De Quervain's Tenosynovitis
Original Editor - Elizabeth Dallas, Boris Alexandra
Top Contributors - Wanda van Niekerk, John Winkelhaus, David Cameron, John Fite, Robin Leigh Tacchetti, Robin Tacchetti, Laura Ritchie, Admin, Boris Alexandra, Kim Jackson, Aurelie Canas Perez, Julie Schuermans, Elizabeth Dallas, Lucinda hampton, Redisha Jakibanjar, Corin Arundale, Rachael Lowe, Tarina van der Stockt, Jess Bell, Jorge Rodríguez Palomino, WikiSysop, Naomi O'Reilly, Arturo Quiroz Marnef, 127.0.0.1, Kai A. Sigel, Claire Knott, Anas Mohamed, Chrysolite Jyothi Kommu and Evan Thomas
Clinically Relevant Anatomy
[edit | edit source]
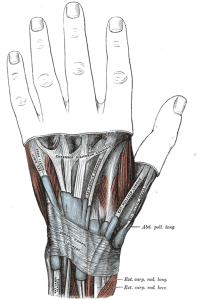
De Quervain's tenosynovitis involves the abductor pollicis longus and the extensor pollicis brevis tendons.
M. extensor pollicis brevis (EPB)
- origin: ½ dorsal side of the radius, the membrana interossea
- insertion: base of the proximal phalanx of the thumb
- function: - wrist joint: radial abduction
- thumb: extension - innervations: N. radialis
- artery: A. interossea posterior
M. abductor pollicis longus (APL)
- origin: dorsal side of the radius and the ulna, the membrana interossea
- insertion: base of ossis metacarpi I
- function: - wrist joint: radial abduction
- thumb: abduction - innervations: N. radialis
- artery: A. interossea posterior
The extensor retinaculum is a strong, fibrous structure that holds all the wrist extensors into place. It is located on the dorsal side of the wrist.
Definition/Description[edit | edit source]
De Quervain 's tenosynovitis is a painful wrist condition situated in the first dorsal compartment of the wrist.[1][2] It's a painfil inflammation of the tendons of extensor pollicis brevis (EPB) and the abductor pollicis longus (APL). These muscles are located on the dorsal side of the forearm and go to the lateral side of the thumb through a fibrous-osseous tunnel made of the processus styloideus radii and the extensor retinaculum. [3] [4] The pain, which is the main complaint, gets worse with abduction of the thumb, grasping action of the hand and an ulnar deviation of the wrist. Thickening and swelling can also be present. [5]
Epidemiology /Etiology[edit | edit source]
De Quervain's (Say "duh-Kair-VAZ") syndrome or de Quervain's disease named after the Swiss surgeon Fritz de ‘Quervain, who identified it first in 1895.[5] It’s an inflammation of the sheath or tunnel that surrounds two tendons that control the movement of the thumb. [2]
It’s caused by repetitive use of the thumb in combination with radial deviation of the wrist. (pinching, wringing, lifting, grasping, gardening, knitting). In this position the tendons of the EPB and the APL are pressed to the processus styloideus and when the movement is repeated frequently it can cause irritation of the tendons by friction. The tendons swell, the tunnel becomes too small. [4] [6]
Common activities were we need to use our wrist and thumb can cause a problem. [2]
It is often diagnosed in patients between 30-50 years. De Quervain syndrome is 10 times more frequent in women than men.[7] It’s common in sports like golf, bowling, tennis, mountain bike and it includes mothers of young children, computer keyboards operators, engine drivers.
In the technology age is has been nicknamed “Blackberry Thumb”[8]
Clinical Presentation[edit | edit source]
DeQuervains occurs in women 8-10 times more often than men. [9]The condition can be sudden or gradual. Presents most commonly with pain, swelling and tenderness on the radial side of the wrist at the base of the thumb (first dorsal compartment) as well in rest as in radial deviating of the wrist. Abduction of the thumb is also painful. The pain can radiate into the forearm and distally into the thumb. [3] [4] Symptoms increase with pinching, grasping, and gripping activities. New mothers are prone to this due to child care tasks with lifting, holding and feeding placing the hand in awkward positions; as well as hormonal changes. [10]
Differential Diagnosis
[edit | edit source]
1. Osteoarthritis of the first CMC joint[8][11]
2. Intersection syndrome – pain will be more towards the middle of the back of the forearm and about 2-3 inches below the wrist[8][11]
3. Wartenberg’s Syndrome - isolated neuritis of the superficial radial nerve, can be caused by tight jewelry[8][11]
4. Radiographs of the wrist and hand should be carefully scrutinized for scaphoid or scapholunate ligament.[12]
Diagnostic Procedures[edit | edit source]
Symptoms [13]
- Pain, tenderness and swelling at the base of the thumb.
