Cervical Anatomy
Introduction[edit | edit source]
An expert understanding of cervical anatomy is critical to physiotherapists working in this region. An understanding of this anatomy is essential for assessment and treatment of cervical spine problems.
The cervical spine’s major functions include supporting and cushioning loads to the head/neck while allowing for rotation, and protecting the spinal cord extending from the brain.[1] The cervical spine is subjected to extrinsic factors such as repetitive movements, whole body vibrations and static load. [2]
The cervical spine is the most superior portion of the vertebral column, lying between the cranium and the thoracic vertebrae.
It consists of seven distinct vertebrae, two of which are given unique names:
- The first cervical vertebrae (C1) is known as the atlas.
- The second cervical vertebrae (C2) is known as the axis.
This page is a review of cervical spine vertebrae, joints, ligaments and muscles.
Vertebrae[edit | edit source]
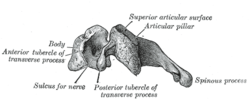
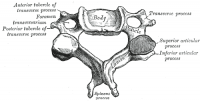
The cervical vertebrae have three main features which distinguish them from other vertebrae:
- Triangular vertebral foramen.
- Bifid spinous process – this is where the spinous process splits into two distally.
- Transverse foramina – holes in the transverse processes. They give passage to the vertebral artery, vein and sympathetic nerves[3].
The main role of the cervical spine is to support and promote the movement of the head and neck.[4] [5]
- Large vertebral bodies are not necessary considering the relatively small weight-bearing load at this level.
- Increased range of motion takes priority over vertebral size and rigidity.
- Additional motion and flexibility may carry an increased risk for injury of the spinal cord and its associated neurovascular structures[4].
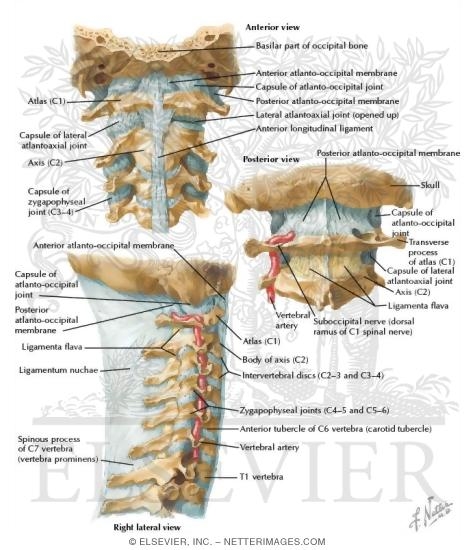
Atlas and Axis[edit | edit source]
The atlas and axis have additional features that mark them apart from the other cervical vertebrae[3].
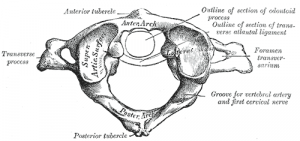
Atlas[edit | edit source]
The atlas is the first cervical vertebra and articulates with the occiput of the head and the axis (C2). Has no vertebral body and no spinous process.
- Has lateral masses which are connected by an anterior and posterior arch. Each lateral mass contains a superior articular facet (for articulation with occipital condyles), and an inferior articular facet (for articulation with C2).
- The anterior arch contains a facet for articulation with the dens of the axis. This is secured by the transverse ligament of the atlas – which attaches to the lateral masses. The posterior arch has a groove for the vertebral artery and C1 spinal nerve.
Axis[edit | edit source]
The axis (C2) is easily identifiable due to its dens (odontoid process) which extends superiorly from the anterior portion of the vertebra.
The dens articulates with the anterior arch of the atlas, in doing so creating the medial atlanto-axial joint. This allows for rotation of the head independently of the torso.
