Cesarean Section: Difference between revisions
Kim Jackson (talk | contribs) (Formatting and replaced image) |
No edit summary |
||
| (41 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|Mereena Baby]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:User Name|Mereena Baby]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== | == Introduction == | ||
[[File: | [[File:Cesarian.jpeg|right|frameless|450x450px]] | ||
A cesarean section can be defined as the procedure in which the delivery of a baby is through an incision in the [[Abdominal Muscle Anatomy|abdominal]] wall and uterus rather than through the [[pelvis]] and [[Female Genital Tract|vagina]].<ref>Al-Ziraqi, I, et al: uterine rupture after previous caesarean section.BJOG 117(7):809-820,2010</ref><ref>Gilbert,E, and Harman, J;High risk pregnancy and delivery, ed.1.St Louis:CV Mosby,1986</ref><ref>Harrington,K, and Haskvitz, E:Managing a patient’s constipation with physical therapy.Phys Ther Nov 86:1511-1519;2006</ref><ref>Jamieson,D, and Steege, J:The prevalence of dysmenorrhea,dyspareunia, pelvic pain and irritable bowel syndrome in primary care practices.Obstet Gynecol 87(1):55-58,1996</ref><ref>Norwood,C:caesarean variations: Patients, facilities, or policies.Int J Childbirth Educ 1 :4,1986.</ref> General, spinal or epidural [[Surgery and General Anaesthetic|anesthesia]] is used.<ref name=":0">Carolyn Kisner, Lynn Allen Colby :Therapeutic Exercise Foundations and techniques 6 th edition:Pg 952</ref> | |||
The incision used during a cesarean section can be vertical (up-and-down) or transverse (side-to-side). However, the condition of the mother and the fetus determines which type of incision will be used. | |||
== | == Increasing Cesarean Demand == | ||
Births by caesarean section are rising, worldwide. The latest figures (2016) show that 25% of births in Western Europe were by caesarean delivery; in North America it was 32%, and in South America 41%.<ref>The Conversation Caesarean section versus natural birth – an obstetrician examines a new review Available from: https://theconversation.com/caesarean-section-versus-natural-birth-an-obstetrician-examines-a-new-review-90483 (accessed 3.4.2021)</ref> | |||
Caesarean sections can be lifesaving for both mother and baby, however an increasing number of them are not being performed for a medical reason<ref name=":25">The Conversation Babies born by caesarean develop slower in first year than those born naturally – new findings Available from:https://theconversation.com/babies-born-by-caesarean-develop-slower-in-first-year-than-those-born-naturally-new-findings-147639 (accessed 3.4.2021)</ref>. | |||
* | A growing body of evidence highlights the potential negative effects of non-essential planned caesareans. eg children born via planned caesarean section have a small, elevated risk of poor development and/or performance at school age. Other studies have found that babies born by planned caesarean have an increased risk of breathing problems after birth, and an increased risk of [[Childhood Obesity|childhood obesity]], [[asthma]] and [[diabetes]]. | ||
* Mothers requiring a caesarean for medical reasons shouldn’t worry as these are performed to protect their health, and the health of their child. It’s also important to remember that many factors affect development – including [[nutrition]], childhood experiences and [[Genetic Conditions and Inheritance|genetics]] – which are all key in helping babies keep up with others their age<ref name=":25" />. | |||
* Some women request C-sections with their first babies — to avoid labor or the possible complications of vaginal birth or to take advantage of the convenience of a planned delivery. However, this is discouraged if client plans on having several children. Women who have multiple C-sections are at increased risk of placental problems as well as heavy bleeding, which might require surgical removal of the uterus (hysterectomy).<ref name=":26">Mayo Clinic [https://www.mayoclinic.org/tests-procedures/c-section/about/pac-20393655 Cesarean section] Available from: https://www.mayoclinic.org/tests-procedures/c-section/about/pac-20393655<nowiki/>(accessed 3.4.2021)</ref> | |||
