Cervical Stenosis: Difference between revisions
Rachael Lowe (talk | contribs) mNo edit summary |
(updated categories - removed course pages) |
||
| (32 intermediate revisions by 7 users not shown) | |||
| Line 3: | Line 3: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
== Definition/Description == | == Definition/Description == | ||
Cervical stenosis is | Cervical stenosis is a narrowing of the cervical spinal canal. This narrowing of the spinal canal may result in compression of the spinal cord and/or the nerve roots and affect the function of the spinal cord or the nerve, which may cause symptoms associated with [[Cervical Radiculopathy|cervical radiculopathy]] or [[Cervical Myelopathy|cervical myelopathy]]. | ||
[[Spinal Stenosis|Spinal stenosis]] may occur as a result of [[Cervical Spondylosis|spondylosis]] (degenerative changes in the cervical spine) but can also be the result of traumatic (fractures and instability) and inflammatory conditions or caused by herniated discs or tumours. | |||
The below 4-minute video brings in the most relevant information | |||
{{#ev:youtube|https://www.youtube.com/watch?v=sWPB0fzX8ao&app=desktop|width}}<ref>Mayo Clinic Cervical spinal stenosis Available from:https://www.youtube.com/watch?v=sWPB0fzX8ao&app=desktop (last accessed 3.2.2020)</ref> | |||
== Clinically Relevant Anatomy == | |||
* See also [[Cervical Anatomy]] | |||
The cervical spinal canal normally provides enough room for the neural elements. The sagittal diameter of the spinal canal varies with height and between individuals. The first cervical vertebral body (C 1) is about 21.8 mm high and the spinal cord makes up about 50% of the spinal canal. On the other hand, C 6 is about 17.8 mm in height and the spinal cord takes up about 75% of the spinal canal<ref name=":4">Meyer F, Börm W, Thomé C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696878/ Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment.] Deutsches Ärzteblatt International. 2008 May;105(20):366.</ref>. | |||
* Average anterior-posterior canal diameter at all levels is 14.1 +/- 1.6 mm. | |||
* The canal diameters range from 9.0 to 20.9 mm, with a median diameter of 14.4 mm. | |||
* Men have significantly larger cervical spinal canals than women at all of the levels<ref name=":8">Lee MJ, Cassinelli EH, Riew KD. [https://www.ncbi.nlm.nih.gov/pubmed/17272453 Prevalence of cervical spine stenosis: anatomic study in cadavers]. JBJS. 2007 Feb 1;89(2):376-80.</ref>. | |||
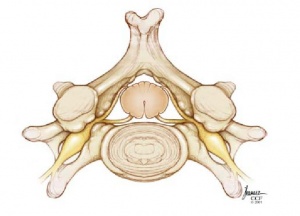
Stenosis is usually the secondary consequences of space-occupying lesions eg: | |||
* Progressive disk degeneration, accompanied by disk protrusion, | |||
* Ventral spondylophyte formation, | |||
* Thickening of the ligamenta flavum | |||
* Hypertrophy of the dorsal facets. | |||
Movement affects the diameter of the spinal canal and cord: | |||
* The diameter of the spinal canal in flexion and extension is reduced. | |||
* During extension, the ligamentum flavum is folded, which further constricts the spinal canal. | |||
* Changes in length of the spinal canal also affect the length of the spinal cord. eg the shortening of the spinal cord in extension is linked to an increase in diameter and can be additionally damaged by movement. It is pinched between the pincers of the posteroinferior end of one vertebral body and the lamina or ligamentum flavum of the caudal segment. .<ref name=":4" /> | |||
{| width="100%" cellspacing="1" cellpadding="1" | {| width="100%" cellspacing="1" cellpadding="1" | ||
|- | |- | ||
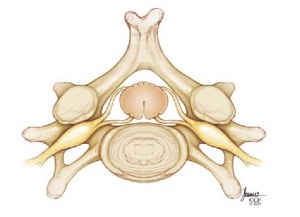
| [[Image:Normal-cervical.jpg|thumb|center | | [[Image:Normal-cervical.jpg|thumb|center|Normal cervical vertebrae]] | ||
| [[Image:Cervica-Stenosis.jpg|thumb|center|Cervical stenosis]] | | [[Image:Cervica-Stenosis.jpg|thumb|center|Cervical stenosis]] | ||
|} | |} | ||
== | === Pathophysiology === | ||
Many theories regarding the pathophysiology of spinal stenosis suggest a number of confluent mechanisms: | |||
* The spinal cord can be directly compressed by osteophytic bones and ligamentous hypertrophy. | |||
* Compression of local vascular structures can lead to ischemia of the spinal cord from arterial insufficiency and venous stasis. | |||
* A herniated disk can exert repeated local trauma to the spinal cord or nerve root during repetitive flexion and extension movements, especially in the unstable spine with multiple levels of subluxations. | |||