C7: has a much larger and singular spinous process, known as the vertebra prominens, which is similar to those in the thoracic vertebrae.[4]
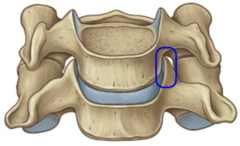
Intervertebral Disc (IVD)[edit | edit source]
IVD height grows more slowly than does vertebral body height (one third of the length of the spine is related to the disks at birth, one fifth of total spinal length after the age of 7 years). [6] The nucleus pulposus of cervical discs dries out by the age of 30 to a firm, fibrocartilaginous plate.[7]
- In the coronal plane, the superior surface of the disk is concave and the inferior surface is convex to conform to the adjacent vertebral bodies.
- Anteriorly, the disks are thicker than posteriorly to facilitate the lordotic curvature of the cervical spine.
- Movement in the coronal plane is limited by the uncinate process; however, the disks allow for some anteroposterior translation.
- Posterolateral disk herniations are fewer in frequency, likely secondary to the posterolateral location of the uncinate process.
The cartilaginous endplate is composed of hyaline cartilage and is located adjacent to the subchondral bone.
- serves as a barrier to nucleus pulposus pressure on the vertebral body to limit protrusion.
- serves as the growth plate and is responsible for endochondral ossification.
- permit diffusion of nutrients from the subchondral bone to the disk and serve as insertion points for the inner fibers of the annulus.
- The ALL and the posterior longitudinal ligament (PLL) are confluent with the outer fibers of the annulus[6]
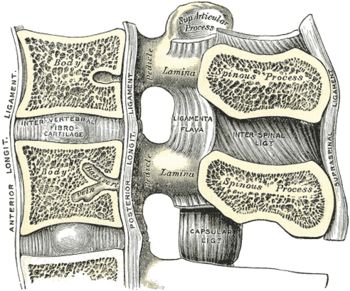
Joints[edit | edit source]
The joints of the cervical spine can be divided into two groups – those that are present throughout the vertebral column, and those unique to the cervical spine.[3]
Present throughout Vertebral Column
There are two different joints present throughout the vertebral column: The disc joint (determines how much vertebral motion is possible at a particular segmental level), and the facet joints (determine the type of motion)
- Disc Joint, between vertebral bodies – adjacent vertebral bodies are joined by intervertebral discs, made of fibrocartilage (cartilaginous joint, known as a symphysis). As a whole, the disc joint itself has three major functions:
- The disc joint bears the weight of the body above it. The increasing size of the vertebral bodies and the discs attached to them descending the spine helps the disc joints bear the increasing weight of the portion of the body above it.
- The disc joint’s thickness allows for a great deal of motion. Overall, the intervertebral discs comprise 25% of the height of the entire spine. In the cervical spine, they total 40% of its height. The greater the relative height of the discs compared to vertebral body height, the greater the possible motion at that region of the spine.
- The intervertebral discs help to absorb shock[8]
- Facet joint, formed by the articulation of superior and inferior articular processes from adjacent vertebrae (synovial joint). The scientific name for facet joints is zygapophyseal joints, hence they are also often known as Z joints. Facet joints function to guide motion at that segmental joint level of the spine. Facet joints determine the type of motion (i.e., the direction of motion) that can occur there. At the upper cervical spine, the plane of the facets is perfectly horizontal in the transverse plane. Descending the cervical spine, the orientation of the facets gradually transition to be more vertical in the frontal plane. As a general rule, the plane of the cervical facets is usually considered to be an oblique plane with an approximately 45-degree angle between the transverse and frontal planes (Fig. 7A). This angle is often compared to that of the slope of a roof. The type of motion best afforded at each vertebral segmental joint level is important to know and understand when performing joint mobilization[8]
Unique to Cervical Spine[edit | edit source]
Joints unique to the cervical spine: uncovertebral joints; the atlanto-axial (x3); atlanto-occipital joints (x2).
