’s, Ehlers-Danlos, Grisel, Morquio)
- Inflammatory arthritides (e.g. rheumatoid arthritis, ankylosing spondylitis)
- Recent neck/head/dental surgery.
Causes of cervical deformity/instability:
- Congenital and developmental cervical deformities
- Neoplastic cervical deformities
- Neurologic abnormalities
- Metabolic and degenerative cervical deformities
- Inflammatory- induced cervical deformities
- Infection- induced cervical deformities
- Iatrogenically induced cervical deformities
- Traumatically induced deformities
Characteristics/Clinical Presentation[edit | edit source]
Aberrant motions occurring in the mid-ranges of active cervical movement are cardinal signs of cervical clinical instability[1]
Symptoms can be different but the most frequent clinical findings are[1]:
- Tenderness in the cervical region
- Referred pain in the shoulder or paraspinal region
- Cervical radiculopathy
- Cervical myelopathy
- Headaches
- Paraspinal muscle spasm
- Decreased cervical lordosis
- Neck pain with sustained postures
- Hypermobility and soft end-feeling in passive motion testing
- Poor cervical muscle strength (multifidus, longus capitis, longus colli)
Differential Diagnosis[edit | edit source]
It’s important to remember that problems in de neck region can be masked by problems in other regions of the body. A frozen shoulder (adhesive capsulitis) for example can be seen in conjunction with a cervical radiculopathy. Other shoulder pathologies such as brachial plexitis can also cause pain and weakness of muscles in the shoulder-neck-region. [LOE 5].
Certain Patients that might present acute neurologic symptoms that raise alarm for cervical compression or neck pain but without a specific origin should undergo a thorough physical examination and radiographic evaluation to determine the source.
More often than not are the findings nonspecific and can be representative of any number of related conditions. Neck pain, weakness and other characteristics also present in cervical spine instability can also be seen in the following cervical diseases including the following: [13][14]
- Cervical strain
- Cervical trauma or fracture
- Occipital headaches
- Degenerative disease of the spine
- Previously undiagnosed syndrome
- Neurological involvement
- Progressive neck pain
- Resistant neck pain
- Central or lateral disc herniation
- Guillain-Barré syndrome
- Cervical spondylosis
- Pathologic fracture
- Cervical canal stenosis
- Facet joint pathologies
- Infections: discitis, osteomyelitis, etc.
Diagnostic Procedures[edit | edit source]
Cervical instability is a diagnosis based primarily on a patient’s history and reported symptoms.
Imaging
Objective criteria have been established in the analysis of end-range flexion and extension radiographs to diagnose cervical spine instability[15]. However, radiographs do not provide information about the quantity or quality of motion in the neutral zone (ie, mid-range), which limits their value in the diagnosis of cervical spine clinical instability[1].
There is often little correlation between the degree of instability or hypermobility shown on radiographic studies and clinical symptoms. Even after severe whiplash injuries, plain radiographs are usually normal despite clinical findings indicating the presence of soft tissue damage. [16]
MRI images could be useful to screen the integrity of the vertebral ligaments. Taking images during an anterior shear test or a distraction test shows a greater intervertebral distance and an increase in direct length of the ligaments[17].
However, functional computerized tomography (fCT) and magnetic resonance imaging (fMRI) scans and digital motion x-ray (DMX) are able to adequately depict cervical instability pathology . Studies using fCT for diagnosing soft tissue ligament or post-whiplash injuries have demonstrated the ability of this technique to show excess atlanto-occipital or atlanto-axial movement during axial rotation . This is especially pertinent when patients have signs and symptoms of cervical instability, yet have normal MRIs in a neutral position.
Functional imaging technology, as opposed to static standard films, is necessary for adequate radiologic depiction of instability in the cervical spine because they provide dynamic imaging (flexion and extension images of the spine) of the neck during movement and are helpful for evaluating the presence and degree of cervical instability.[18][19] (LOE 2B)
Examination
Cook et al[13] tired to obtain consensus of symptoms and physical examination findings associated with clinical cervical spine instability. The study resulted in a list of 16 symptoms and 12 physical examination findings that is associated with CCSI.
