Distal femoral fracture: Difference between revisions
Mande Jooste (talk | contribs) (edited anatomy section) |
No edit summary |
||
| (27 intermediate revisions by 4 users not shown) | |||
| Line 4: | Line 4: | ||
</div> | </div> | ||
== | == Introduction == | ||
[[ | [[File:Distal-femoral-fracture.png|thumb|290x290px|Distal-femoral-fracture]] | ||
Distal femoral [[Fracture|fractures]] involve the femoral condyles and the metaphyseal region, commonly caused by high energy trauma such as motor vehicle accidents or a fall from a height. In the elderly, they may occur from [[Falls in elderly|falling]] at home.<ref name=":4">Radiopedia Distal femoral fracture Available:https://radiopaedia.org/articles/distal-femoral-fracture (accessed 11.12.2022)</ref>Other names: Supracondylar femur fracture; Intercondylar femur fracture; Hoffa's Fracture. | |||
The majority of distal femur fractures require surgical intervention.<ref name=":5">Coon MS, Best BJ. Distal Femur Fractures. InStatPearls [Internet] 2021 Aug 9. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK551675/ (accessed 11.12.2022)</ref> | |||
== Pathology: Mechanism == | |||
Bimodal distribution | |||
# '''High energy fractures''': usually occur in young adults (predominantly 30year old males) and result in intra-articular fractures. Mechanism of injury commonly includes motor vehicle accidents, high-velocity missile injuries and/ or a direct blow mechanism. | |||
# '''Low energy fractures:''' mostly occur in elderly people, secondary to [[Osteoporosis disease|osteoporosis]] (predominantly in women over 65years)<ref>Streubel P., Ricci W., Wong A., Gardner M. [https://pubmed.ncbi.nlm.nih.gov/20830542/ Mortality After Distal Femur Fractures in Elderly Patients.] Clinical Orthopaedics and Related Research [Internet]. 2011 Apr 1; 469(4):1188-1196.</ref><ref name=":1">Hoskins W., Bingham R., Griffin XL. [https://www.orthopaedicsandtraumajournal.co.uk/article/S1877-1327(16)30160-9/fulltext Distal femur fractures in adults.] Orthopaedics and Trauma [Internet]. 2017;31(2):93–101. </ref><ref name=":2" />. These fractures most commonly occur with twisting motions or falls <ref>Mashru R., Perez E. [http://search.ebscohost.com.uplib.idm.oclc.org/login.aspx?direct=true&db=eoah&AN=48551848&site=pfi-live Fractures of the distal femur current trends in evaluation and management.] Current Opinion in Orthopaedics 2007;18(1):41–48. </ref> . 4-6% of all femur fractures are distal femur fractures, and more than 85%of these occurrences are low energy fractures in the elderly. | |||
High energy fractures: usually | |||
Low energy fractures: mostly | |||
== Clinical Presentation == | == Clinical Presentation == | ||
[[File:Hoffa-fracture.jpeg|thumb|Distal femur fracture]] | |||
Most common symptoms of distal femur fracture include: | History: patients commonly present after fall or traumatic event. Most common symptoms of distal femur fracture include: | ||
* Pain with [[weight bearing]] | * Pain with [[weight bearing|weight-bearing]] | ||
* Swelling and bruising | * Swelling and bruising | ||
* Tenderness to touch | * Tenderness to touch | ||
* Deformity.<ref name=":0" /> | * Deformity.<ref name=":0">Crist B., Della Rocca G., Murtha Y. [https://pubmed.ncbi.nlm.nih.gov/18705562/ Treatment of Acute Distal Femur Fractures.] ''ORTHOPEDICS.'' 2008 Jul;31(7):681-690.</ref> | ||
* In the context of polytrauma<ref name=":4" /> | |||
== Diagnostic Procedures == | |||
'''Clinical/Physical examination''': the typical clinical picture during the inspection of the knee is pain of distal femur that is made worse with knee movement and inability to weight-bear. | |||
'''Radiographic examination:''' AP and lateral views of the femur. | |||
'''CT-scans:''' Highly recommended with high energy trauma and if an intra-articular fracture is suspected. (55% of distal femur fractures are intra-articular.) <ref name=":1" /> | |||