* In the cervical spine, segments C5-6 and C6-7 are often affected.<ref name=":0">Raja A, Hanna A, Hoang S, Mesfin FB. [https://www.ncbi.nlm.nih.gov/books/NBK441989/ Spinal Stenosis] dec 2019.Available from:https://www.ncbi.nlm.nih.gov/books/NBK441989/ (last accessed 3.2.2020)</ref> | |||
== Epidemiology == | |||
Cervical spine stenosis appears to be very common and it estimated that cervical stenosis is present in: | |||
* 4.9% of the adult population, | |||
* 6.8% of the population fifty years of age or older | |||
* 9% of the population seventy years of age or older<ref name=":8" />. | |||
Most patients’ symptoms chronically deteriorate over the years however deterioration can occur rapidly and is then mostly irreversible: | |||
* 75% of patients experience phases of neurological deterioration. | |||
* About 5% of all patients with asymptomatic spinal cord compression become symptomatic each year. | |||
* Some patients present with an acute clinical course (mostly patients with significant but asymptomatic stenosis who suffer acute spinal cord compression after a trivial injury)<ref name=":4" />. | |||
Risk factors that lead to the development of spinal stenosis are multifactorial: | |||
* Genetic influence as demonstrated in the study of twins | |||
* Cumulative trauma can lead to the progression of the disease | |||
* Osteoporosis can be a contributing factor | |||
* Cigarette smoking in several epidemiological studies has been shown to lead to back pain and degenerative spinal diseases.<ref name=":0" /> | |||
Cervical stenosis | === Etiology === | ||
Cervical spine stenosis can be caused by a combination of factors. | |||
* Some individuals can have a congenitally narrowed spinal canal that is exacerbated by pathologic factors. | |||
* Disk herniation together with the formation of osteophytic spurs, hypertrophy of the articular facets and ligamentum flavum, and ossification of posterior longitudinal ligaments can lead to central and foraminal stenosis. | |||
* Structural factors such as subluxation from disk and facet joint degeneration and changes in the normal lordotic curvatures of the spine can lead to spinal compression.<ref name=":0" /> | |||
Potential symptoms | == Characteristics/Clinical Presentation == | ||
Initial evaluation of a patient with spinal stenosis often begins with a detailed history of symptoms and physical exam, with a focus on sensation, motor strength, reflexes, and gait.<ref name=":0" /> | |||
* Cervical stenosis does not necessarily cause symptoms, but if symptoms are present they will mainly be caused by associated [[Cervical Radiculopathy|cervical radiculopathy]] or [[Cervical Myelopathy|cervical myelopathy]]. | |||
* Cervical spondylotic myelopathy can be seen in patients with greater than 30% spinal narrowing, leading to [[gait]] disturbance, lower extremity weakness, and [[Coordination Exercises|ataxia]]. | |||
Cervical spinal stenosis can lead to radicular symptoms due to nerve root compression and myelopathy due to spinal cord compression, radicular symptoms are dependent on the level affected eg a C5-6 disk herniation leads to C6 radiculopathy. | |||
* C4-5 [[Disc Herniation|disk herniation]] can lead to deltoid weakness and shoulder paresthesia. Patients also can experience pain and paresthesia in the head, neck, and shoulder. | |||
* C6-7 disk herniation is the most common, leading to a wrist drop and paresthesia in the 2 and three fingers. | |||
* C5-6 disk herniation is the next common, resulting in weakness in forearm flexion and paresthesia in the thumb and radial forearm. | |||
* C7-T1 disk herniation can lead to weakness in the hand intrinsic muscles and numbness in the 4 and five digits.<ref name=":0" /> | |||
Potential symptoms include:<ref name="p1">North American Spine Society Public Education Series. Cervical stenosis and myelopathy. http://www.spine.org/Documents/cervical_stenosis_2006.pdf (Accessed 22 November 2011).</ref><ref name="p2">Williams SK, et al. Concomitant cervical and lumbar stenosis: Strategies for treatment and outcomes. Semin Spine Surg 2007;19(3):165-176.</ref><ref name="p3">Countee RW, et al. Congenital stenosis of the cervical spine: Diagnosis and management. J Natl Med Assoc 1979;71(3):257-264.</ref> | |||
*Pain in neck or arms | *Pain in the neck or arms | ||
*Arm and leg dysfunction | *Arm and leg dysfunction | ||