The related symptoms listed in descending rank of relationship are:
- Intolerance to prolonged static postures
- Fatigue and inability to hold head up
- Better with external support, including hands or collar
- Frequent need for self-manipulation
- Feeling of instability, shaking, or lack of control
- Frequent episodes of acute attacks
- Sharp pain, possibly with sudden movements
- Head feels heavy
- Neck gets stuck, or locks, with movement
- Better in unloaded position such as lying down
- Catching, clicking, clunking, and popping sensation
- Past history of neck dysfunction or trauma
- Trivial movements provoke symptoms
- Muscles feel tight or stiff
- Unwillingness, apprehension, or fear of movement
- Temporary improvement with clinical manipulation
The 12 physical examination findings included:
- Poor coordination/neuromuscular control, including poor recruitment and dissociation of cervical segments with movement
Abnormal joint play Motion that is not smooth throughout range (of motion), including segmental hinging, pivoting, or fulcruming Aberrant movement Hypomobility of upper thoracic spine Increased muscle guarding, tone, or spasms with test movements Palpable instability during test movements Jerkiness or juddering of motion during cervical movement Decreased cervical muscle strength Catching, clicking, clunking, popping sensation heard during movement assessment Fear, apprehension, or decreased willingness to move during examination Pain provocation with joint-play testing Motion disparity between AROM and PROM Poor posture; postural deviations Decreased AROM in weight bearing Need to support head during examination movements Positive radiographic evidence Palpable segmental changes, such as step-off at C5-C6 Positive ligament shear test Painful arc, including through range of pain Forward head posture Positive test for transverse ligament of atlas Hypomobility of upper cervical spine Positive Alar Ligament Stress Test Positive Sharp-Purser Test Pain at end range of movement Positive VBI tests
Magee et al reported poor cervical muscle endurance is one of the clinical findings we find with cervical instability. A good way to test these muscles (the deep cervical flexor muscles, the longus capitis and longus colli) is the craniocervical flexion test (CCFT). The CCFT could be described as a test of neuromotor control.
The features that are tested are the activation and isometric endurance of the deep cervical flexors as well as their interaction with the superficial cervical flexors (the sternocleidomastoid and the anterior scalene) during the performance of five progressive stages of increasing craniocervical flexion range of motion. It is a low-load test performed in the supine position with the patient guided to each stage by feedback from a pressure sensor placed behind the neck. While the test in the clinical setting provides only an indirect measure of performance, the construct validity of the CCFT has been verified in a laboratory setting by direct measurement of deep and superficial flexor muscle activity. If the 5 stages can’t be completed by the patient, the deep cervical flexor muscles need to be trained. [20]
Outcome Measures[edit | edit source]
To measure chronic neck pain we can use the neck disability index, the neck bournemouth questionnaire or the neck pain and disability scale. These three questionnaires are specific and valid instruments to evaluate the neckpain and dysfunction. [21][22]
The pain catastrophizing scale can be used to evaluate how the patient experiences the pain. It measures the rumination, magnification and helplessness of the patient. [22]
- Symptoms
There is a large agreement on following symptoms to make a clinical judgment on CCSI: “intolerance to prolonged static postures,” “fatigue and inability to hold head up,” “better with external support, including hands or collar,” “frequent need for self-manipulation,” “feeling of instability, shaking, or lack of control,” “frequent episodes of acute attacks,” and “sharp pain, possibly with sudden movements.” [10] Level of evidence: 4
- Physical examination
The physical examination findings related to cervical instability that reached the highest consensus among specialists included “poor coordination/neuromuscular control, including poor recruitment and dissociation of cervical segments with movement,” “abnormal joint play,” “motion that is not smooth throughout range (of motion), including segmental hinging, pivoting, or fulcruming,” and “aberrant movement.” [10]
- Radiography
All initial evaluations of cervical spine injuries should begin with plain radiographs. A variety of other imaging modalities may also be used, such as conventional tomography, CT, and MRI. An appropriate choice has to be made quickly to make a diagnosis of cervical trauma. When cervical trauma exists, it may be at multiple levels, justifying the fact that if treatment is to be instituted, imaging should include the upper and lower cervical hinges. The quality of the standard radiographs varies greatly; their negative quality and predictive value decreases when the severity of the injury increases. [1,2,3,4,5,6,7]
Examination[edit | edit source]
Little is known about the diagnostic accuracy of upper cervical spine instability tests.