== | == Types of Cesareans == | ||
[[File:First Breath.jpeg|right|frameless|400x400px]] | |||
The two types of incisions that can be used for a caesarean section are: | |||
# Lower segment incision – will be used wherever possible. This is a horizontal cut through the abdomen and a horizontal cut through the lower part of the uterus, sometimes known as a ‘bikini line’ incision. These cuts heal better, are less visible and are less likely to cause problems in future pregnancies. | |||
# Classical incision – refers to a vertical cut on the uterus. The cut on the abdomen may be horizontal or vertical. This type of incision is usually only used for extreme emergencies or in specific situations, such as if the placenta is lying very low, if the baby is lying sideways or if the baby is very small. It can increase the chance of having problems in later pregnancies and births<ref name=":1">Vic Gov. [https://www.betterhealth.vic.gov.au/health/HealthyLiving/caesarean-section Ceserean Section] Available from: https://www.betterhealth.vic.gov.au/health/HealthyLiving/caesarean-section (accessed 3.4.2021)</ref>. | |||
Image: First breath of a child being born by cesarean section | |||
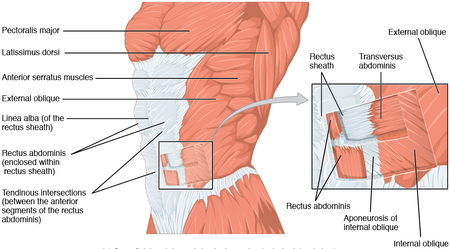
== | == Anatomy == | ||
[[File:1112 Muscles of the Abdomen Anterolateral.png|right|frameless|450x450px]] | |||
* | To achieve a cesarean delivery, the surgeon must traverse all the layers that separate him/her from the fetus. | ||
* First, the [[skin]] is incised, followed by the subcutaneous tissues. The next layer is the [[fascia]] overlying the [[Abdominal Muscles|rectus abdominis]] muscles. | |||
* After separating the rectus [[muscle]]<nowiki/>s the surgeon enters the abdominal cavity through the parietal peritoneum. | |||
* The uterus is next incised. It consists of the serosal outer layer (perimetrium), the muscle layer (myometrium), and the inside mucosal layer (endometrium). All three of these layers are incised to make the uterine incision. | |||
* Depending on the status of the patient’s amniotic membranes (if her “water is broken” or intact), the surgeon could encounter that amniotic sac upon incision of the uterus. The amniotic sac, if present, would be the last layer between the surgeon and the fetus. | |||
* It is at this point that the fetus is delivered, achieving the primary goal of the cesarean section<ref>Sung S, Mahdy H. [https://www.ncbi.nlm.nih.gov/books/NBK546707/ Cesarean Section]. StatPearls [Internet]. 2020 Aug 23.Available from: https://www.ncbi.nlm.nih.gov/books/NBK546707/<nowiki/>(accessed 3.4.2021)</ref> | |||
== Reasons for the Procedure == | |||
Some cesarean deliveries are planned and scheduled, while others are performed as a result of complication that occurs during [[labour]]. There are several conditions in which cesarean delivery is more likely to occur. These include: | |||
* Fetal distress, indicated by abnormal fetal heart rate | |||
* | * Abnormal position of the fetus breech presentation (breech or transverse positioning) | ||
* | * Labour that fails to progress | ||
* | * Size of a baby is too large to be delivered vaginally | ||
* | * Placental complications like placenta previa | ||
* | * Maternal medical conditions such as [[Gestational diabetes|diabetes]], [[Hypertension in Pregnancy|high blood pressure]], [[Human Immunodeficiency Virus (HIV)|HIV]] infection | ||
* | * Active [[Herpes Zoster|herpes]] infection in the mother’s vagina or cervix | ||
* | * Carrying multiples | ||