*Weakness, stiffness or clumsiness in the hands | *Weakness, stiffness or clumsiness in the hands | ||
| Line 76: | Line 80: | ||
*Difficulty walking | *Difficulty walking | ||
*Frequent falling | *Frequent falling | ||
*Urinary urgency which may progress to bladder and bowel [[Urinary Incontinence]] | |||
*Urinary urgency which may progress to bladder and bowel | *Diminished [[proprioception]] | ||
*Diminished proprioception | |||
The progression of the symptoms may also vary: | The progression of the symptoms may also vary in the following ways: | ||
*A slow and steady decline | *A slow and steady decline | ||
*Progression to a certain point and stabilizing | *Progression to a certain point and stabilizing | ||
*Rapidly declining | *Rapidly declining | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* | * [[Diabetes]] | ||
* | * [[Inflammatory Myopathies|Inflammatory spondyloarthropathy]] (e.g., ankylosing spondylitis) | ||
* | * [[Paget's Disease|Paget's disease]] of the bone | ||
*[[ | * Peripheral neuropathy (paralysis) | ||
* | * [[Peripheral Arterial Disease|Peripheral vascular disease]] | ||
* | * [[Disc Herniation|Single level lumbar disc herniation]] | ||
* | * Spinal cord tumor | ||
* | * Vascular insufficiency (atherosclerosis of the aorta and/or leg arteries) | ||
* Vertebral disc disease | |||
== | == Pathophysiology == | ||
Many theories regarding the pathophysiology of spinal stenosis suggest a number of confluent mechanisms. The spinal cord can be directly compressed by osteophytic bones and ligamentous hypertrophy. Compression of local vascular structures can lead to ischemia of the spinal cord from arterial insufficiency and venous stasis. A herniated disk can exert repeated local trauma to the spinal cord or nerve root during repetitive flexion and extension movements, especially in the unstable spine with multiple levels of subluxations. | |||
In the cervical spine, segments C5-6 and C6-7 are often affected | |||
Most patients will experience some type of pain associated with the spine but luckily, even without surgery, the majority will have an uneventful recovery. Only 1-3% will have a herniated disc and less than 2% will have compression of a nerve root. | |||
Spinal stenosis is common with aging but predicting which individual will develop symptoms is not possible. In most cases, the degenerative process can be controlled by changes in lifestyle. | |||
{{#ev:youtube|9n09uGsCEkA|300}} | === Evaluation === | ||
Diagnosis can be made through imaging with extended release x-ray, CT, and MRI. With the availability of MRI, a plain radiograph is of limited value although dynamic views in flexion and extension modes can demonstrate dynamic instability or spondylolisthesis. CT can help differentiate calcified disks or bone osteophytes from “soft disks,” differentiate ossification of the posterior longitudinal ligament from a thickened posterior longitudinal ligament and detect bone fractures or lytic lesions. MRI is the gold standard; it is able to show intrinsic cord abnormalities, the degree of spinal stenosis, and differentiate other conditions such as tumors, hematoma, or infection. If a patient has a pacemaker and cannot obtain an MRI, a CT myelogram can be performed to identify the level and degree of stenosis.{{#ev:youtube|9n09uGsCEkA|300}} | |||
== Outcome Measures == | == Outcome Measures == | ||
<sup></sup> | |||
<sup></sup> | |||
*[[Neck Disability Index]] | *[[Neck Disability Index]] | ||
*[[Neck Pain and Disability Scale]] | *[[Neck Pain and Disability Scale]] | ||
== Medical Management == | |||
Initial treatment can include both conservative and nonsurgical methods. These methods include physical therapy such as stretching, strengthening, and aerobic fitness to improve and stabilize muscles and posture; anti-inflammatory and analgesic medications; and epidural steroid injections<ref name=":5">Foris LA, Varacallo M. [https://www.statpearls.com/kb/viewarticle/29357 Spinal stenosis and neurogenic claudication.] Florida: StatPearls Publishing. 2018. Available from:https://www.statpearls.com/kb/viewarticle/29357 (last accessed 3.2.2020)</ref>. | |||
* Surgery is for only those who fail repeated nonoperative treatments (aimed at improving symptoms and function rather than preventing neurologic complications) and only considered after attempting nonsurgical modalities, or if a patient's symptoms result in disability. | |||