One study proposed different identifiers for cervical spine instability. They divided them into different categories: movements, descriptive components, and postures. Patients also experienced neurological problems and headaches. [15] [LOE 5]
Movements: [13][LOE 5]
The neck locks when doing certain movements
A sharp pain can be provoked by certain movements
Banal movements provoke symptoms out of proportion
Patients are not willing to move their neck into areas beyond their confort zone
Descriptive components: [13][1][LOE 5,4]
History of a trauma or neckdysfunction(cervicogenic headaches, chronic whiplash dysfunction, rheumatoid arthritis, osteoarthritis, and segmental degeneration)
Supporting the neck with a brace or hands causes relief of symptoms
The neck feels instable
Catching or clicking sensation when moving the neck
The musculature of the neck feels stiff
The pain is worse at the end of the day
Postures: [1][LOE 4]
Neckpain or headaches provoked by static weightbearing postures
Relieved by non-weightbearing postures
Cook et al.(2005) listed the related physical examination findings in descending rank of relationship. These findings are:
- Poor coordination/neuromuscular control, including poor recruitment and dissociation of cervical segments with movement
- Abnormal joint play
- Motion that is not smooth throughout range (of motion), including segmental hinging, pivoting, or fulcruming
- Aberrant movement
- Hypomobility of upper thoracic spine
- Increased muscle guarding, tone, or spasms with test movements
- Palpable instability during test movements
- Jerkiness or juddering of motion during cervical movement
- Decreased cervical muscle strength
- Catching, clicking, clunking, popping sensation heard during movement assessment
- Fear, apprehension, or decreased willingness to move during examination
- Pain provocation with joint-play testing
The following tests can be used to measure cervical instability[23]:
- Craniocervical flexion test
- Sharp-Purser test
- Upper cervical flexion test
- Cervical flexion-rotation test
- Transverse Ligament Stress Test
- Neck Flexor Muscle Endurance Test
- Spurling's Test
The craniocervical flexiontest is a test to measure the isometric endurance of the deep cervical flexors. The main goal of the test is to aply an isometric force on a pressure sensor placed behind the neck without using the superficial cervical flexors. The construct validity of the craniocervical flexiontest has ben verified in a laboratory setting. [24][LOE 5]
Deep cervical flexor electromyographic activity was recorded with custom electrodes inserted via the nose and fixed by suction to the posterior mucosa of the oropharynx. Surface electrodes were placed over the superficial neck muscles (sternocleidomastoid and anterior scalene). Root mean square electromyographic amplitude and craniocervical flexion range of motion was measured during five incremental levels of craniocervical flexion in supine. After this we can conclude there is a strong linear relation between the electromyographic amplitude of the deep cervical flexor muscles and the incremental stages of the craniocervical flexion test for control and individuals with neck pain. These data confirm that reduced performance of the cranio cervical flexion test is associated with dysfunction of the deep cervical flexor muscles and support the validity of this test for patients with neck pain. [25](LOE 3B)
The sharp-Purser test listed in Gregory Uitvlugt et al is a useful clinical examination to diagnose atlantoaxial instability. We assessed the validity of the Sharp-Purser test in 123 outpatients with rheumatoid arthritis. Our findings indicate a predictive value of 85% and a specificity of 96%. The sensitivity was 88% when subluxation was > 4 mm. [26] (LOE 2B)
Medical Management[edit | edit source]
In the past few decades nonoperative maneuvers like traction, cast immobilization and long periods of bed rest had been replaced by the use of instrumentation to stabilize the spine after a trauma. This method can reduce the risk of negative sequelae of long term bed rest[27]. The cervical stability can be received by using posterior fixation such as lateral mass plating, processus spinosus or facet wiring and cervical pedicle screws. The choice of which fixation is best, can be made by the surgeon after seeing a CT-scan or MRI. In a retrospective study of Fehlings, the cervical spine stabilization was successful in 93% off the cases[28]. Obviously this fixation procedure also holds some risks. It is possible that the spinal cord, vertebral artery, spinal nerve and facet joints get injured. Levine et al. reported radicular symptoms in 6 of their 72 patients[29].
Physical Therapy Management[edit | edit source]
The goal of the physical treatment is to enhance the function of the spinal stabilizing subsystems and to decrease the stresses on the involved spinal segments.
• Posture education and spinal manipulation:
- Decreases stresses on the passive subsystem.
- Proper posture: reduces the loads placed on the spinal segments at end-ranges and returns the spine to a biomechanically efficient position.