* Previous history of cesarean delivery.<ref>Pushpal K Mitra : Textbook of Physiotherapy in surgical conditions:Pg 235-238</ref><ref>Notzon FC, Cnattingius S, Bergsjø P, Cole S, Taffel S, Irgens L, Daltveit AK. Cesarean section delivery in the 1980's: International comparison by indication. American journal of obstetrics and gynecology. 1994 Feb 1;170(2):495-504.</ref> Initially, clinicians were concerned about the scar from the previous birth rupturing. However, growing evidence is supporting safe vaginal birth after caesarean (VBAC).<ref>Bangal VB, Giri PA, Shinde KK, Gavhane SP. Vaginal birth after cesarean section. North American journal of medical sciences. 2013 Feb;5(2):140.</ref><ref>Cahill A, Tuuli M, Odibo AO, Stamilio DM, Macones GA. Vaginal birth after caesarean for women with three or more prior caesareans: assessing safety and success. BJOG: An International Journal of Obstetrics & Gynaecology. 2010 Mar;117(4):422-8.</ref><ref>Flamm BL, Goings JR, Liu Y et al. Elective repeat caesarean section versus trial of labour: a prospective multicenter study. Obstetrics and Gynecology 1994; 83: 927-932.</ref><ref>McMahon MJ, Luther ER, Bowes WA et al. Comparison of trial of labour with an elective second caesarean section. New England Journal of Medicine 1996; 335: 689-695.</ref> | |||
== | == Risks == | ||
Risks to the baby include: | |||
* | * Breathing problems. Babies born by scheduled C-section are more likely to develop transient tachypnea (abnormally fast breathing during the first few days after birth). | ||
* Surgical injury. Although rare, accidental nicks to the baby's skin can occur during surgery. | |||
Risks to you include: | |||
* Infection: an infection of the lining of the uterus (endometritis). | |||
* Postpartum hemorrhage: A C-section might cause heavy bleeding during and after delivery. | |||
* Reactions to anesthesia: Adverse reactions to any type of anesthesia are possible. | |||
* Blood clots: A C-section might increase the risk of developing a [[Deep Vein Thrombosis|deep vein thrombosis]]. | |||
* Wound infection. | |||
* Surgical injury: Although rare, surgical injuries to the bladder or bowel can occur during a C-section. | |||
* Increased risks during future pregnancies: The more C-sections a person has, the higher the risks of placenta previa and placenta accreta (a condition in which the placenta becomes abnormally attached to the wall of the uterus).<ref name=":26" /> | |||
* | == Physiotherapy == | ||
[[File:Breastfeeding.jpeg|right|frameless]] | |||
Physical therapy can significantly improve a mothers ability to return to functional activities postpartum. | |||
* Pregnancy and cesarean section can have a significant impact on a mothers [[posture]] and muscle strength and may lead to urinary [[Urinary Incontinence]], [[Pelvic Girdle Dysfunction Interventions: Core Activation, Targeted Strengthening and Stretching|pelvic girdle]] or [[Low Back Pain and Pregnancy|back pain]], and/or [[Uterine Prolapse|pelvic organ prolapse.]] | |||
* Caring for a newborn typically requires static postures, lifting, carrying, and bending that require a significant amount of strength and stability throughout the pelvis, back, abdomen, neck, and shoulders. | |||
'''Educate Client''' on these common manoeuvers | |||
Getting into and out of bed: When turning over in bed, bend one knee at a time and support the belly with a hand or a small pillow, if necessary, while turning shoulders, hips, and knees all at the same time to avoid excessive twisting. When getting into bed, keep shoulders, hips and knees facing the same direction while lowering body down onto the side and bringing both feet up onto the bed together before rolling onto your back. Reverse this sequence when getting out of bed by rolling onto your side, lowering both legs off the side of the bed, and pushing up to a seated position with your arm. | |||
Sitting and feeding: Whether breastfeeding or bottle feeding, make sure person has adequate support for low back and uses a cushion or pillow to bring the baby close to avoid slouching or leaning. Remember client can also lie on side for feeding. | |||
Coughing and sneezing: It is important to keep your chest clear. You can do this by taking a deep breath 2-3 times per hour. Your tummy may be sore but try not to hold back a cough or sneeze. To make these more comfortable, you can lean forward, resting your hands on your legs or bring your knees to your chest if you are lying in bed. Support your belly with your hands or a small pillow. | |||
Posture: Try to stand tall and avoid slouching or leaning forward. When changing diapers, place your baby on a changing table that is high enough to avoid bending. | |||