Uncovertebral joints are small synovial articulations, measuring 2 × 4 to 3 × 6 mm., situated between the five lower cervical vertebral bodies. They are located anteromedially to the mixed nerve root and posteromedially to the vertebral artery, vein, and sympathetics as these pass through the vertebral foramen. They participate with the disk and vertebral body in the formation of the anterior wall of the foramen. On the upper surfaces of their posterolateral aspects of the relevant vertebra convex spur-like ridges (consisting of spongy bone and covered by cartilage) are the uncinate process. On the corresponding undersurface of the vertebral body below are concave areas (also covered by cartilage). These two structures come into apposition and are covered by synovial membrane to form the Luschka joints.[9]
The atlanto-axial joints are formed by the articulation between the atlas and the axis:
- Lateral atlanto-axial joints (x2) – formed by the articulation between the inferior facets of the lateral masses of C1 and the superior facets of C2. These are plane type synovial joints.
- Medial atlanto-axial joint – formed by the articulation of the dens of C2 with the articular facet of C1. This is a pivot type synovial joint.
The atlanto-occipital joints consist of an articulation between the spine and the cranium. They occur between then superior facets of the lateral masses of the atlas and the occipital condyles at the base of the cranium. These are condyloid type synovial joints, and permit flexion at the head i.e. nodding.
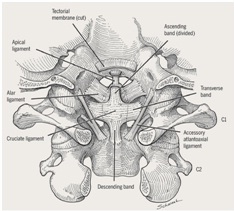
Ligaments[edit | edit source]
There are six major ligaments to consider in the cervical spine. The majority of these ligaments are present throughout the entire vertebral column.
Present throughout Vertebral Column
- Anterior and posterior longitudinal ligaments – long ligaments that run the length of the vertebral column, covering the vertebral bodies and intervertebral discs.
- Ligamentum flavum – connects the laminae of adjacent vertebrae.
- Interspinous ligament – connects the spinous processes of adjacent vertebrae.
Unique to Cervical Spine
- Nuchal ligament – a continuation of the supraspinous ligament. It attaches to the tips of the spinous processes from C1-C7, and provides the proximal attachment for the rhomboids and trapezius.
- Transverse ligament of the atlas – connects the lateral masses of the atlas, and in doing so anchors the dens in place.
(Note: Some texts consider the interspinous ligament to be part of the nuchal ligament).[3]
Muscles[edit | edit source]
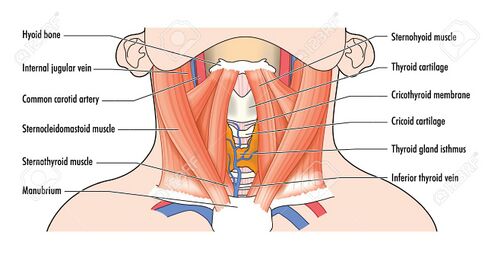
The cervical vertebrae serve as the origination and insertion points for a host of muscles that support but also enable movement of the head and neck. The musculature of the neck is comprised of a number of different muscle groups. They can be divided into anterior, lateral and posterior groups based on their position in the neck. They are further divided into more specific groups based on a number of determinants; including depth, precise location, and function. Sternocleidomastoid is a key landmark because it divides the neck into anterior region and vertebral regions.
Anterior Neck Muscles[edit | edit source]
Superficial muscles - platysma, sternocleidomastoid
Suprahyoids - Digastric, mylohyoid, geniohyoid, stylohyoid
Infrahyoids - sternohyoid, sternothyroid, thyrohyoid, omohyoid[10]
Vertebral Muscles[edit | edit source]
Muscles forming musculoskeletal columns around vertebra. These are further divided into anterior, lateral and posterior vertebral muscle groups.
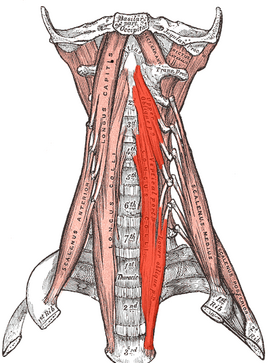
Anterior (Prevertebral) Vertebral Muscles[edit | edit source]
These are also termed Deep cervical flexor:
- Rectus Capitis Anterior
- Rectus Capitis Lateralis
- Longus capitis
- Longus colli/ Longus cervicis (3 portions: superior oblique, inferior oblique, vertical)
Lateral Vertebral Muscles (Paravertebral)[edit | edit source]
Scalenes - anterior, middle, posterior and minimus scalene muscles
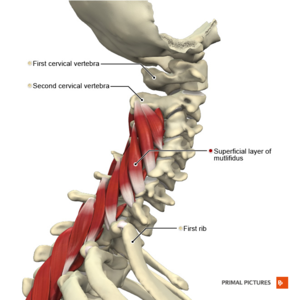
Posterior Vertebral Muscles[edit | edit source]
These can be further divided into intrinsic and extrinsic muscles.