* If a patient presents with rapidly progressive neurological deficits or if there is the presence of bladder dysfunction, urgent surgery is necessary eg cauda equina syndrome, conus medullaris syndrome, trauma, or an intraspinal canal tumor. | |||
* The surgical approach is multilevel decompressive laminectomy with or without lumbar fusion. | |||
* Lumbar fusion is generally reserved for patients with spondylolisthesis.<ref name=":5" /> | |||
== | == Physical Therapy Management == | ||
Nonoperative treatments, such as physical therapy management, are aimed at reducing pain and increasing the patient's function. Nonoperative treatments do not change the narrowing of the spinal canal, but can provide the patient of a long-lasting pain control and improved function without surgery. A rehabilitation program may require 3 or more months of supervised treatment. <ref name="p1" /> | |||
A physical therapy program may include<ref>May, S. & Comer, C. Is surgery more effective than non-surgical treatment for spinal stenosis, and which non-surgical treatment is more effective? A systematic review. Physiotherapy, 2013, 99(1), 12-20</ref>)<ref name=":2">Hu SS, et al. Cervical spondylosis section of Disorders, diseases, and injuries of the spine. In HB Skinner, ed., Current Diagnosis and Treatment in Orthopedics, 4th ed., pp. 238–242. New York: McGraw-Hill.,2006</ref><ref name=":3">Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006; 443:198.</ref> | |||
* Stretching exercises: These exercises are aimed at restoring the flexibility of the muscles of the neck, trunk, arms and legs. | |||
* Manual therapy: Cervical and thoracic joint manipulation to improve or maintain the range of motion. | |||
* Heat therapy: to improve blood circulation to the muscles and other soft tissues. | |||
* Cardiovascular exercises for arms and legs: This will improve blood circulation and enhance the patient's cardiovascular endurance and promote good physical conditioning. | |||
* Aquatic exercises: to allow your body to exercise without pressure on the spine. | |||
* Training of activity of daily living (ADL) and functional movements. | |||
Exercises and techniques that may help relieve symptoms of spinal stenosis and prevent progression of the condition include:<ref name=":1">.Yeh et Al., Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosi, Journal of Orthopaedic Surgery and Research, August 2014</ref><ref name=":2" /><ref name=":3" /> | |||
* Specific strengthening exercises for the arm, trunk and leg muscles. | |||
* Stretching | |||
* Postural re-education | |||
* Scapular stabilization | |||
* Ergonomics and frequent changes of position, to avoid sustained postures that compress the spine | |||
* Planning ahead so that you take breaks in between potentially back-stressing activities such as walking and yard work. | |||
* Proper lifting, pushing, and pulling. | |||
== '''Prognosis''' == | |||
Spinal stenosis has significant morbidity and affects the quality of life. With time it can lead to chronic pain and muscle weakness. In some cases, it may lead to cauda equina syndrome. Patients with central spinal stenosis may have difficulty walking and have gait disturbances. While some patients may improve with time, the majority have a progression of the condition, leading to disability. The cost of managing spinal stenosis is enormous, and for patients can lead to high healthcare bills.<ref name=":5" /> | |||
== References == | |||
<references /> | |||
<br> | <br> | ||
[[Category:Cervical Spine - Conditions]] | |||
[[Category:Vrije_Universiteit_Brussel_Project]] | [[Category:Vrije_Universiteit_Brussel_Project]] | ||
[[Category:Cervical Spine]] | |||
[[Category:Conditions]] | |||
Latest revision as of 11:37, 15 November 2023
Original Editors - Demol Yves as part of the Vrije Universiteit Brussel Evidence-based Practice Project
Top Contributors - Demol Yves, Rachael Lowe, Lucinda hampton, Sara Evenepoel, Kim Jackson, WikiSysop, Nicolas Casier, Simisola Ajeyalemi, Rucha Gadgil, Admin, Daphne Jackson, David Herteleer, Jess Bell, Olajumoke Ogunleye, Tony Lowe and Evan Thomas
Definition/Description[edit | edit source]
Cervical stenosis is a narrowing of the cervical spinal canal. This narrowing of the spinal canal may result in compression of the spinal cord and/or the nerve roots and affect the function of the spinal cord or the nerve, which may cause symptoms associated with cervical radiculopathy or cervical myelopathy.