== Classification System == | |||
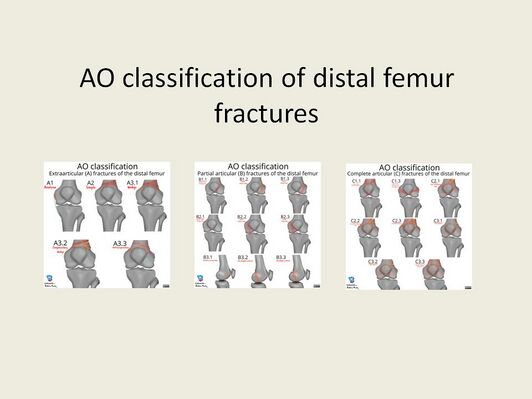
[[File:AO.jpg|Adapted from: Murphy, A., Ng, J. AO classification of distal femur fractures. Reference article, Radiopaedia.org. (accessed on 12 Aug 2022) <nowiki>https://doi.org/10.53347/rID-94057</nowiki>|alt=|right|frameless|532x532px]] | |||
The AO classification system of distal femoral fractures is a commonly utilised system by orthopaedic surgeons. | |||
* '''Type A:''' Extra-articular fractures | |||
* '''Type B:''' Partial articular fratures, one part of the articular surface is involved and the rest of the joint is still attached to the metaphysis and diaphysis | |||
* | |||
* '''Type C:''' Complete articualr fractures, the fracture is crossing the joint surface and separated from the diaphysis | |||
<ref>Murphy A., Ng J. [https://radiopaedia.org/articles/ao-classification-of-distal-femur-fractures AO classification of distal femur fractures. Reference article, Radiopaedia.org.] Available: <nowiki>https://doi.org/10.53347/rID-94057</nowiki> (accessed on 09 Aug 2022)</ref> | |||
== | == Outcome Measures == | ||
* [[Dynamic Gait Index]] | |||
* [[Lower Extremity Functional Scale (LEFS)|Lower Extremity Functional Scale]] | |||
* [[Timed Up and Go Test (TUG)|Timed Up and Go Test]] | |||
== Management / Interventions == | |||
[[File:Traction placement.jpeg|thumb|399x399px|Femur traction placement]] | |||
Surgical management for distal femur fractures is since the 1970s regarded superior to non-surgical management. <ref name=":2">Piétu G., Ehlinger M. [https://pubmed.ncbi.nlm.nih.gov/27867137/ Minimally invasive internal fixation of distal femur fractures.] Orthopaedics & Traumatology: Surgery & Research, 2017; 103(1): S161-S169.</ref> | |||
# Surgical Interventions: Usually require open reduction and internal fixation (especially in cases of displaced or intraarticular fractures). Extra-articular or simple intra-articular fractures may be treated with intramedullary nailing and screw fixation. Simple unicondylar or epicondyle fractures may be treated with simple screw fixation. Extremely comminuted, non-reconstructable fractures or patients with pre-existing osteoarthritis might need arthroplasty.<ref name=":4" /> | |||
# Nonsurgical Interventions: Rare and considered in stable non-displaced fractures in non-ambulatory patients.<ref name=":4" /> | |||
=== | === Postoperative Management === | ||
* Wound dressings post-op as well as 2days post-op, or as directed by the operating doctor. | * Wound dressings post-op as well as 2days post-op, or as directed by the operating doctor. | ||
* 10-14 days post-op removal of stitches | * 10-14 days post-op removal of stitches | ||
| Line 68: | Line 60: | ||
* Stair climbing after 7-14days | * Stair climbing after 7-14days | ||
* 6 weeks post-op control X-ray | * 6 weeks post-op control X-ray | ||
* Depending on the fracture type and appearance of callus formation, you can increase weight bearing. <ref name=":3">Schandelmaier P, Blauth M, Krettek C. Internal Fixation of Distal Femur Fractures with the Less Invasive Stabilizing System (LISS). Orthopaedics and Traumatology | * Depending on the fracture type and appearance of callus formation, you can increase weight-bearing. <ref name=":3">Schandelmaier P., Blauth M., Krettek C. [https://link.springer.com/article/10.1007/s065-001-8351-z Internal Fixation of Distal Femur Fractures with the Less Invasive Stabilizing System (LISS).] Orthopaedics and Traumatology 2001; 9(3):166–184.</ref> | ||
== Physical Therapy Management == | == Physical Therapy Management == | ||
The main aim of Physiotherapy post distal femur fracture is to get the patient back to his/ her baseline function and to prevent complications. | The main aim of Physiotherapy post distal femur fracture is to get the patient back to his/ her baseline function and to prevent complications. | ||
