Childhood Obesity: Difference between revisions
(Added text content to 'managing childhood obesity as a parent' but have not included the digrams/ images) |
Lynne Turner (talk | contribs) (added in check point with reflective element) |
||
| Line 94: | Line 94: | ||
* ''Negative attitudes.'' from parents, staff and peers can hinder your child’s interest in physical activity [REF] | * ''Negative attitudes.'' from parents, staff and peers can hinder your child’s interest in physical activity [REF] | ||
* ''Embarrassment.'' vulnerability, disappointment and shame at appearing physically incapable are just some of the emotions your child may experience | * ''Embarrassment.'' vulnerability, disappointment and shame at appearing physically incapable are just some of the emotions your child may experience | ||
[[File:Checkpoint.png|left|thumb]] | |||
Check Point: | |||
* Have a think, what are the main barriers that come to mind for you | |||
* Write down the main barrier | |||
* Now read the next section | |||
==== '''Facilitators: are what can make it easier''' ==== | ==== '''Facilitators: are what can make it easier''' ==== | ||
| Line 112: | Line 118: | ||
* the use of consistent encouragement by providers needs to be a key component of successful weight management. | * the use of consistent encouragement by providers needs to be a key component of successful weight management. | ||
* use of technology (eg, via text-messaging or email) for providing ongoing encouragement related to weight management between visits | * use of technology (eg, via text-messaging or email) for providing ongoing encouragement related to weight management between visits | ||
[[File:Checkpoint.png|left|thumb]] | |||
Check Point: | |||
* Look at the barrier you wrote down | |||
* Can you now think of a facilitator that could make it easier to overcome | |||
* Repeat this exercise for all of the barriers you thought of | |||
==== '''Stages of Change Model''' ==== | ==== '''Stages of Change Model''' ==== | ||
Revision as of 21:26, 27 March 2018
Original Editors - Alexander Dow, Andrea Civitarese, Lynne Turner, Alison O’Brien, Rachael Le Page, Courtney Ferguson
Top Contributors - Andrea Civitarese, Rachael Le Page, Lynne Turner, Kim Jackson, Lucinda hampton, Courtney Ferguson, Alison O' Brien, Alexander Dow and Rachael Lowe
Who is this page for?[edit | edit source]
The goal this page is to provide guidance and information to parents of overweight and obese children. We hope to give you some tools and resources in order to help you feel confident in managing your child's weight and activity levels.
By using this page, we hope you will be able to...[edit | edit source]
Obesity Overview[edit | edit source]
What is Childhood Obesity?[edit | edit source]
For adults, body mass index (BMI) is the method that is most commonly used to diagnose obesity. This method uses an individual's height and weight to establish whether or not they fall within a healthy weight range. BMI ranges are listed below:
- Healthy weight: BMI = 18.5-24.9
- Overweight: BMI = 25-29.9
- Obese: BMI = 30-39.9
- Severely Obese: BMI = ≥40
Calculate your child's BMI using the NHS Healthy Weight Calculator.
In children, BMI alone is not used to diagnose obesity, as children's bodies are constantly changing. To diagnose childhood obesity, paediatricians need to take many factors into consideration. Along with BMI, the paediatrician will take into consideration how your child is growing and developing, your family's history of obesity and related health problems (such as diabetes and heart disease), and your child's eating habits, activity levels, and general health.
Why does this matter?[edit | edit source]
What Are The Benefits Of Physical Activity For My Child?[edit | edit source]
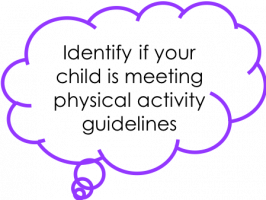
Physical activity and inactivity can have a big effect on your child's health and development in many way.
Regular activity[edit | edit source]
Having your child participate in regular physical activity benefit their body and mind health in a variety of ways.