Spinal stenosis may occur as a result of spondylosis (degenerative changes in the cervical spine) but can also be the result of traumatic (fractures and instability) and inflammatory conditions or caused by herniated discs or tumours. The below 4-minute video brings in the most relevant information
Clinically Relevant Anatomy[edit | edit source]
- See also Cervical Anatomy
The cervical spinal canal normally provides enough room for the neural elements. The sagittal diameter of the spinal canal varies with height and between individuals. The first cervical vertebral body (C 1) is about 21.8 mm high and the spinal cord makes up about 50% of the spinal canal. On the other hand, C 6 is about 17.8 mm in height and the spinal cord takes up about 75% of the spinal canal[2].
- Average anterior-posterior canal diameter at all levels is 14.1 +/- 1.6 mm.
- The canal diameters range from 9.0 to 20.9 mm, with a median diameter of 14.4 mm.
- Men have significantly larger cervical spinal canals than women at all of the levels[3].
Stenosis is usually the secondary consequences of space-occupying lesions eg:
- Progressive disk degeneration, accompanied by disk protrusion,
- Ventral spondylophyte formation,
- Thickening of the ligamenta flavum
- Hypertrophy of the dorsal facets.
Movement affects the diameter of the spinal canal and cord:
- The diameter of the spinal canal in flexion and extension is reduced.
- During extension, the ligamentum flavum is folded, which further constricts the spinal canal.
- Changes in length of the spinal canal also affect the length of the spinal cord. eg the shortening of the spinal cord in extension is linked to an increase in diameter and can be additionally damaged by movement. It is pinched between the pincers of the posteroinferior end of one vertebral body and the lamina or ligamentum flavum of the caudal segment. .[2]
Pathophysiology[edit | edit source]
Many theories regarding the pathophysiology of spinal stenosis suggest a number of confluent mechanisms:
- The spinal cord can be directly compressed by osteophytic bones and ligamentous hypertrophy.
- Compression of local vascular structures can lead to ischemia of the spinal cord from arterial insufficiency and venous stasis.
- A herniated disk can exert repeated local trauma to the spinal cord or nerve root during repetitive flexion and extension movements, especially in the unstable spine with multiple levels of subluxations.
- In the cervical spine, segments C5-6 and C6-7 are often affected.[4]
Epidemiology[edit | edit source]
Cervical spine stenosis appears to be very common and it estimated that cervical stenosis is present in:
- 4.9% of the adult population,
- 6.8% of the population fifty years of age or older
- 9% of the population seventy years of age or older[3].
Most patients’ symptoms chronically deteriorate over the years however deterioration can occur rapidly and is then mostly irreversible:
- 75% of patients experience phases of neurological deterioration.
- About 5% of all patients with asymptomatic spinal cord compression become symptomatic each year.
- Some patients present with an acute clinical course (mostly patients with significant but asymptomatic stenosis who suffer acute spinal cord compression after a trivial injury)[2].
Risk factors that lead to the development of spinal stenosis are multifactorial:
- Genetic influence as demonstrated in the study of twins
- Cumulative trauma can lead to the progression of the disease
- Osteoporosis can be a contributing factor
- Cigarette smoking in several epidemiological studies has been shown to lead to back pain and degenerative spinal diseases.[4]
Etiology[edit | edit source]
Cervical spine stenosis can be caused by a combination of factors.
- Some individuals can have a congenitally narrowed spinal canal that is exacerbated by pathologic factors.
- Disk herniation together with the formation of osteophytic spurs, hypertrophy of the articular facets and ligamentum flavum, and ossification of posterior longitudinal ligaments can lead to central and foraminal stenosis.
- Structural factors such as subluxation from disk and facet joint degeneration and changes in the normal lordotic curvatures of the spine can lead to spinal compression.[4]
Characteristics/Clinical Presentation[edit | edit source]
Initial evaluation of a patient with spinal stenosis often begins with a detailed history of symptoms and physical exam, with a focus on sensation, motor strength, reflexes, and gait.[4]
- Cervical stenosis does not necessarily cause symptoms, but if symptoms are present they will mainly be caused by associated cervical radiculopathy or cervical myelopathy.