- Spinal manipulation can be performed on hypomobile segments above and below the level of instability, what eventually will result in a distribution of the spinal movement across several segments. Also the mechanical stresses on the level of clinical instability are believed to be decreased. [10] Level of Evidence 4
- Video over joint mobilization: https://www.youtube.com/watch?v=Rn1Ed2SxTx0
• Strengthening exercises:
- Enhances the function of the active subsystem.
- The cervical multifidus may provide stability via segmental attachments to cervical vertebrae.
- The m. longus colli and capitus provide anterior stability.
- Strengthening the stabilizing muscles may enable those muscles to improve the quality and control of movement occurring within the neutral zone.[10] Level of Evidence 4, [13] Level of Evidence 2B
• Exercise video: Neck strength and stability www.youtube.com/watch
In a more specific situation such as post-operative revalidation for example in the case of a cervical fusion, the treatment can differ as described hereunder.
• The patient is not required to wear a brace. After 6 weeks it is not encouraged to do any lifting more than 4kg as also overhead work. The rehabilitation begins at week 6, mostly a basic stability exercises program. No cervical strengthening or ranges of motion exercises are encouraged in the first 6 months.
The exercises or mainly focused on the neutral postural alignment, were the patients are recommended to us there trunk, hips and chest to produce proper cervical alignment. For other types of operations the treatment-plan will be defined in function of the critical nature of the trauma.[19]Level of Evidence 5
The use of posture education and spinal manipulation may be used to decrease stress on the passive subsystem. Spinal manipulation can be performed on hypomoblie spinal segments above and below the instability level. It is believed that with those manipulations the spinal movement is more evenly distributed across the segments and that mechanical stress on clinical instability is decreased.
By using proper posture the loads placed on spinal segments is reduced at end-ranges. The spine can return to his biomechanically efficient position. [3][1]
To enhance the function of the active subsystem the physiotherapist will use strengthening exercises for the spinal region. The multifidus and the transversus abdominis play a role in the lumbar stabilization. Some have hypnotized that an analogy could be made between the cervical and lumbar multifidus and between the m. longus coli and m. longus capitis and the transversus abdominis.[3][1]
One of the main goals of the non-surgical treatment is to improve the quality of controlled motion. Therefore proprioception exercises must be used, this will improve the control of movement in the neutral zone. Another important goal is to decrease the stress on the cervical region, using soft tissue techniques. By achieving these goals surgery may be prevented.[3][1]
Kenneth A. Olson (2001) used the following exercises for his case study.[1] (LOE: 3B)
Therapeutic manipulations (mostely for headache)[1] (LOE: 3B):
| Type | Description |
|---|---|
|
Grade I oscillation |
Small amplitude movement performed at the beginning of range |
|
Grade II oscillation |
Large amplitude movement performed within the range but not reach- ing the'limit of the range |
|
Grade III oscillation |
Large amplitude movement performed up to the limit of the range |
|
Grade IV oscillation |
Small amplitude movement performed at the limit of the range. |
|
High velocity thrust |
When a sudden high velocity, short amplitude motion is delivered at the pathological limit of an accessory motion |
|
Isometric |
Where the patient's muscles are used to mobilize the joint by performing an isometric contraction against the operator's resistance |
- Second rib manipulation using supine thrust technique
- Upper thoracic manipulation (high-velocity thrust)
- Cervical facet joint upglide manipulation (grade IV)
- Suboccipital distraction with C2 stabilization
- Upper thoracic rotation manipulation (grade III)
Active exercise therapy [1](LOE: 3B):
- Partial suboccipital nod with a head lift in supine to strengthen the longus capitus and longus colli muscles[12] (LOE: 3B):
The patient lies on his back with his head on the table/a pillow. He nods and hold this position as he lift his head off the table/pillow. This position is hold during 2-3 seconds and then the patient lowers his head back on the table/pillow. 3-4 sets of 10 repetitions were performed.
- Active suboccipital nodding:
The patient lies on his back with a pillow under his head and nods. The physiotherapist applies a little resistance to prevent the patient to perform a neck flexion. The patient is then asked to bend his neck from a neutral position to the point of first resistance and then return to a neutral position. The patient is instructed to keep her head on the pillow throughout performance of the exercise. 3-4 sets of 10 repetitions were performed.
- Craniovertebral sidebending isometric manipulation:
With the patient in supine, head resting on a low pillow, passively position the cran- iovertebral region into right sidebending to the point of resistance to the motion. Manually resist further right sidebending by applying manual pressure above the right ear as the patient holds isometrically for 10 seconds. Passively reposition the patient into further right sidebending if the passive motion has improved, and then reapply the isometric force for 10 seconds. This sequence is repeated 3-4 times in 1 session.