Body
- Burns fat and maintains a healthy body weight
- Reduces their risk of developing chronic and major illnesses (see inactivity below)
- Builds and strengthens bones and muscles
- Improves fitness and establishes a healthy lifestyle
- Enhances balance, coordination and posture
- Builds core skills eg walking, running and throwing
Mind
- Builds confidence, self-esteem and mood
- Reduces stress, anxiety and depression
- Improves sleep
- Builds friendships and social skills
- Improves concentration, learning and academic performance
EMBED https://www.youtube.com/watch?v=nD-0Wc6eSUE
Inactivity[edit | edit source]
You may find that your child enjoys playing video games and watching tv, however this leads to an inactive lifestyle which can have a bad effect on your child’s future health. These effects may not show until later life but it is important to be aware of the higher risk of developing the following major diseases due to childhood inactivity (HW Kohl III, 2013):
- Obesity
- Heart disease eg coronary heart disease
- Stroke
- Diabetes
- Cancer
- Mental health disease eg anxiety, depression and dementia
- Earlier death
Physical Activity Guidelines for Children (Age 5-12)[edit | edit source]
Barriers and Facilitators to Managing Childhood Obesity[edit | edit source]
One of the key roles of health visitors and health professionals is to effectively present parents with the most up to date evidence on childhood obesity and interventions. Factors such as race, ethnicity, lifestyle, genetics, culture, socio-economic status, and the environment tend to have great influence on dietary choices (El-Sayed et al, 2011). Dealing with obesity is a complicated process, which involves a broad sociological awareness and understanding. It also requires tactful and compassionate communication skills that can influence behaviour and bring about positive lifestyle changes by breaking down barriers and identifying facilitators.
Barriers: are things that get in the way[edit | edit source]
Resources Barriers
- Financial resources. financial barriers can be a massive barrier to physical fitness especially for large families.
- Limited time. work hours for parents can be a barrier to family exercise, especially if having to work during evenings or on weekends,
- Access to programs. access to exercise programs can often be limited in areas or for certain age groups,
- Knowledge gaps. incomplete knowledge surrounding healthy eating (Keenan and Stapleton 2010 and Redsell et al 2010),
Social Barriers
- Cultural practices and expectations. cultural differences can contribute to difficulty in maintaining a healthy diet.
- Interpersonal dynamics. challenging family dynamics such as shared custody can make maintain a healthy eating and exercise routine can be very challenging.
Emotional Barriers
- Lack of confidence. uncertainty over their ability to control their child’s weight,
- Defeat. feelings of defeat related to previous failed attempts at weight management
- Loneliness. adolescents in particular often described feelings of isolation and loneliness related to their overweight status
- Denial. despite their involvement with the medical system, According to Keenan and Stapleton (2010) and Redsell et al (2010),most parents are unwilling to accept that their child has a weight issue.
- Negative attitudes. from parents, staff and peers can hinder your child’s interest in physical activity [REF]
- Embarrassment. vulnerability, disappointment and shame at appearing physically incapable are just some of the emotions your child may experience
Check Point:
- Have a think, what are the main barriers that come to mind for you
- Write down the main barrier
- Now read the next section
Facilitators: are what can make it easier[edit | edit source]
Building Partnerships
- the importance of building strong partnerships between patients, families, schools and health care providers is essential
- specifically discussed goal setting in collaboration with providers as a helpful element for weight management.
- engaged as an entire unit, so that parents and children could better partner to achieve goals around healthy living.
- GP or practice nurse can refer you to a local weight management programme for children, such as MEND and More Life.
Access to Resources
- primary care centre directly providing programs, including fitness classes, nutrition courses, and cooking classes
- showing parents and children how to create a healthy snack that not only looks good but tastes good.
- access to support groups could be a helpful resource and nutrition education classes
- access to free local community programmes and after school clubs
- clearer signposting to available resources
Consistent Encouragement
- the use of consistent encouragement by providers needs to be a key component of successful weight management.
- use of technology (eg, via text-messaging or email) for providing ongoing encouragement related to weight management between visits
Check Point:
- Look at the barrier you wrote down
- Can you now think of a facilitator that could make it easier to overcome
- Repeat this exercise for all of the barriers you thought of
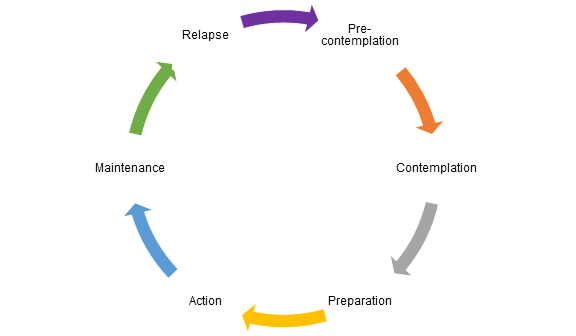
Stages of Change Model [edit | edit source]
Before change can be implemented it is completely normal to go though stages to making these changes a reality, this is referred to as the Stages of Change.
The stages of change are:
- Pre-contemplation (Not yet acknowledging that there is a problem behaviour that needs to be changed)
- Contemplation (Acknowledging that there is a problem but not yet ready or sure of wanting to make a change)
- Preparation/Determination (Getting ready to change)
- Action/Willpower (Changing behaviour)
- Maintenance (Maintaining the behaviour change) and
- Relapse (Returning to older behaviours and abandoning the new changes)
Managing Childhood Obesity as a Parent[edit | edit source]
Identify the causes:
- Busy lifestyle of the family equals less time to cook proper meals at home and increases eating out.