- Cervical spondylotic myelopathy can be seen in patients with greater than 30% spinal narrowing, leading to gait disturbance, lower extremity weakness, and ataxia.
Cervical spinal stenosis can lead to radicular symptoms due to nerve root compression and myelopathy due to spinal cord compression, radicular symptoms are dependent on the level affected eg a C5-6 disk herniation leads to C6 radiculopathy.
- C4-5 disk herniation can lead to deltoid weakness and shoulder paresthesia. Patients also can experience pain and paresthesia in the head, neck, and shoulder.
- C6-7 disk herniation is the most common, leading to a wrist drop and paresthesia in the 2 and three fingers.
- C5-6 disk herniation is the next common, resulting in weakness in forearm flexion and paresthesia in the thumb and radial forearm.
- C7-T1 disk herniation can lead to weakness in the hand intrinsic muscles and numbness in the 4 and five digits.[4]
Potential symptoms include:[5][6][7]
- Pain in the neck or arms
- Arm and leg dysfunction
- Weakness, stiffness or clumsiness in the hands
- Leg weakness
- Difficulty walking
- Frequent falling
- Urinary urgency which may progress to bladder and bowel Urinary Incontinence
- Diminished proprioception
The progression of the symptoms may also vary in the following ways:
- A slow and steady decline
- Progression to a certain point and stabilizing
- Rapidly declining
Differential Diagnosis[edit | edit source]
- Diabetes
- Inflammatory spondyloarthropathy (e.g., ankylosing spondylitis)
- Paget's disease of the bone
- Peripheral neuropathy (paralysis)
- Peripheral vascular disease
- Single level lumbar disc herniation
- Spinal cord tumor
- Vascular insufficiency (atherosclerosis of the aorta and/or leg arteries)
- Vertebral disc disease
Pathophysiology[edit | edit source]
Many theories regarding the pathophysiology of spinal stenosis suggest a number of confluent mechanisms. The spinal cord can be directly compressed by osteophytic bones and ligamentous hypertrophy. Compression of local vascular structures can lead to ischemia of the spinal cord from arterial insufficiency and venous stasis. A herniated disk can exert repeated local trauma to the spinal cord or nerve root during repetitive flexion and extension movements, especially in the unstable spine with multiple levels of subluxations.
In the cervical spine, segments C5-6 and C6-7 are often affected
Most patients will experience some type of pain associated with the spine but luckily, even without surgery, the majority will have an uneventful recovery. Only 1-3% will have a herniated disc and less than 2% will have compression of a nerve root.
Spinal stenosis is common with aging but predicting which individual will develop symptoms is not possible. In most cases, the degenerative process can be controlled by changes in lifestyle.
Evaluation[edit | edit source]
Diagnosis can be made through imaging with extended release x-ray, CT, and MRI. With the availability of MRI, a plain radiograph is of limited value although dynamic views in flexion and extension modes can demonstrate dynamic instability or spondylolisthesis. CT can help differentiate calcified disks or bone osteophytes from “soft disks,” differentiate ossification of the posterior longitudinal ligament from a thickened posterior longitudinal ligament and detect bone fractures or lytic lesions. MRI is the gold standard; it is able to show intrinsic cord abnormalities, the degree of spinal stenosis, and differentiate other conditions such as tumors, hematoma, or infection. If a patient has a pacemaker and cannot obtain an MRI, a CT myelogram can be performed to identify the level and degree of stenosis.
Outcome Measures[edit | edit source]
Medical Management[edit | edit source]
Initial treatment can include both conservative and nonsurgical methods. These methods include physical therapy such as stretching, strengthening, and aerobic fitness to improve and stabilize muscles and posture; anti-inflammatory and analgesic medications; and epidural steroid injections[8].
- Surgery is for only those who fail repeated nonoperative treatments (aimed at improving symptoms and function rather than preventing neurologic complications) and only considered after attempting nonsurgical modalities, or if a patient's symptoms result in disability.
- If a patient presents with rapidly progressive neurological deficits or if there is the presence of bladder dysfunction, urgent surgery is necessary eg cauda equina syndrome, conus medullaris syndrome, trauma, or an intraspinal canal tumor.