'''Exercises''' | |||
* | * Low-intensity exercises can be commenced once the scar is healed properly. It usually takes 6 weeks for the scar to heal. Till then breathing exercises, calf stretch, ankle-toe movements, active exercises of the upper limb, and walking can be done. The total duration should be around 30 minutes per day as per ACOG guideines. | ||
see also | |||
* [[Physical Activity and Pregnancy]] | |||
* | * [[Pregnancy Related Pelvic Pain]] | ||
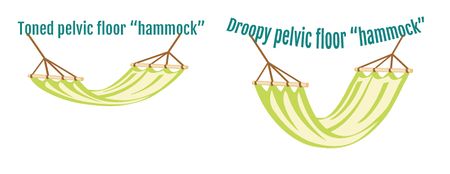
[[File:Pelvic-floor-muscles hammock.jpg|right|frameless|450x450px]] | |||
* | It is important to client does not expect too much too soon, the body needs time to heal. | ||
* Avoid any activities that cause straining: Do not lift anything heavier than the baby for the first few weeks. | |||
* Walking is a great way to stay active. | |||
* Performing gentle pelvic floor muscle contractions as soon as possible. Regular use of these muscles helps improve normal bowel and bladder control, improve and prevent prolapse, and restore sexual function. See [[Kegel's Exercise : Females|Pelvic Floor Exercises]] , [[Postnatal Period]] | |||
* Six weeks after a cesarean section is typically when it is safe to return to gentle exercise but this will vary by person, best to check with healthcare provider at your six-week postpartum follow-up visit. Once you have received the go-ahead, client can start to return to exercise making sure to start slow and build gradually. | |||
* [[Scar Management|Scar]] management: Once scar has healed completely, it can be beneficial to start doing some work to desensitize and stretch your scar<ref>Motion [https://motion.care/physical-therapy-after-c-section/ PT after a cesarean] Available from: https://motion.care/physical-therapy-after-c-section/ (accessed 3.4.2021)</ref>. | |||
'''Advice Mother to:''' | |||
* Eat a healthy, high-fibre diet and drink plenty of water. Do this every day to avoid constipation. | |||
* Use warmth on your wound. Warmth can have a soothing effect. Try a wheat bag or hot water bottle. | |||
* In accordance with your midwife’s or your doctor’s instructions, take [[Pain Medications|pain-relieving medication]] regularly to begin with to prevent pain. If you are breastfeeding, check that any medication you are using is safe for your baby too. | |||
* Keep your wound clean and dry. Look for signs of infection (such as redness, pain, swelling of the wound or bad-smelling discharge). Report these to your doctor or midwife. | |||
* While some women like loose clothing, many prefer firm, high-waisted compression underwear or control briefs to offer abdominal support. This can reduce pain and be worn for comfort for the first six weeks. | |||
* Avoid sex until you feel comfortable. It is quite normal to for it to take weeks, even months, before you are ready to have sex. | |||
* Numbness or itching around the scar is normal. This can last a long time for some women. | |||
* Join a new mothers’ group. Talking with other mums who have had a similar experience to you can be very helpful<ref name=":1" />. | |||
''' | |||
* | |||
* | |||
* | |||
* | |||
* | |||
* | |||
* | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category: | [[Category:Pelvic Health]] | ||
[[Category:Pelvis]] | |||
[[Category:Womens_Health]] | [[Category:Womens_Health]] | ||
[[Category:Pregnancy]] | [[Category:Pregnancy]] | ||
[[Category:Postpartum]] | [[Category:Postpartum]] | ||
[[Category:Interventions]] | |||
[[Category:Pelvis - Interventions]] | |||
Latest revision as of 11:37, 6 August 2022
Introduction[edit | edit source]
A cesarean section can be defined as the procedure in which the delivery of a baby is through an incision in the abdominal wall and uterus rather than through the pelvis and vagina.[1][2][3][4][5] General, spinal or epidural anesthesia is used.[6]
The incision used during a cesarean section can be vertical (up-and-down) or transverse (side-to-side). However, the condition of the mother and the fetus determines which type of incision will be used.
