Distal femoral fracture: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
</div> | </div> | ||
== | == Introduction == | ||
[[ | [[File:Radiogr.jpg|Extra-articular distal femur fracture.|alt=|right|frameless|433x433px]]Distal femoral [[Fracture|fractures]] involve the femoral condyles and the metaphyseal region, commonly caused by high energy trauma such as motor vehicle accidents or a fall from a height. In the elderly, they may occur from [[Falls in elderly|falling]] at home.<ref name=":4">Radiopedia Distal femoral fracture Available:https://radiopaedia.org/articles/distal-femoral-fracture (accessed 11.12.2022)</ref> | ||
Distal femoral [[Fracture|fractures]] involve the femoral condyles and the metaphyseal region, commonly caused by high energy trauma such as motor vehicle accidents or a fall from a height. In the elderly, they may occur from [[Falls in elderly|falling]] at home.<ref>Radiopedia Distal femoral fracture Available:https://radiopaedia.org/articles/distal-femoral-fracture (accessed 11.12.2022)</ref> | |||
Most common types of distal femur fractures: | Most common types of distal femur fractures: | ||
| Line 13: | Line 11: | ||
* Comminuted fractures: when the bone breaks into many pieces | * Comminuted fractures: when the bone breaks into many pieces | ||
* Intra-articular fractures: when the bone extends into the knee joint | * Intra-articular fractures: when the bone extends into the knee joint | ||
== Pathology: Mechanism == | |||
== | Bimodal distribution | ||
# '''High energy fractures''': usually occur in young adults (predominantly 30year old males) and result in intra-articular fractures. Mechanism of injury commonly includes motor vehicle accidents, high-velocity missile injuries and/ or a direct blow mechanism. | # '''High energy fractures''': usually occur in young adults (predominantly 30year old males) and result in intra-articular fractures. Mechanism of injury commonly includes motor vehicle accidents, high-velocity missile injuries and/ or a direct blow mechanism. | ||
| Line 25: | Line 18: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
History: patients commonly present after fall or traumatic event. Most common symptoms of distal femur fracture include: | |||
Most common symptoms of distal femur fracture include: | |||
* Pain with [[weight bearing|weight-bearing]] | * Pain with [[weight bearing|weight-bearing]] | ||
* Swelling and bruising | * Swelling and bruising | ||
* Tenderness to touch | * Tenderness to touch | ||
* Deformity | * Deformity.<ref name=":0">Crist B., Della Rocca G., Murtha Y. [https://pubmed.ncbi.nlm.nih.gov/18705562/ Treatment of Acute Distal Femur Fractures.] ''ORTHOPEDICS.'' 2008 Jul;31(7):681-690.</ref> | ||
* In the context of polytrauma<ref name=":4" /> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
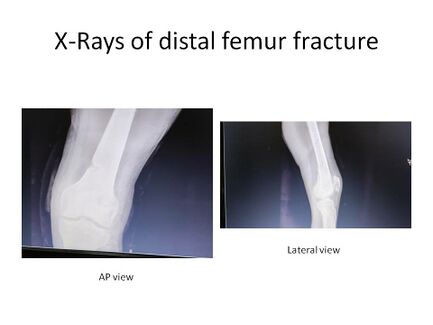
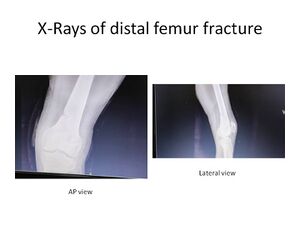
[[File:Radiogr.jpg|thumb|AP and lateral views of an extra-articular distal femur fracture.]] | [[File:Radiogr.jpg|thumb|AP and lateral views of an extra-articular distal femur fracture.]] | ||
'''Clinical/Physical examination''': the typical clinical picture during the inspection of the knee is | '''Clinical/Physical examination''': the typical clinical picture during the inspection of the knee is pain of distal femur that is made worse with knee movement and inability to weight-bear. | ||
'''Radiographic examination:''' AP and lateral views of the femur. | '''Radiographic examination:''' AP and lateral views of the femur. | ||
'''CT-scans:''' Highly recommended with high energy trauma and if an intra-articular fracture is suspected. (55% of distal femur fractures are intra-articular.) <ref name=":1" /> | '''CT-scans:''' Highly recommended with high energy trauma and if an intra-articular fracture is suspected. (55% of distal femur fractures are intra-articular.) <ref name=":1" /> | ||
[[File:AO.jpg | |||
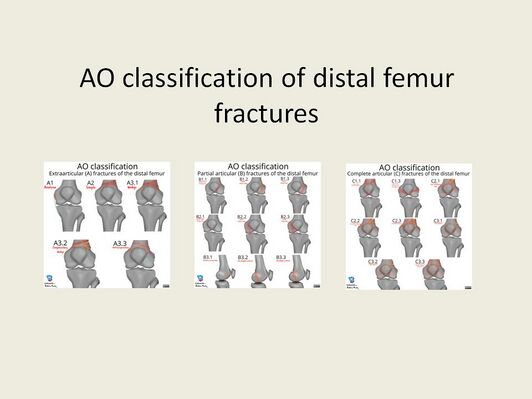
The | == Classification System == | ||
[[File:AO.jpg|Adapted from: Murphy, A., Ng, J. AO classification of distal femur fractures. Reference article, Radiopaedia.org. (accessed on 12 Aug 2022) <nowiki>https://doi.org/10.53347/rID-94057</nowiki>|alt=|right|frameless|532x532px]] | |||
The AO classification system of distal femoral fractures is a commonly utilised system by orthopaedic surgeons. | |||