- Pain can also radiate proximally into the forearm and distally into the thumb.
- Difficulty of movement of the thumb and wrist with activities such as grasping, pinching and crepitus (creaking sound).[13]
It’s a pain provocation test.[6]
Examination[edit | edit source]
The patient has to make an thumb adduction or an clenched fist in combination with an ulnar deviation. The patient feels pain on the radial side of the wrist around the processus styloideus and by doing this movement it reveals tenderness and swelling on the radial side of the wrist (radial styloid). The patient feels pain on active or passive movement of the thumb.
The diagnosis can be confirmed by performing Finkelstein’s test.
For this test the patient tucks the thumb into the palm of the hand and a quick turn of the wrist into full ulnar deviation follows is given. Another alternative approach that produces fewer false-positives involves gripping the patient’s thumb rather than tucking the thumb into the palm. A sharp pain occurs in the tendon sheath, as the test is positive. Advice to also examine the other common sites of tendon involvement: the flexor tendons of the fingers and the Achilles tendon.
[14]
Finkelstein’s test can give however a false positive result. [15]
On examination, resisted extension and abduction of the thumb is painful. Passive movements of wrist and thumb causes pain as the tendon slides up and down within its irritated sheath, and causes painful friction. Very occasionally, resisted radial deviation of the wrist also hurts because the thumb tendons assist this movement. Finkelstein’s test (deviating the wrist to the ulnar side, while the patients makes a fist with the thumb inside the fingers) reproduces these symptoms.
Medical Management (current best evidence)[edit | edit source]
| [16] |
Surgery is indicated if conservative therapy doesn’t help to improve the symptoms and complains of the patient. It’s also indicated when the patient relapses. [6] The sheath of the first dorsal compartment is opened longitudinally for decompression.
Experts agreed that patients with de Quervain’s disease should receive instructions in combination with other treatments: NSAIDs plus splinting, corticosteroid injection or surgery. [17]
When surgical treatment is recommended (for patients not responding to conservative treatment), a longitudinal incision is better than a transverse one as there are less complications of surgical treatment with a longitudinal incision. Patients with longitudinal scars had five hypertrophic scars, including some painful ones (less painful than transverse incisions). The hypertrophic scars are treated with corticosteroid injections, with no injuries to the nerve or vein. [18]
Ultrasound improves the treatment outcome and can be used as a diagnostic tool in management of de Quervain’s disease.[19] Success with ultrasound-guided injections was better than it was reported in literature and without adverse reactions .[14] Ultrasound-guided injections targeting the M. Extensor Pollicis Brevis with septation is more effective than manual injection. [20]
Endoscopic release for de Quervain’s tenosynovitis provides early improvement after surgery; there are fewer superficial radial nerve complications and greater scarf satisfaction, compared with open release surgery.[21] Endoscopic release of the first extensor compartment is reported as an effective and safe procedure for patients who are not responsive to non-operative treatments over an open release surgery. [21]
Another effective treatment of conservative management is steroid injection, but more research is needed to establish the full benefits of the treatment. [22]
Short-term clinical results showed that one-quarter partial resection of the extensor retinaculum on the dorsal side of the wrist, is a safe operative treatment and there aren’t any serious complications. [23]
Surgical treatment:[edit | edit source]
They make a short incision only through the skin creases over the first extensor compartment. Then they spread the longitudinal blades of the skin parallel to the radial nerve branches. (Injury to these radial nerve branches is the most common complication of this operation and is associated not only with troublesome neuromas, but even more with notoriously troublesome dysethesia in the nerve’s distribution to the dorsum of the hand.) The radial nerve branches are retracted; the first extensor compartment is opened along the dorsal border of the APL. They decompress the APL and search for the EPB. This step is important, as failure to decompress the EPB will be reflected in failure to gain full pain relief. Postoperatively, the wrist is splinted in a neutral position until the skin sutures are removed. This will minimize the probability of tendon anterior subluxation. The prognosis for permanent recovery is excellent.