Extrinsic muscles[edit | edit source]
Trapezius and Levator scapulae
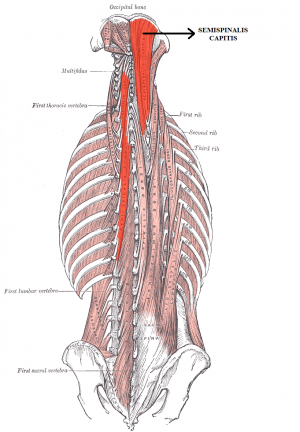
Intrinsic muscles[edit | edit source]
- Superficial muscles :
- Deep muscles:
- Suboccipital group -
- Transversospinalis muscles -
- semispinalis capitis,
- semispinalis cervicis,
- rotatores cervicis,
- multifidus (these are also known as deep neck extensors)
- Interspinales and intertransversarii.[11][10]
Movements and muscles in the cervical spine and head[edit | edit source]
| Movement | Muscles[12] |
|---|---|
| Flexion | Longus colli
Rectus capitis anterior (head only) |
| Extension | Levator Scapulae
Rectus capitis posterior, major and minor (head only) |
| Lateral flexion | Scalene anterior, medius and posterior
Sternocleidomastoid Splenius capitis Trapezius Erector spinae Rectus capitis lateralis (head only) |
| Rotation | Semispinalis cervicis
Multifidus Scalene anterior Splenius cervicis and capitis Sternocleidomastoid Inferior oblique (head only) Rectus captitis posterior major (head only) |
Nerves[edit | edit source]
The cervical spine functions as bony protection of the spinal cord as it exits the cranium.
Despite the presence of seven cervical vertebrae, there are eight pairs of cervical nerves, termed C1 to C8. C1 through C7 exit the spine cranially to its associated vertebrae, while C8 exits caudally to C7. [4]
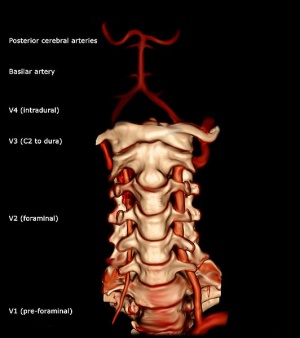
The transverse foramina of the cervical vertebrae provide a passageway by which the vertebral artery, vein and sympathetic nerves can pass. The only exception to this is C7 – where the vertebral artery passes around the vertebra, instead of through the transverse foramen.[3]The neural components sit posterior to the vertebral artery.[13]
Blood Supply[edit | edit source]
Distal to their bifurcation from the subclavian arteries, the vertebral arteries course cranially to the base of the skull. They progress past the C7 vertebrae anteriorly before entering the transverse foramen of C6. After exiting the C2 transverse foramen, the arteries bend laterally to enter the more widely placed transverse foramen of C1 and then revert medially over the superior aspect of the arch of the atlas before entering the base of the skull. Main tributaries of the vertebral arteries, the cervical radicular arteries, supply blood directly to the cervical vertebral bodies.
Also located in the cervical spine region are the carotid arteries. The common carotids bifurcate into the internal and external carotids at the C3 vertebral level. Despite their association with the neck, they do not perfuse any structures in the cervical spine.[4]
Concluding Points[edit | edit source]
- The ringlike structures of the atlas (C1) and axis (C2) are unique as compared with C3 to C7 vertebral bodies.