Increasing Cesarean Demand[edit | edit source]
Births by caesarean section are rising, worldwide. The latest figures (2016) show that 25% of births in Western Europe were by caesarean delivery; in North America it was 32%, and in South America 41%.[7]
Caesarean sections can be lifesaving for both mother and baby, however an increasing number of them are not being performed for a medical reason[8].
A growing body of evidence highlights the potential negative effects of non-essential planned caesareans. eg children born via planned caesarean section have a small, elevated risk of poor development and/or performance at school age. Other studies have found that babies born by planned caesarean have an increased risk of breathing problems after birth, and an increased risk of childhood obesity, asthma and diabetes.
- Mothers requiring a caesarean for medical reasons shouldn’t worry as these are performed to protect their health, and the health of their child. It’s also important to remember that many factors affect development – including nutrition, childhood experiences and genetics – which are all key in helping babies keep up with others their age[8].
- Some women request C-sections with their first babies — to avoid labor or the possible complications of vaginal birth or to take advantage of the convenience of a planned delivery. However, this is discouraged if client plans on having several children. Women who have multiple C-sections are at increased risk of placental problems as well as heavy bleeding, which might require surgical removal of the uterus (hysterectomy).[9]
Types of Cesareans[edit | edit source]
The two types of incisions that can be used for a caesarean section are:
- Lower segment incision – will be used wherever possible. This is a horizontal cut through the abdomen and a horizontal cut through the lower part of the uterus, sometimes known as a ‘bikini line’ incision. These cuts heal better, are less visible and are less likely to cause problems in future pregnancies.
- Classical incision – refers to a vertical cut on the uterus. The cut on the abdomen may be horizontal or vertical. This type of incision is usually only used for extreme emergencies or in specific situations, such as if the placenta is lying very low, if the baby is lying sideways or if the baby is very small. It can increase the chance of having problems in later pregnancies and births[10].
Image: First breath of a child being born by cesarean section
Anatomy[edit | edit source]
To achieve a cesarean delivery, the surgeon must traverse all the layers that separate him/her from the fetus.
- First, the skin is incised, followed by the subcutaneous tissues. The next layer is the fascia overlying the rectus abdominis muscles.
- After separating the rectus muscles the surgeon enters the abdominal cavity through the parietal peritoneum.
- The uterus is next incised. It consists of the serosal outer layer (perimetrium), the muscle layer (myometrium), and the inside mucosal layer (endometrium). All three of these layers are incised to make the uterine incision.
- Depending on the status of the patient’s amniotic membranes (if her “water is broken” or intact), the surgeon could encounter that amniotic sac upon incision of the uterus. The amniotic sac, if present, would be the last layer between the surgeon and the fetus.
- It is at this point that the fetus is delivered, achieving the primary goal of the cesarean section[11]
Reasons for the Procedure[edit | edit source]
Some cesarean deliveries are planned and scheduled, while others are performed as a result of complication that occurs during labour. There are several conditions in which cesarean delivery is more likely to occur. These include:
- Fetal distress, indicated by abnormal fetal heart rate
- Abnormal position of the fetus breech presentation (breech or transverse positioning)
- Labour that fails to progress
- Size of a baby is too large to be delivered vaginally
- Placental complications like placenta previa
- Maternal medical conditions such as diabetes, high blood pressure, HIV infection
- Active herpes infection in the mother’s vagina or cervix
- Carrying multiples
- Previous history of cesarean delivery.[12][13] Initially, clinicians were concerned about the scar from the previous birth rupturing. However, growing evidence is supporting safe vaginal birth after caesarean (VBAC).[14][15][16][17]
Risks[edit | edit source]
Risks to the baby include:
- Breathing problems. Babies born by scheduled C-section are more likely to develop transient tachypnea (abnormally fast breathing during the first few days after birth).