Systemic anti-inflammatory medications with or without splinting are ineffective in treating de Quervain’s tenosynovitis. The direct injection of a small dose of cortisone into each of the two tendons is highly effective, about 60 to 70% for the first incidence unless dealing with an “-its” type. Accurate positioning of the needle into each tendon should be confirmed by observing the needle movements as flexing the first MC joint passively moves the APL. After the APL has been injected, the needle is placed for injection into small EPB sheath, with confirmation done by passively flexing the thumb’s MP joint.
Technique for steroid injection of tendon illustrated in treating de Quervain’s tenosynovitis. First good anaesthesia is obtained by intradermal injection of the skin allowing unhurried precise placement of the needle for the tendon steroid injections. A fine needle without an attached syringe is placed and repositioned as necessary until its position in the tendon sheath is confirmed with passive movement of the first MC joint for the APL and the thumb’s MP joint for the EPB. The syringe is attached after needle placement for the steroid injection. [12]
Physical Therapy Management (current best evidence)[edit | edit source]
The goals are to decrease the pain and the inflammation
Conservative therapy consists of: [4] [6]
- Rest by activity modification and the use of a thumb and wrist splint for 6 weeks
- Ice or cold packs
- Use of Non-Steroidal Anti-Inflammatory Drugs (NSAID’s): oral medication, phonophoresis or iontophoresis
- corticosteroid injections
Exercise is not practised because it can increase the pain and irritation of the tendons. There is not enough information about the benefit of exercise on De Quervain's syndrome.[24][6]
Key Research[edit | edit source]
- KANEKO, S., TAKASAKI, H., MAY, S., ‘Application of Mechanical Diagnosis and Therapy to a Patient Diagnosed with de Quervain’s Disease: A Case Study’, Journal of hand therapy, 2009.
- KNOBLOCH, K., GOHRITZ, A., SPIES, M., VOGT, M.P., ‘Neovascularisation in de Quervain’s disease of the wrist: novel combined therapy using sclerosing therapy with polidocanol and eccentric training of the forearms and wrists—a pilot report’, Springer, 2008.
- FOURNIER, K., BOURBONNAIS, D., BRAVO, G., ARSENAULT, J., HARRIS, P., GRAVEL, D., ‘Reliability and Validity of Pinch and Thumb Strength Measurements in de Quervain’s Disease’, Journal of hand therapy, 2006.
- ANDERSON, M., TICHENOR, C.J., ‘A Patient With De Quervain's Tenosynovitis: A Case Report Using an Australian Approach to Manual Therapy’, Physical therapy, 1994, nr 4, vol 74, p. 314 – 326.
Resources
[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1n1suG1n0N6R_6QRmGUFXGKlKAJMf_RVjy77Etvcmbew50JspU|charset=UTF-8|short|max=10: Error parsing XML for RSS
References
[edit | edit source]
- ↑ Muhammad Omer Ashraf • V. G. Devadoss Systematic review and meta-analysis on steroid injection therapy for de Quervain’s tenosynovitis in adult. Eur J Orthop Surg Traumatol (2014) (Level of Evidence 1A )
- ↑ 2.0 2.1 2.2 Hassan MK, Rahman MH. Role of Ultrasound In The Management of De'Quervain's Disease. Medicine today 2012 (Level of Evidence 1B)
- ↑ SCHUNKE, M., SCHULTE, E., SCHUMACHER, U., VOLL, M., WESKER, K., Prometheus, Bohn Stafleu van Loghum, Houten, 2005.
- ↑ 4.0 4.1 4.2 MEEUSEN, R., Praktijkgids pols- en handletsels, Kluwer editorial, Diegem, 1999.
- ↑ 5.0 5.1 Thomas Pagonis, Konstantinos Ditsios. Improved Corticosteroid Treatment of Recalcitrant de Quervain Tenosynovitis With a Novel 4-Point Injection Technique. Am J Sports Med 2011 (Level of evidence 2B)
- ↑ 6.0 6.1 6.2 6.3 6.4 VAN DONGEN, L.M., PILON, J.H.J., Handboek voor handrevalidatie theorie en praktijk, Bohn Stafleu van Loghum, Houten/Mechelen, 2002.