# Postoperatively, patients should begin gentle range of motion of the knee to prevent stiffness. | |||
# Depending on the intraoperative stability, the affected extremity may be made non-weight bearing, touchdown weight-bearing, or partial weight-bearing for 10 to 12 weeks. The physiotherapist will teach the patient how to mobilise using the correct [[Walking Aids|walking aid,]] with the correct [[weight bearing|weight-bearing]] status. | |||
# Thorough education regarding the condition, management and rehabilitation should be given. | |||
# Extensive physical therapy follows surgical fixation and stabilisation of the fracture. Will include a basic progressive [[Range of Motion|range of motion]] exercises, teaching of muscle strengthening exercises, circulatory exercises and mobility/ [[Gait]] activities. | |||
'''Physical therapy management summary''': | |||
* Education (Regarding condition, surgery, complications, rehabilitation, and importance of frequent mobilisation during the day) | |||
* Management of swelling (Ice and elevation) | |||
* Mobilise patient out of bed and teach the patient on correct assistive device usage | |||
* Gait training (Weight-bearing status case-specific, but in most cases to start with PWB (15% of body weight)) | |||
* Progressive Gluteal, Quadriceps and Hamstring muscle strengthening | |||
* Progressive Knee range of motion exercises | |||
* Patellar mobility | |||
* Ankle movements and foot-pumps to aid with circulation | |||
* Mobilisation with a walker and immediate weight bearing (within patients tolerance levels) | '''Specifically for Extra-articular fractures'''<u>:</u> after the fracture has been surgically stabilised by locked plating or retrograde inter medullary nailing. Physiotherapy is indicated from Day 1 post-op. Early mobilisation without any weight-bearing limitations have good morbidity and mortality outcomes in the elderly; and also have accelerated functional recovery.<ref>Smith W., Stoneback J., Morgan S., Stahel P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5142343/ Is immediate weight bearing safe for periprosthetic distal femur fractures treated by locked plating?.] Patient Saf Surg 2016; 10:26.</ref> | ||
* Mobilisation with a walker and immediate weight-bearing (within patients tolerance levels) | |||
* Straight leg raises | * Straight leg raises | ||
* Seated knee extension | * Seated knee extension | ||
* Progressive quadriceps strengthening exercises<ref>Mohammed S, Hussain | * Progressive quadriceps strengthening exercises<ref>Mohammed S., Hussain M., Steven K., Daily M., Frank R., Avilucea M. [https://pubmed.ncbi.nlm.nih.gov/29521874/ Stable fixation and Immediate weight bearing after combined retrograde inter medullary nailing and open reduction internal fixation of noncomminuted distal interprosthetic femur fractures.] Journal of Orthopaedic trauma. June 2018; 32(6):e237-e240.</ref> | ||
A full recovery and a return to sports or normal daily activities usually requires 4-6 months post-surgery, depending on the severity of the injury. | |||
== Complications == | == Complications == | ||
Malunion | * Pain secondary to hardware presence eg over the plate on the lateral femoral condyle where the iliotibial band may rub, medial screw irritation secondary to excessively long screws in contact with medial soft tissues. | ||
* [[Fracture Complications|Malunion]]: greater than 5 to 10 degrees affects knee mechanics, which may lead to arthritis of the medial and lateral compartments. | |||
* [[Fracture Complications|Delayed union]] or Nonunion (substantial complication, with rates up to 20%). | |||
* [[Fracture Complications|Implant failure]]<ref name=":1" /> | |||