- Surgical injury. Although rare, accidental nicks to the baby's skin can occur during surgery.
Risks to you include:
- Infection: an infection of the lining of the uterus (endometritis).
- Postpartum hemorrhage: A C-section might cause heavy bleeding during and after delivery.
- Reactions to anesthesia: Adverse reactions to any type of anesthesia are possible.
- Blood clots: A C-section might increase the risk of developing a deep vein thrombosis.
- Wound infection.
- Surgical injury: Although rare, surgical injuries to the bladder or bowel can occur during a C-section.
- Increased risks during future pregnancies: The more C-sections a person has, the higher the risks of placenta previa and placenta accreta (a condition in which the placenta becomes abnormally attached to the wall of the uterus).[9]
Physiotherapy[edit | edit source]
Physical therapy can significantly improve a mothers ability to return to functional activities postpartum.
- Pregnancy and cesarean section can have a significant impact on a mothers posture and muscle strength and may lead to urinary Urinary Incontinence, pelvic girdle or back pain, and/or pelvic organ prolapse.
- Caring for a newborn typically requires static postures, lifting, carrying, and bending that require a significant amount of strength and stability throughout the pelvis, back, abdomen, neck, and shoulders.
Educate Client on these common manoeuvers
Getting into and out of bed: When turning over in bed, bend one knee at a time and support the belly with a hand or a small pillow, if necessary, while turning shoulders, hips, and knees all at the same time to avoid excessive twisting. When getting into bed, keep shoulders, hips and knees facing the same direction while lowering body down onto the side and bringing both feet up onto the bed together before rolling onto your back. Reverse this sequence when getting out of bed by rolling onto your side, lowering both legs off the side of the bed, and pushing up to a seated position with your arm.
Sitting and feeding: Whether breastfeeding or bottle feeding, make sure person has adequate support for low back and uses a cushion or pillow to bring the baby close to avoid slouching or leaning. Remember client can also lie on side for feeding.
Coughing and sneezing: It is important to keep your chest clear. You can do this by taking a deep breath 2-3 times per hour. Your tummy may be sore but try not to hold back a cough or sneeze. To make these more comfortable, you can lean forward, resting your hands on your legs or bring your knees to your chest if you are lying in bed. Support your belly with your hands or a small pillow.
Posture: Try to stand tall and avoid slouching or leaning forward. When changing diapers, place your baby on a changing table that is high enough to avoid bending.
Exercises
- Low-intensity exercises can be commenced once the scar is healed properly. It usually takes 6 weeks for the scar to heal. Till then breathing exercises, calf stretch, ankle-toe movements, active exercises of the upper limb, and walking can be done. The total duration should be around 30 minutes per day as per ACOG guideines.
see also
It is important to client does not expect too much too soon, the body needs time to heal.
- Avoid any activities that cause straining: Do not lift anything heavier than the baby for the first few weeks.
- Walking is a great way to stay active.
- Performing gentle pelvic floor muscle contractions as soon as possible. Regular use of these muscles helps improve normal bowel and bladder control, improve and prevent prolapse, and restore sexual function. See Pelvic Floor Exercises , Postnatal Period
- Six weeks after a cesarean section is typically when it is safe to return to gentle exercise but this will vary by person, best to check with healthcare provider at your six-week postpartum follow-up visit. Once you have received the go-ahead, client can start to return to exercise making sure to start slow and build gradually.
- Scar management: Once scar has healed completely, it can be beneficial to start doing some work to desensitize and stretch your scar[18].
Advice Mother to:
- Eat a healthy, high-fibre diet and drink plenty of water. Do this every day to avoid constipation.
- Use warmth on your wound. Warmth can have a soothing effect. Try a wheat bag or hot water bottle.
- In accordance with your midwife’s or your doctor’s instructions, take pain-relieving medication regularly to begin with to prevent pain. If you are breastfeeding, check that any medication you are using is safe for your baby too.