- Bigger portion sizes.
- Consuming large amounts of sugar.
- Ease of access to junk food and sugary drinks.
- School cutting back on P.E. programmes.
- Reduced physical activity and increased time in front of TV or computers.
WHAT TO DO?
- Get the whole family involved.
- Changing the family lifestyle to a more healthy one helps reduce childhood obesity as well as benefitting everyone else!
2. Lead by example.
- Exercise in some way every day. Do something you enjoy, whether it be a short walk or going for a swim.
- Avoid the TV or computer as much as possible. Your kids as less likely to turn on the TV if they are switched off and you are doing something they could be involved with.
- Prepare healthy meals in front of your child. Try to get them involved in preparation with an appropriate job. Tell them what it is and why it is good for you.
- Tell them about the good food you are eating, while eating it. Ask them if they fancy a bite?
3. Communicate well.
Addressing your child’s weight can be a sensitive subject, especially for teenagers. The earlier you start addressing the issue the better. Although it is never too late to try!
TIPS:
- Maintain an open dialogue: Encourage sharing of thoughts and feeling of your child about their body image. Do not force this, just encourage at appropriate times. Share your own feelings about your body.
- Listen well: Show that you are interested in how they feel and show them that you love them, no matter how they look.
- Avoid negative comments: Negativity can affect your child’s body image, relationship with food, and confidence. Stay positive in the way you talk about your own body as well as anyone else’s.
- Avoid blaming: This can result in a breakdown in the parent-child relationship which may result in a loss of trust, and stop your child listening to any advice you give. Therefore screaming, threatening, or punishing you child about their activity levels, weight or food is a big no no!
- Focus on health rather than weight: People can lose sight of what is important. As long as your child is healthy then weight is not so important. Children grow quickly, and may grow taller and ‘into their weight’.
HEALTHIER FOOD CHOICES
Be aware parents that if you are planning on changing your child’s diet, to consult your GP or dietician.
Parents can make simple healthy choices for their children such as;
- Start with small servings and let your child ask for more.
- Avoid adult sized plates
- try and make some healthy school lunches
- Here is a useful link for fun ideas - https://www.bbcgoodfood.com/howto/guide/school-packed-lunch-inspiration
This diagram shows you how much your child should be eating from each food group
- Linked is an online calorie counter will help you count your child’s calories. It is also available as an app; https://www.myfitnesspal.com/ PHYSICAL ACTIVITY It is always great to encourage your children to participate in 60 minutes of exercise every day. Children tend to imitate adults, if you exercise regularly you could encourage your children to join you. The benefits and guidelines of this topic are discussed in the above sections. REDUCE SCREEN TIME It is ok for your children to have some sedentary time, for example when they are doing homework etc. However, it is good to try and limit television, video games or the computer to no more than 2 hours a day. Instead you could find fun activities to do with your children that involves more physical activity.
Local Opportunities for Physical Activity in Edinburgh[edit | edit source]
Apps[edit | edit source]
These are some free apps that are available which give ideas for activities and encourage physical activity for children. This is not an exhausted list and there are many more apps available.
HOOP
App to find and book fun things to do in your local area for children aged 0-11 years old. (Available on iTunes and Android)
Kiddy Keep Fit by Scotty & Lulu
Fun app using music and games to get children moving and exercising. (Available on iTunes)
7-minute workout for kids
High intensity workouts with rests for 7 minutes to develop strength, stability and balance. (Available on iTunes)
Habitz
App set up by health professionals to assist parents to inspire their children to develop healthy habits and lifestyles. (Available on iTunes)
Sworkit Kids – Fitness Meets Fun (7-14 year olds)
Fun app providing a wide variety and duration of exercises to develop and enhance strength, agility and flexibility. (Available on iTunes and Android)
Appu’s Yoga for Kids
Easy yoga poses for children which enhances and refreshes their body and mind. (Available on iTunes and Android)
Wuf Shanti Yoga Fun Machine
Yoga app which uses games and music to promote health and happiness in children through yoga, meditation and mindfulness. (Available on iTunes)
When to ask for help... And who to ask[edit | edit source]
Conclusion[edit | edit source]
Useful Links[edit | edit source]
References[edit | edit source]
see adding references tutorial.
- ↑ Childhood Obesity in the UK Available from: https://www.youtube.com/watch?v=5Km1fFLX6T8 [last accessed 15/03/18]