* [[Fracture Complications|Infection (superficial infection or deep infection)]] | |||
* Limited range of motion (common)<ref name=":5" /> | |||
* [[Leg Length Discrepancy|Leg length discrepancy]]<ref>El-Tantawy A., Atef A. [https://pubmed.ncbi.nlm.nih.gov/25427781/ Comminuted distal femur closed fractures: a new application of the Ilizarov concept of compression–distraction.] Eur J Orthop Surg Traumatolo 2015 Apr 1;25(3):555–562. </ref> | |||
* Ligamentous instability<ref name=":3" /> | |||
== Resources == | |||
Intra-articular physeal fractures<ref>Pennock A., Ellis H., Willimon S., Wyatt C., Broida S., Dennis M., Bastrom, T. [https://pubmed.ncbi.nlm.nih.gov/29051906/ Intra-articular Physeal Fractures of the Distal Femur: A Frequently Missed Diagnosis in Adolescent Athletes.] Orthop J Sports Medi 2017 Oct 10;5(10):2325967117731567. </ref> | |||
{{#ev:youtube|kXngbbqVa9g|300}}<ref>Nabil Ebraheim. Distal Femur Supracondylar Fracture - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: https://www.youtube.com/watch?v=kXngbbqVa9g [last accessed 8/4/2019]</ref> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Injury]] | [[Category:Injury]] | ||
[[Category:Knee_Injuries]] | [[Category:Knee_Injuries]] | ||
[[Category:Knee]] | [[Category:Knee]] | ||
[[Category:Conditions]] | |||
[[Category:Knee - Conditions]] | |||
[[Category:Bones]] | [[Category:Bones]] | ||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | ||
[[Category:Primary Contact]] | [[Category:Primary Contact]] | ||
[[Category:Acute Care]] | [[Category:Acute Care]] | ||
[[Category:Bone Conditions | [[Category:Bone - Conditions]] | ||
Latest revision as of 08:40, 11 December 2022
Top Contributors - Mande Jooste, Angeliki Chorti, Kim Jackson, Laura Ritchie, Lucinda hampton, Evan Thomas, Daphne Jackson, Admin, Leen Wyers, Karen Wilson and Claire Knott
Introduction[edit | edit source]
Distal femoral fractures involve the femoral condyles and the metaphyseal region, commonly caused by high energy trauma such as motor vehicle accidents or a fall from a height. In the elderly, they may occur from falling at home.[1]Other names: Supracondylar femur fracture; Intercondylar femur fracture; Hoffa's Fracture.
The majority of distal femur fractures require surgical intervention.[2]
Pathology: Mechanism[edit | edit source]
Bimodal distribution
- High energy fractures: usually occur in young adults (predominantly 30year old males) and result in intra-articular fractures. Mechanism of injury commonly includes motor vehicle accidents, high-velocity missile injuries and/ or a direct blow mechanism.
- Low energy fractures: mostly occur in elderly people, secondary to osteoporosis (predominantly in women over 65years)[3][4][5]. These fractures most commonly occur with twisting motions or falls [6] . 4-6% of all femur fractures are distal femur fractures, and more than 85%of these occurrences are low energy fractures in the elderly.
Clinical Presentation[edit | edit source]
History: patients commonly present after fall or traumatic event. Most common symptoms of distal femur fracture include:
- Pain with weight-bearing
- Swelling and bruising
- Tenderness to touch
- Deformity.[7]
- In the context of polytrauma[1]
Diagnostic Procedures[edit | edit source]
Clinical/Physical examination: the typical clinical picture during the inspection of the knee is pain of distal femur that is made worse with knee movement and inability to weight-bear.
Radiographic examination: AP and lateral views of the femur.
CT-scans: Highly recommended with high energy trauma and if an intra-articular fracture is suspected. (55% of distal femur fractures are intra-articular.) [4]
Classification System[edit | edit source]
The AO classification system of distal femoral fractures is a commonly utilised system by orthopaedic surgeons.