- The major stabilizing ligament of C1 and C2 is the transverse ligament.
- Understanding the various anatomic relationships of the spinal ligaments and muscles is essential.
- The vertebral artery usually enters the transverse foramen at C6.
- Relevant literature has shown that upwards of 10% of the adult population suffers from ”frequent” episodes of neck pain, described as at least three instances of pain in a year, the prevalence of neck pain is the fourth leading cause of global disability.[4]
- Subacute and chronic neck pain also share diverse etiology. Arthritis of cervical facet joints is a common cause of mechanical neck pain. Meanwhile, nerve root compression, intervertebral disk herniation, and spinal stenosis are the most frequent cause of peripheral neuropathic neck pain[4]
- Between the vertebral canal bone and the dura mater is the epidural space[6]
- The cervical spine’s major functions include supporting and cushioning loads to the head/neck while allowing for rotation, and protecting the spinal cord extending from the brain.
- Of these seven vertebrae, the atlas (C1) and the axis (C2) are among the most important for rotation and movement of the head
- The cervical spine protects both the efferent and afferent nerves that stem from the spinal cord if damaged potentially having dramatic effects on the nervous system, affecting the patient’s daily activity, and even causing a potential paralysis[14]
Resources[edit | edit source]
References[edit | edit source]
- ↑ Frost BA, Camarero-Espinosa S, Foster EJ. Materials for the spine: anatomy, problems, and solutions. Materials. 2019 Jan;12(2):253. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6356370/ (last accessed 28.1.2020)
- ↑ Petersen JA, Brauer C, Thygesen LC, Flachs EM, Lund CB, Thomsen JF. Prospective, population-based study of occupational movements and postures of the neck as risk factors for cervical disc herniation. BMJ open. 2022 Feb 1;12(2):e053999.
- ↑ 3.0 3.1 3.2 3.3 3.4 Teach me anatomy The cervical Spine Available from:https://teachmeanatomy.info/neck/bones/cervical-spine/ (last accessed 28.1.2020)
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Kaiser JT, Lugo-Pico JG. Anatomy, Head and Neck, Cervical Vertebrae. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539734/ (last accessed 28.1.2020)
- ↑ Kaiser JT, Reddy V, Lugo-Pico JG. Anatomy, head and neck, cervical vertebrae.2022.
- ↑ 6.0 6.1 6.2 Musculoskeletal Cervical spine Available from:https://musculoskeletalkey.com/cervical-spine-anatomy/ (last accessed 29.1.2020)
- ↑ Peng B, Bogduk N. Cervical discs as a source of neck pain. An analysis of the evidence. Pain Medicine. 2019 Mar 1;20(3):446-55.
- ↑ 8.0 8.1 Learn muscles . Cervical spine joints. Available from: https://learnmuscles.com/blog/2017/08/01/cervical-spinal-joints/ (last accessed 29.1.2020)
- ↑ RSNA Joints of Luschka Available from: https://pubs.rsna.org/doi/10.1148/66.2.181 (last accessed 28.1.2020)
- ↑ 10.0 10.1 Drake R, Vogl AW, Mitchell AW. Gray's anatomy for students E-book. Elsevier Health Sciences; 2009 Apr 4.
- ↑ Ken Hub Muscles of the neck Available from: https://www.kenhub.com/en/library/anatomy/muscles-of-the-neck-an-overview (last accessed 28.1.2020)
- ↑ Palastanga, N., & Soames, R. (2012). Anatomy and human movement (6th ed.). Edinburgh: Churchill Livingstone.
- ↑ Joshi N, Klinger N, Halalmeh DR, Tubbs RS, Moisi MD. The Neural Sulcus of the Cervical Vertebrae: A Review of Its Anatomy and Surgical Perspectives. Cureus. 2020 Jan 18;12(1).
- ↑ Frost BA, Camarero-Espinosa S, Foster EJ. Materials for the spine: anatomy, problems, and solutions. Materials. 2019 Jan;12(2):253.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6356370/ (last accessed 29.1.2020)