* '''Type A:''' Extra-articular fractures | * '''Type A:''' Extra-articular fractures | ||
| Line 58: | Line 53: | ||
Surgical management for distal femur fractures is since the 1970s regarded superior to non-surgical management. <ref name=":2">Piétu G., Ehlinger M. [https://pubmed.ncbi.nlm.nih.gov/27867137/ Minimally invasive internal fixation of distal femur fractures.] Orthopaedics & Traumatology: Surgery & Research, 2017; 103(1): S161-S169.</ref> | Surgical management for distal femur fractures is since the 1970s regarded superior to non-surgical management. <ref name=":2">Piétu G., Ehlinger M. [https://pubmed.ncbi.nlm.nih.gov/27867137/ Minimally invasive internal fixation of distal femur fractures.] Orthopaedics & Traumatology: Surgery & Research, 2017; 103(1): S161-S169.</ref> | ||
# Surgical Interventions: Usually require open reduction and internal fixation (especially in cases of displaced or intraarticular fractures). Extra-articular or simple intra-articular fractures may be treated with intramedullary nailing and screw fixation. Simple unicondylar or epicondyle fractures may be treated with simple screw fixation. Extremely comminuted, non-reconstructable fractures or patients with pre-existing osteoarthritis might need arthroplasty.<ref name=":4" /> | |||
# Nonsurgical Interventions: Rare and considered in stable non-displaced fractures in non-ambulatory patients.<ref name=":4" /> | |||
=== Postoperative Management === | === Postoperative Management === | ||
| Line 79: | Line 67: | ||
The main aim of Physiotherapy post distal femur fracture is to get the patient back to his/ her baseline function and to prevent complications. | The main aim of Physiotherapy post distal femur fracture is to get the patient back to his/ her baseline function and to prevent complications. | ||
Whilst the patient is admitted to hospital, the Physiotherapist will teach the patient how to mobilise using the correct [[Walking Aids|walking aid,]] with the correct [[weight bearing|weight-bearing]] status as discussed with the doctor. Thorough education regarding the condition, management and rehabilitation should be given. | # Whilst the patient is admitted to hospital, the Physiotherapist will teach the patient how to mobilise using the correct [[Walking Aids|walking aid,]] with the correct [[weight bearing|weight-bearing]] status as discussed with the doctor. Thorough education regarding the condition, management and rehabilitation should be given. | ||
# Extensive physical therapy will follow surgical fixation and stabilisation of the fracture. Extensive physical therapy will include a basic progressive [[Range of Motion|range of motion]] exercises, teaching of muscle strengthening exercises, circulatory exercises and mobility/ [[Gait]] activities. | |||
Extensive physical therapy will follow surgical fixation and stabilisation of the fracture. Extensive physical therapy will include a basic progressive [[Range of Motion|range of motion]] exercises, teaching of muscle strengthening exercises, circulatory exercises and mobility/ [[Gait]] activities. | |||
'''Physical therapy management summary''': | |||
* Education (Regarding condition, surgery, complications, rehabilitation, and importance of frequent mobilisation during the day) | |||
* Management of swelling (Ice and elevation) | |||
* Mobilise patient out of bed and teach the patient on correct assistive device usage | |||
* Gait training (Weight-bearing status case-specific, but in most cases to start with PWB (15% of body weight)) | |||
* Progressive Gluteal, Quadriceps and Hamstring muscle strengthening | |||
* Progressive Knee range of motion exercises | |||
* Patellar mobility | |||
* Ankle movements and foot-pumps to aid with circulation | |||
'''Specifically for Extra-articular fractures'''<u>:</u> after the fracture has been surgically stabilised by locked plating or retrograde inter medullary nailing. Physiotherapy is indicated from Day 1 post-op. Early mobilisation without any weight-bearing limitations have good morbidity and mortality outcomes in the elderly; and also have accelerated functional recovery.<ref>Smith W., Stoneback J., Morgan S., Stahel P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5142343/ Is immediate weight bearing safe for periprosthetic distal femur fractures treated by locked plating?.] Patient Saf Surg 2016; 10:26.</ref> | |||