- Quadruped position arm lift with spinal stabilization.
3-4 sets of 10 repetitions were performed.
All those exercises can be performed at home. In adittion the patient recieved controlled opening exercises for the mandible that would be repeated 5- 6 times, 5-6 times per day as home training.
Anita R. Gross et al listed an evidence-based home neck care exercise program that exists in 3 progressive phases. These exercises should be judiciously tailored to individual circumstances and applied as indicated based on a clinical examination. These exercices can be included if the CCFT test was found positive. [30](LOE 5)
Phase 1
- Craniocervical flexion
Start with pressure biofeedback inflated to 20 mmHg. Make sure your chin and forehead are lined up. Nod your head, keeping the large neck muscles soft and bringing the reading up to 22 mmHg. Work up to ten 10-second holds. Then progress to 24, 26, and 28 mmHg.
- Neck active range of motion
Start with your head in neutral, then:
- Tilt backward
- Bend forward
- Tilt side to side
- Turn side to side
- Resisted shoulder extension with elbow flexed
“Set” your cervical spine, abdominals and scapulae, then extend your arm with elbows bent backward.
- Resisted shoulder extension with elbow straight
“Set” your cervical spine, abdominals, and scapulae, then extend your arm backward.
- Resisted shoulder shrug
“Set” your cervical spine, abdominals, and scapulae, then slightly abduct arms and minimally shrug shoulders.
- Resisted elbow exercise
“Set” your cervical spine, abdominals, and scapulae, then:
- Bend
- Straighten level 1
- Straighten level 2 your elbows.
Phase 2
- Headlift
Start with your head in neutral (chin and forehead lined up), do a chin nod and lift your head, while maintaining your chin tucked. Hold for a count of 5 to 10 seconds and return smoothly with your chin still tucked.
- Isometric neck strength
Place your hand on your head and resist:
- Bending
- Tilting backward
- Tilting sideways
- Turning your head
Hold for a count of 5 to 10 seconds.
- Shoulder stretches
“Set” your cervical spine, abdominals, and scapulae,
- Clasp your hands behind your back and squeeze your scapulae together
- Hold your arms out in front of you and reach forward feeling a stretch between your scapulae
- Reach your arms overhead
Hold for 20 seconds.
- Shoulder stretches
“Set” your cervical spine, abdominals, and scapulae
- With elbows at shoulder level, lean into a corner to feel a stretch in the front of your chest
- With elbows at eye level lean into a corner to feel a stretch
Hold for 20 seconds.
- Transverse abdominus
Tense your lower abdomen by imagining drawing your hip bones together (or apart if that works better), hold for 10 seconds
Then let the 1 leg fall out over a 10-second count
- Wall sit
“Set” cervical spine, transverse abdominus, and scapulae, then slide down the wall into a semi-squat position. Hold for as long as you can, working up to 2 minutes.
Phase 3
- Shoulder strength
“Set” cervical spine, abdominals, and scapulae then “hug a tree.”
- Shoulder strengthen
“Set” cervical spine, abdominals, and scapulae, then elevate arms into a “reverse fly.”
- Resisted neck: craniocervical flexion and oblique flexion
“Set” cervical spine, abdominals, and scapulae, then
- Nod head
- Nod head at a slight oblique angle
- Resisted neck extension
“Set” cervical spine, abdominals, and scapulae:
- First nod your head
- Then tilt your head backward
- The focus of extension is in the lower neck
- Resisted neck side flexion
“Set” cervical spine, abdominals, and scapulae, then tilt head to the side.
- Resisted neck rotation
“Set” cervical spine, transverse abdominus, and scapulae, then rotate head.