- Keep your wound clean and dry. Look for signs of infection (such as redness, pain, swelling of the wound or bad-smelling discharge). Report these to your doctor or midwife.
- While some women like loose clothing, many prefer firm, high-waisted compression underwear or control briefs to offer abdominal support. This can reduce pain and be worn for comfort for the first six weeks.
- Avoid sex until you feel comfortable. It is quite normal to for it to take weeks, even months, before you are ready to have sex.
- Numbness or itching around the scar is normal. This can last a long time for some women.
- Join a new mothers’ group. Talking with other mums who have had a similar experience to you can be very helpful[10].
References[edit | edit source]
- ↑ Al-Ziraqi, I, et al: uterine rupture after previous caesarean section.BJOG 117(7):809-820,2010
- ↑ Gilbert,E, and Harman, J;High risk pregnancy and delivery, ed.1.St Louis:CV Mosby,1986
- ↑ Harrington,K, and Haskvitz, E:Managing a patient’s constipation with physical therapy.Phys Ther Nov 86:1511-1519;2006
- ↑ Jamieson,D, and Steege, J:The prevalence of dysmenorrhea,dyspareunia, pelvic pain and irritable bowel syndrome in primary care practices.Obstet Gynecol 87(1):55-58,1996
- ↑ Norwood,C:caesarean variations: Patients, facilities, or policies.Int J Childbirth Educ 1 :4,1986.
- ↑ Carolyn Kisner, Lynn Allen Colby :Therapeutic Exercise Foundations and techniques 6 th edition:Pg 952
- ↑ The Conversation Caesarean section versus natural birth – an obstetrician examines a new review Available from: https://theconversation.com/caesarean-section-versus-natural-birth-an-obstetrician-examines-a-new-review-90483 (accessed 3.4.2021)
- ↑ 8.0 8.1 The Conversation Babies born by caesarean develop slower in first year than those born naturally – new findings Available from:https://theconversation.com/babies-born-by-caesarean-develop-slower-in-first-year-than-those-born-naturally-new-findings-147639 (accessed 3.4.2021)
- ↑ 9.0 9.1 Mayo Clinic Cesarean section Available from: https://www.mayoclinic.org/tests-procedures/c-section/about/pac-20393655(accessed 3.4.2021)
- ↑ 10.0 10.1 Vic Gov. Ceserean Section Available from: https://www.betterhealth.vic.gov.au/health/HealthyLiving/caesarean-section (accessed 3.4.2021)
- ↑ Sung S, Mahdy H. Cesarean Section. StatPearls [Internet]. 2020 Aug 23.Available from: https://www.ncbi.nlm.nih.gov/books/NBK546707/(accessed 3.4.2021)
- ↑ Pushpal K Mitra : Textbook of Physiotherapy in surgical conditions:Pg 235-238
- ↑ Notzon FC, Cnattingius S, Bergsjø P, Cole S, Taffel S, Irgens L, Daltveit AK. Cesarean section delivery in the 1980's: International comparison by indication. American journal of obstetrics and gynecology. 1994 Feb 1;170(2):495-504.
- ↑ Bangal VB, Giri PA, Shinde KK, Gavhane SP. Vaginal birth after cesarean section. North American journal of medical sciences. 2013 Feb;5(2):140.
- ↑ Cahill A, Tuuli M, Odibo AO, Stamilio DM, Macones GA. Vaginal birth after caesarean for women with three or more prior caesareans: assessing safety and success. BJOG: An International Journal of Obstetrics & Gynaecology. 2010 Mar;117(4):422-8.
- ↑ Flamm BL, Goings JR, Liu Y et al. Elective repeat caesarean section versus trial of labour: a prospective multicenter study. Obstetrics and Gynecology 1994; 83: 927-932.
- ↑ McMahon MJ, Luther ER, Bowes WA et al. Comparison of trial of labour with an elective second caesarean section. New England Journal of Medicine 1996; 335: 689-695.
- ↑ Motion PT after a cesarean Available from: https://motion.care/physical-therapy-after-c-section/ (accessed 3.4.2021)