- ↑ Louis Patry, Michel Rossignol; Guide to the diagnosis of work- related musculoskeletal Disorders; Edition Multimonde, 1998, pag 1
- ↑ 8.0 8.1 8.2 8.3 Wikipedia. De Quervain syndrome. www.en.wikipedia.org/wiki/DeQuervain's_syndrome (accessed 13 Dec 2009)
- ↑ What is de Quervain's Disease? www.webmd.com/rheumatoid-arthritis/de-quervains-disease (accessed 15 Dec 2009)
- ↑ assh.org/Public/HandConditions/Pages/deQuervain'sTendonitis.aspx (accessed 13 Dec 2009)
- ↑ 11.0 11.1 11.2 DeQuervain's Disease - Wheeless' Textbook of Orthopaedics www.wheelssonline.com/ortho/dequervains_disease (accessed 13 Dec 2009)
- ↑ 12.0 12.1 Robert W. Wysocki, MD, Injection Therapy in the Management of Musculoskeletal Injuries: Hand and Wrist. Oper Tech Sports Med Elsevier 2012 (Level of Evidence 1A) Cite error: Invalid
<ref>tag; name "robert" defined multiple times with different content - ↑ 13.0 13.1 Anderson M; Tichenor CJ. A Patient with de Quervain's Tenosynovitis: A Case Report Using an Australian Approach to Manual Therapy. Physical Therapy. 1994;74(4):314-326
- ↑ 14.0 14.1 James D. McDermott, Ultrasound-guided injections for de Querain’s tenosynovitis, Clin. Othop. Relat. Res., 2012, vol. 7, p. 1925-1931,( level of evidence: 4.)
- ↑ Muhammad Omer Ashraf • V. G. Devadoss Systematic review and meta-analysis on steroid injection therapy for de Quervain’s tenosynovitis in adult. Eur J Orthop Surg Traumatol (2014) (Level of Evidence 1A )
- ↑ uwhand. Dequervain's Tenosynovitis. Available from: http://www.youtube.com/watch?v=roGXYRnUJZQ [last accessed 28/03/13]
- ↑ Huisstede B.M., Consensus on a multidisciplinary treatment guideline for de Quervain disease: results from the European handguide study, Physical therapy, 2014, (level of evidence: 1A)
- ↑ Syyed Jalil Abrisham, De Quervain tenosynovitis: clinical outcomes of surgical treatment with longitudinal and transverse incision, Oman. Med. Journal, 2011, vol. 2, p 91-93, (level of evidence: 1B)
- ↑ Hajder E., The role of ultrasound-guided triamcinolone injection in the treatment of de Quervain’s disease: treatment and diagnostic tool?, Chirurgie de la main, 2013, vol.6, p. 403-7,( level of evidence: 2B).
- ↑ Kume K., In de Quervain’s with a separate EPB compartment, ultrasound-guided steroid injection is more effective than a clinical injection technique: a prospective open-label study, Journal of hand surgery European volume, 2012, vol. 6, p.523-7,( level of evindence: 1B).
- ↑ 21.0 21.1 Kang H.J., Endoscopic versus open release in patients with de Quervain’s tenosynovitis: a randomized trial, The bone and joint journal, 2013, vol. 7, p. 947-51,( level of evidence: 1A). Cite error: Invalid
<ref>tag; name "kang" defined multiple times with different content - ↑ Ashraf M.O., Systematic review and meta-analysis on steroid injection therapy for de Quervain’s tenosynovitis in adults, European journal of orthopaedic surgery and traumatology: orthopédie traumatology, 2014, vol. 2, p. 149-57,( level of evidence: 1A)
- ↑ Altay M.A., De Quervain’s disease treatment using partial resection of the extensor retinaculum: a short-term results survey, Orthopaedics and traumatology, surgery and research: OTSR, 2011, vol. 5, p. 489-93,( level of evidence: 4)
- ↑ BACKSTROM, K.M., ‘Mobilization With Movement as an Adjunct Intervention in a Patient With Complicated De Quervain’s Tenosynovitis: A Case Report’, Journal of orthopaedic &amp; sports physical therapy, 2002, vol 32, p. 86 -97.