- The surgical approach is multilevel decompressive laminectomy with or without lumbar fusion.
- Lumbar fusion is generally reserved for patients with spondylolisthesis.[8]
Physical Therapy Management[edit | edit source]
Nonoperative treatments, such as physical therapy management, are aimed at reducing pain and increasing the patient's function. Nonoperative treatments do not change the narrowing of the spinal canal, but can provide the patient of a long-lasting pain control and improved function without surgery. A rehabilitation program may require 3 or more months of supervised treatment. [5]
A physical therapy program may include[9])[10][11]
- Stretching exercises: These exercises are aimed at restoring the flexibility of the muscles of the neck, trunk, arms and legs.
- Manual therapy: Cervical and thoracic joint manipulation to improve or maintain the range of motion.
- Heat therapy: to improve blood circulation to the muscles and other soft tissues.
- Cardiovascular exercises for arms and legs: This will improve blood circulation and enhance the patient's cardiovascular endurance and promote good physical conditioning.
- Aquatic exercises: to allow your body to exercise without pressure on the spine.
- Training of activity of daily living (ADL) and functional movements.
Exercises and techniques that may help relieve symptoms of spinal stenosis and prevent progression of the condition include:[12][10][11]
- Specific strengthening exercises for the arm, trunk and leg muscles.
- Stretching
- Postural re-education
- Scapular stabilization
- Ergonomics and frequent changes of position, to avoid sustained postures that compress the spine
- Planning ahead so that you take breaks in between potentially back-stressing activities such as walking and yard work.
- Proper lifting, pushing, and pulling.
Prognosis[edit | edit source]
Spinal stenosis has significant morbidity and affects the quality of life. With time it can lead to chronic pain and muscle weakness. In some cases, it may lead to cauda equina syndrome. Patients with central spinal stenosis may have difficulty walking and have gait disturbances. While some patients may improve with time, the majority have a progression of the condition, leading to disability. The cost of managing spinal stenosis is enormous, and for patients can lead to high healthcare bills.[8]
References[edit | edit source]
- ↑ Mayo Clinic Cervical spinal stenosis Available from:https://www.youtube.com/watch?v=sWPB0fzX8ao&app=desktop (last accessed 3.2.2020)
- ↑ 2.0 2.1 2.2 Meyer F, Börm W, Thomé C. Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment. Deutsches Ärzteblatt International. 2008 May;105(20):366.
- ↑ 3.0 3.1 Lee MJ, Cassinelli EH, Riew KD. Prevalence of cervical spine stenosis: anatomic study in cadavers. JBJS. 2007 Feb 1;89(2):376-80.
- ↑ 4.0 4.1 4.2 4.3 4.4 Raja A, Hanna A, Hoang S, Mesfin FB. Spinal Stenosis dec 2019.Available from:https://www.ncbi.nlm.nih.gov/books/NBK441989/ (last accessed 3.2.2020)
- ↑ 5.0 5.1 North American Spine Society Public Education Series. Cervical stenosis and myelopathy. http://www.spine.org/Documents/cervical_stenosis_2006.pdf (Accessed 22 November 2011).
- ↑ Williams SK, et al. Concomitant cervical and lumbar stenosis: Strategies for treatment and outcomes. Semin Spine Surg 2007;19(3):165-176.
- ↑ Countee RW, et al. Congenital stenosis of the cervical spine: Diagnosis and management. J Natl Med Assoc 1979;71(3):257-264.
- ↑ 8.0 8.1 8.2 Foris LA, Varacallo M. Spinal stenosis and neurogenic claudication. Florida: StatPearls Publishing. 2018. Available from:https://www.statpearls.com/kb/viewarticle/29357 (last accessed 3.2.2020)
- ↑ May, S. & Comer, C. Is surgery more effective than non-surgical treatment for spinal stenosis, and which non-surgical treatment is more effective? A systematic review. Physiotherapy, 2013, 99(1), 12-20
- ↑ 10.0 10.1 Hu SS, et al. Cervical spondylosis section of Disorders, diseases, and injuries of the spine. In HB Skinner, ed., Current Diagnosis and Treatment in Orthopedics, 4th ed., pp. 238–242. New York: McGraw-Hill.,2006
- ↑ 11.0 11.1 Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006; 443:198.
- ↑ .Yeh et Al., Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosi, Journal of Orthopaedic Surgery and Research, August 2014