In the table below you can find the dosage recommendations for the evidence-based home neck care exercise program.
| Exercise | Equipment used | Load (pain-free or low pain) | Rep | Set | Frequency | Duration |
|---|---|---|---|---|---|---|
| Specific neck
Craniocervical flexors 4 isometric 4 isotonic |
Pressure biofeedback Head weight/self resist Rubber tubing |
3 levels mmHg Pain-free range Yellow/red |
10 20 20 |
1 3 3 |
3/wk |
5 min 15 min 20 min |
| Postural/upper extremity
Isotonic |
Rubber tubing |
Green/ blue |
20 | 3 |
3/wk |
12 min |
|
Trunk Isotonic |
Body weight |
20 | 3 |
3/wk |
12 min | |
|
Stretch Specific neck 5 Scapulothoracic 2 |
N/A N/A |
3 3 |
1 1 |
Daily Daily |
10 min 5 min |
Key Research[edit | edit source]
- Osmotherly PG, Rivett DA, Rowe LJ. The anterior shear and distraction tests for craniocervical instability. An evaluation using magnetic resonance imaging. Man Ther. 2012 Oct;17(5):416-21. Level of evidence: 1B
- Kandziora F, Pflugmacher R, Scholz M, Schnake K, Putzier M? Khodadadyan-Klostermann C, Haas NP. Posterior stabilization of subaxial cervical spine trauma: indications and techniques. Injury 2005 Jul;36 Suppl 2:B36-43. Level of Evidence 1A
- Ebraheim N. Posterior lateral mass screw fixation: anatomic and radiographic considerations. The University of Pennsylvania Orthopaedic Journal 12: 66-72, 1999. Level of evidence: 1A
- Ralph E. Gay; Comparison of the Neck Disability Index and the Neck Bournemouth Questionnaire in a sample of patients with chronic uncomplicated neck pain; Journal of Manipulative and Physiological Therapeutics Volume 30, Issue 4, May 2007, Pages 259–262 Level of evidence: 1B
- Steven J Linton; A cognitive-behavioral group intervention as prevention for persistent neck and back pain in a non-patient population: a randomized controlled trial; Volume 90, Issues 1–2, 1 February 2001, Pages 83–90 Level of evidence: 1B
- Steven J Linton, A cognitive-behavioral group intervention as prevention for persistent neck and back pain in a non-patient population: a randomized controlled trial; Volume 90, Issues 1–2, 1 February 2001, Pages 83–90 Level of evidence: 1B
- P.G. Osmotherly et Al., Knowledge and use of craniovertebral instability testing by Australian physiotherapists, Elsevier, 2011. Level of Evidence 2B
Resources
[edit | edit source]
- K.A. Olson, D. Joder, Diagnosis and treatment of Cervical Spine Clinical Instability, Journal of Orthopaedic & Sports Physical Therapy, April 2001. [10] Level of Evidence 4
Clinical Bottom Line[edit | edit source]
Clinical cervical spine instability (CCSI) is controversial and difficult to diagnose. Within the literature, no clinical or diagnostic tests that yield valid and reliable results have been described to differentially diagnose this condition. [10]
The screening by tests for upper cervical instability cannot be done accurately at the moment. [11] level of Evidence 2B
Cervical instability describes a wide range of conditions from neck pain and deformation without any clear proof over little malformations too complete failure of intervertebral connection. Some cause pain, damage/irritation to the spinal cord or nerve roots, while others not. Sometimes this condition can be masked by problemes in other regions of the body.
Until there is no existance of a golden standard or acceptable measurement to diagnose cervical instability. Nowadays a combination of clinical findings and X-ray both dynamic and static are used to diagnose cervical instability.
The general causes of this condition are: trauma, rheumatoid arthritis or a tumor.
The sixteen most related symptoms listed in descending rank of relationship are:
- Intolerance to prolonged static postures
- Fatigue and inability to hold head up
- Better with external support, including hands or collar
- Frequent need for self-manipulation
- Feeling of instability, shaking, or lack of control
- Frequent episodes of acute attacks
- Sharp pain, possibly with sudden movements
- Head feels heavy
- Neck gets stuck, or locks, with movement
- Better in unloaded position such as lying down
- Catching, clicking, clunking, and popping sensation
- Past history of neck dysfunction or trauma
- Trivial movements provoke symptoms
- Muscles feel tight or stiff
- Unwillingness, apprehension, or fear of movement
- Temporary improvement with clinical manipulation
The twelve most observed physical examination findings are:
- Poor coordination/neuromuscular control, including poor recruitment and dissociation of cervical segments with movement
- Abnormal joint play
- Motion that is not smooth throughout range (of motion), including segmental hinging, pivoting, or fulcruming
- Aberrant movement
- Hypomobility of upper thoracic spine
- Increased muscle guarding, tone, or spasms with test movements
- Palpable instability during test movements
- Jerkiness or juddering of motion during cervical movement
- Decreased cervical muscle strength
- Catching, clicking, clunking, popping sensation heard during movement assessment
- Fear, apprehension, or decreased willingness to move during examination
- Pain provocation with joint-play testing
The following tests can be used to identief cervical spine instability:
- Transverse ligament stress test
- Sharp-Purser test
- Upper cervical flexion test
- Cervical flexion-rotation test
- Grimmer test
The medical management consists in stabilization of the cervical spine. The cervical stability can be received by using posterior fixation such as lateral mass plating, processus spinosus or facet wiring and cervical pedicle screws.