* Mobilisation with a walker and immediate weight-bearing (within patients tolerance levels) | * Mobilisation with a walker and immediate weight-bearing (within patients tolerance levels) | ||
* Straight leg raises | * Straight leg raises | ||
Revision as of 06:43, 11 December 2022
Top Contributors - Mande Jooste, Angeliki Chorti, Kim Jackson, Laura Ritchie, Lucinda hampton, Evan Thomas, Daphne Jackson, Admin, Leen Wyers, Karen Wilson and Claire Knott
Introduction[edit | edit source]
Distal femoral fractures involve the femoral condyles and the metaphyseal region, commonly caused by high energy trauma such as motor vehicle accidents or a fall from a height. In the elderly, they may occur from falling at home.[1]
Most common types of distal femur fractures:
- Transverse fractures : when the bone breaks straight across
- Comminuted fractures: when the bone breaks into many pieces
- Intra-articular fractures: when the bone extends into the knee joint
Pathology: Mechanism[edit | edit source]
Bimodal distribution
- High energy fractures: usually occur in young adults (predominantly 30year old males) and result in intra-articular fractures. Mechanism of injury commonly includes motor vehicle accidents, high-velocity missile injuries and/ or a direct blow mechanism.
- Low energy fractures: mostly occur in elderly people, secondary to osteoporosis (predominantly in women over 65years)[2][3][4]. These fractures most commonly occur with twisting motions or falls [5] . 4-6% of all femur fractures are distal femur fractures, and more than 85%of these occurrences are low energy fractures in the elderly.
Clinical Presentation[edit | edit source]
History: patients commonly present after fall or traumatic event. Most common symptoms of distal femur fracture include:
- Pain with weight-bearing
- Swelling and bruising
- Tenderness to touch
- Deformity.[6]
- In the context of polytrauma[1]
Diagnostic Procedures[edit | edit source]
Clinical/Physical examination: the typical clinical picture during the inspection of the knee is pain of distal femur that is made worse with knee movement and inability to weight-bear.
Radiographic examination: AP and lateral views of the femur.
CT-scans: Highly recommended with high energy trauma and if an intra-articular fracture is suspected. (55% of distal femur fractures are intra-articular.) [3]
Classification System[edit | edit source]
The AO classification system of distal femoral fractures is a commonly utilised system by orthopaedic surgeons.
- Type A: Extra-articular fractures
- Type B: Partial articular fratures, one part of the articular surface is involved and the rest of the joint is still attached to the metaphysis and diaphysis
- Type C: Complete articualr fractures, the fracture is crossing the joint surface and separated from the diaphysis
Outcome Measures[edit | edit source]
Lower Extremity Functional Scale
Management / Interventions[edit | edit source]
Surgical management for distal femur fractures is since the 1970s regarded superior to non-surgical management. [4]
- Surgical Interventions: Usually require open reduction and internal fixation (especially in cases of displaced or intraarticular fractures). Extra-articular or simple intra-articular fractures may be treated with intramedullary nailing and screw fixation. Simple unicondylar or epicondyle fractures may be treated with simple screw fixation. Extremely comminuted, non-reconstructable fractures or patients with pre-existing osteoarthritis might need arthroplasty.[1]
- Nonsurgical Interventions: Rare and considered in stable non-displaced fractures in non-ambulatory patients.[1]
Postoperative Management[edit | edit source]
- Wound dressings post-op as well as 2days post-op, or as directed by the operating doctor.
- 10-14 days post-op removal of stitches
- Mobilise with two elbow crutches; gait training; Usually PWB (15kg) (WB status is to be confirmed by the operating doctor as it is patient/ case specific)
- Stair climbing after 7-14days
- 6 weeks post-op control X-ray
- Depending on the fracture type and appearance of callus formation, you can increase weight-bearing. [8]
Physical Therapy Management[edit | edit source]
The main aim of Physiotherapy post distal femur fracture is to get the patient back to his/ her baseline function and to prevent complications.