The physical therapy management is focused on the strengthening of the deep neck muscles, but further research has to be made to investigate the evidence of the existing exercises (described in the physical therapy management).
Recent Related Research (from Pubmed)
[edit | edit source]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 K.A. Olson, D. Joder, Diagnosis and treatment of Cervical Spine Clinical Instability, Journal of Orthopaedic Sports Physical Therapy, April 2001. Level of Evidence 4
- ↑ Windsor, R. “Cervical Spine Anatomy.” Updated april 9, 2013 (http://emedicine.medscape.com/article/1948797-overview#a30)
- ↑ 3.0 3.1 3.2 3.3 Panjabi, M. M. “The Stabilizing System of the Spine. Part II. Neutral Zone and Instability Hypothesis.” Journal of Spinal Disorders 5, no. 4: 390–397, December 1992 (Level of evidence 5)
- ↑ M. Takeshi et Al., Soft-Tissue Damage and Segmental Instability in Adult Patients with Cervical Spinal Cord Injury Without Major Bone Injury, Spine Journal, December 2012.fckLRLevel of Evidence 2B
- ↑ R. Banerjee et Al., Catastrophic Cervical Spine Injuries in the Collision Sport Athlete, Part 1 Epidemiology, Functional Anatomy, and Diagnosis, The American Journal of Sports Medicine, 2004. Level of Evidence 2A
- ↑ W.Platzer, Atlas van de Anatomie, Bewegingsapparaat, Sesam, 1999. Level of Evidence 5
- ↑ Olson, K. A., and D. Joder. “Diagnosis and Treatment of Cervical Spine Clinical Instability.” The Journal of Orthopaedic and Sports Physical Therapy 31, no. 4 (April 2001): 194–206. (Level of evidence: 3B)
- ↑ Choudhary AK, Ishak R, Zacharia TT, Dias MS. Imaging of spinal injury in abusive head trauma: a retrospective study. Pediatr Radiol. 2014 Sep. 44 (9):1130-40.
- ↑ R. Banerjee et Al., Catastrophic Cervical Spine Injuries in the Collision Sport Athlete, Part 1 Epidemiology, Functional Anatomy, and Diagnosis, The American Journal of Sports Medicine, 2004. Level of Evidence 2A
- ↑ 10.0 10.1 Yeo, Chang Gi, Ikchan Jeon, and Sang Woo Kim. “Delayed or Missed Diagnosis of Cervical Instability after Traumatic Injury: Usefulness of Dynamic Flexion and Extension Radiographs.” Korean Journal of Spine 12, no. 3 (September 2015): 146–49 (Level of evidence 3B)
- ↑ Macovei, Luana-Andreea, and Elena Rezuş. “CERVICAL SPINE LESIONS IN RHEUMATOID ARTHRITIS PATIENTS.” Revista Medico-Chirurgicală̆ a Societă̆ţ̜ii De Medici Ş̧i Naturaliş̧ti Din Iaş̧i 120, no. 1 (March 2016): 70–76. (Level of evidence 2B)
- ↑ Myśliwiec, Andrzej, Adam Posłuszny, Edward Saulicz, Iwona Doroniewicz, Paweł Linek, Tomasz Wolny, Andrzej Knapik, Jerzy Rottermund, Piotr Żmijewski, and Paweł Cieszczyk. “Atlanto-Axial Instability in People with Down’s Syndrome and Its Impact on the Ability to Perform Sports Activities - A Review.” Journal of Human Kinetics 48 (November 22, 2015): 17–24. (Level of evidence 2A)
- ↑ 13.0 13.1 13.2 13.3 13.4 Cook C, Brismee JM, Fleming R, et al (2005). Identifiers suggestive of clinical cervical spine instability: a Delphi study of physical therapists. Physical Therapy 85(9):895-906.
- ↑ Magee DJ, Zachazewski JE,Quillen Ws : Cervical spine in Pathology an intervention in Musculoskeletal Rehabilitation p17-63 ,2009, St-Louis, Saunders Elsevier
- ↑ McCracken B, Klineberg E, Pickard B, Wisner DH. Flexion and extension radiographic evaluation for the clearance of potential cervical spine injures in trauma patients. European Spine Journal. 2013 Jul 1;22(7):1467-73.
- ↑ Van Mameren H, Drukker J, Sanches H, Beursgens J. Cervical spine motion in the sagittal plane (I) range of motion of actually performed movements, an x-ray cinematographic study. Eur J Morphol. 1990;28(1): 47–68 (Level of evidence: 2B)
- ↑ Osmotherly PG, Rivett DA, Rowe LJ. The anterior shear and distraction tests for craniocervical instability. An evaluation using magnetic resonance imaging. Man Ther. 2012 Oct;17(5):416-21. Level of evidence: 1B
- ↑ Radcliff K, Kepler C, Reitman C, Harrop J, Vaccaro A. CT and MRI-based diagnosis of craniocervical dislocations the role of the occipitoatlantal ligament. Clin Orthop Rel Res. 2012 (Level of evidence: 2B)
- ↑ Antinnes J, Dvorak J, Hayek J, Panjabi MM, Grob D. The value of functional computed tomography in the evaluation of soft-tissue injury in the upper cervical spine. Eur Spine J. 1994;3: 98–101 (Level of evidence: 2B)
- ↑ Gwendolen AJ et al; Clinical assessment of the deep cervical flexor muscles: the craniocervical flexion test. J Manipulative Physiol Ther 2008 Sep;31(7):525-33. (Level of evidence 2C)
- ↑ Ralph E. Gay; Comparison of the Neck Disability Index and the Neck Bournemouth Questionnaire in a sample of patients with chronic uncomplicated neck pain; Journal of Manipulative and Physiological Therapeutics. Volume 30, Issue 4, May 2007, Pages 259–262 (Level of evidence 1B)
- ↑ 22.0 22.1 Steven J Linton, A cognitive-behavioral group intervention as prevention for persistent neck and back pain in a non-patient population: a randomized controlled trial; Volume 90, Issues 1–2, 1 February 2001, Pages 83–90 (Level of evidence 1B)
- ↑ Hutting N, Scholten-Peeters GG, Vijverman V, Keesenberg MD, Verhagen AP. Diagnostic accuracy of upper cervical spine instability tests: a systematic review.Phys Ther. 2013 Dec;93(12):1686-95. doi: 10.2522/ptj.20130186. Epub 2013 Jul 25.
- ↑ Jull GA; Clinical assessment of the deep cervical flexor muscles: the craniocervical flexion test; J Manipulative Physiol Ther. 2008 Sep;31(7):525-33. (Level of evidence 5)
- ↑ Falla DL, Jull GA, Hodges PW. Patients with neck pain demonstrate reduced electromyographic activity of the deep cervical flexor muscles during performance of the craniocervical flexion test. Spine (Phila Pa 1976). 2004 Oct 1;29(19):2108-14 (Level of evidence: 3B)
- ↑ Gregory Uitvlugt; Clinical assessment of atlantoaxial instability using the sharp-purser test; Arthritis & Rheumatism; nov 2005 (Level of evidence: 2B)
- ↑ Kandziora F, Pflugmacher R, Scholz M, Schnake K, Putzier M? Khodadadyan-Klostermann C, Haas NP. Posterior stabilization of subaxial cervical spine trauma: indications and techniques. Injury 2005 Jul;36 Suppl 2:B36-43. (Level of Evidence IA) Review
- ↑ Kandziora F, Pflugmacher R, Scholz M, Schnake K, Putzier M? Khodadadyan-Klostermann C, Haas NP. Posterior stabilization of subaxial cervical spine trauma: indications and techniques. Injury 2005 Jul;36 Suppl 2:B36-43. Level of Evidence IA
- ↑ Ebraheim N. Posterior lateral mass screw fixation: anatomic and radiographic considerations. The University of Pennsylvania Orthopaedic Journal 12: 66-72, 1999. (Level of evidence Ia) Review
- ↑ Gross R. et al; Knowledge to action: a challenge for neck pain treatment; J Orthop Sports Phys Ther. 2009 May;39(5):351-63 (Level of evidence 5)