- Whilst the patient is admitted to hospital, the Physiotherapist will teach the patient how to mobilise using the correct walking aid, with the correct weight-bearing status as discussed with the doctor. Thorough education regarding the condition, management and rehabilitation should be given.
- Extensive physical therapy will follow surgical fixation and stabilisation of the fracture. Extensive physical therapy will include a basic progressive range of motion exercises, teaching of muscle strengthening exercises, circulatory exercises and mobility/ Gait activities.
Physical therapy management summary:
- Education (Regarding condition, surgery, complications, rehabilitation, and importance of frequent mobilisation during the day)
- Management of swelling (Ice and elevation)
- Mobilise patient out of bed and teach the patient on correct assistive device usage
- Gait training (Weight-bearing status case-specific, but in most cases to start with PWB (15% of body weight))
- Progressive Gluteal, Quadriceps and Hamstring muscle strengthening
- Progressive Knee range of motion exercises
- Patellar mobility
- Ankle movements and foot-pumps to aid with circulation
Specifically for Extra-articular fractures: after the fracture has been surgically stabilised by locked plating or retrograde inter medullary nailing. Physiotherapy is indicated from Day 1 post-op. Early mobilisation without any weight-bearing limitations have good morbidity and mortality outcomes in the elderly; and also have accelerated functional recovery.[9]
- Mobilisation with a walker and immediate weight-bearing (within patients tolerance levels)
- Straight leg raises
- Seated knee extension
- Progressive quadriceps strengthening exercises[10]
Complications[edit | edit source]
- Malunion
- Delayed union
- Non-union (or breakage of the plate)
- Implant failure[3]
- Infection (superficial infection or deep infection)
- Limited range of motion
- Leg length discrepancy[11]
- Ligamentous instability[8]
Resources[edit | edit source]
Intra-articular physeal fractures[12]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Radiopedia Distal femoral fracture Available:https://radiopaedia.org/articles/distal-femoral-fracture (accessed 11.12.2022)
- ↑ Streubel P., Ricci W., Wong A., Gardner M. Mortality After Distal Femur Fractures in Elderly Patients. Clinical Orthopaedics and Related Research [Internet]. 2011 Apr 1; 469(4):1188-1196.
- ↑ 3.0 3.1 3.2 Hoskins W., Bingham R., Griffin XL. Distal femur fractures in adults. Orthopaedics and Trauma [Internet]. 2017;31(2):93–101.
- ↑ 4.0 4.1 Piétu G., Ehlinger M. Minimally invasive internal fixation of distal femur fractures. Orthopaedics & Traumatology: Surgery & Research, 2017; 103(1): S161-S169.
- ↑ Mashru R., Perez E. Fractures of the distal femur current trends in evaluation and management. Current Opinion in Orthopaedics 2007;18(1):41–48.
- ↑ Crist B., Della Rocca G., Murtha Y. Treatment of Acute Distal Femur Fractures. ORTHOPEDICS. 2008 Jul;31(7):681-690.
- ↑ Murphy A., Ng J. AO classification of distal femur fractures. Reference article, Radiopaedia.org. Available: https://doi.org/10.53347/rID-94057 (accessed on 09 Aug 2022)
- ↑ 8.0 8.1 Schandelmaier P., Blauth M., Krettek C. Internal Fixation of Distal Femur Fractures with the Less Invasive Stabilizing System (LISS). Orthopaedics and Traumatology 2001; 9(3):166–184.
- ↑ Smith W., Stoneback J., Morgan S., Stahel P. Is immediate weight bearing safe for periprosthetic distal femur fractures treated by locked plating?. Patient Saf Surg 2016; 10:26.
- ↑ Mohammed S., Hussain M., Steven K., Daily M., Frank R., Avilucea M. Stable fixation and Immediate weight bearing after combined retrograde inter medullary nailing and open reduction internal fixation of noncomminuted distal interprosthetic femur fractures. Journal of Orthopaedic trauma. June 2018; 32(6):e237-e240.
- ↑ El-Tantawy A., Atef A. Comminuted distal femur closed fractures: a new application of the Ilizarov concept of compression–distraction. Eur J Orthop Surg Traumatolo 2015 Apr 1;25(3):555–562.
- ↑ Pennock A., Ellis H., Willimon S., Wyatt C., Broida S., Dennis M., Bastrom, T. Intra-articular Physeal Fractures of the Distal Femur: A Frequently Missed Diagnosis in Adolescent Athletes. Orthop J Sports Medi 2017 Oct 10;5(10):2325967117731567.
- ↑ Nabil Ebraheim. Distal Femur Supracondylar Fracture - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: https://www.youtube.com/watch?v=kXngbbqVa9g [last accessed 8/4/2019]