- Type A: Extra-articular fractures
- Type B: Partial articular fratures, one part of the articular surface is involved and the rest of the joint is still attached to the metaphysis and diaphysis
- Type C: Complete articualr fractures, the fracture is crossing the joint surface and separated from the diaphysis
Outcome Measures[edit | edit source]
Management / Interventions[edit | edit source]
Surgical management for distal femur fractures is since the 1970s regarded superior to non-surgical management. [5]
- Surgical Interventions: Usually require open reduction and internal fixation (especially in cases of displaced or intraarticular fractures). Extra-articular or simple intra-articular fractures may be treated with intramedullary nailing and screw fixation. Simple unicondylar or epicondyle fractures may be treated with simple screw fixation. Extremely comminuted, non-reconstructable fractures or patients with pre-existing osteoarthritis might need arthroplasty.[1]
- Nonsurgical Interventions: Rare and considered in stable non-displaced fractures in non-ambulatory patients.[1]
Postoperative Management[edit | edit source]
- Wound dressings post-op as well as 2days post-op, or as directed by the operating doctor.
- 10-14 days post-op removal of stitches
- Mobilise with two elbow crutches; gait training; Usually PWB (15kg) (WB status is to be confirmed by the operating doctor as it is patient/ case specific)
- Stair climbing after 7-14days
- 6 weeks post-op control X-ray
- Depending on the fracture type and appearance of callus formation, you can increase weight-bearing. [9]
Physical Therapy Management[edit | edit source]
The main aim of Physiotherapy post distal femur fracture is to get the patient back to his/ her baseline function and to prevent complications.
- Postoperatively, patients should begin gentle range of motion of the knee to prevent stiffness.
- Depending on the intraoperative stability, the affected extremity may be made non-weight bearing, touchdown weight-bearing, or partial weight-bearing for 10 to 12 weeks. The physiotherapist will teach the patient how to mobilise using the correct walking aid, with the correct weight-bearing status.
- Thorough education regarding the condition, management and rehabilitation should be given.
- Extensive physical therapy follows surgical fixation and stabilisation of the fracture. Will include a basic progressive range of motion exercises, teaching of muscle strengthening exercises, circulatory exercises and mobility/ Gait activities.
Physical therapy management summary:
- Education (Regarding condition, surgery, complications, rehabilitation, and importance of frequent mobilisation during the day)
- Management of swelling (Ice and elevation)
- Mobilise patient out of bed and teach the patient on correct assistive device usage
- Gait training (Weight-bearing status case-specific, but in most cases to start with PWB (15% of body weight))
- Progressive Gluteal, Quadriceps and Hamstring muscle strengthening
- Progressive Knee range of motion exercises
- Patellar mobility
- Ankle movements and foot-pumps to aid with circulation
Specifically for Extra-articular fractures: after the fracture has been surgically stabilised by locked plating or retrograde inter medullary nailing. Physiotherapy is indicated from Day 1 post-op. Early mobilisation without any weight-bearing limitations have good morbidity and mortality outcomes in the elderly; and also have accelerated functional recovery.[10]
- Mobilisation with a walker and immediate weight-bearing (within patients tolerance levels)
- Straight leg raises
- Seated knee extension
- Progressive quadriceps strengthening exercises[11]
A full recovery and a return to sports or normal daily activities usually requires 4-6 months post-surgery, depending on the severity of the injury.
Complications[edit | edit source]
- Pain secondary to hardware presence eg over the plate on the lateral femoral condyle where the iliotibial band may rub, medial screw irritation secondary to excessively long screws in contact with medial soft tissues.
- Malunion: greater than 5 to 10 degrees affects knee mechanics, which may lead to arthritis of the medial and lateral compartments.
- Delayed union or Nonunion (substantial complication, with rates up to 20%).
- Implant failure[4]
- Infection (superficial infection or deep infection)
- Limited range of motion (common)[2]
- Leg length discrepancy[12]
- Ligamentous instability[9]
Resources[edit | edit source]
Intra-articular physeal fractures[13]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Radiopedia Distal femoral fracture Available:https://radiopaedia.org/articles/distal-femoral-fracture (accessed 11.12.2022)
- ↑ 2.0 2.1 Coon MS, Best BJ. Distal Femur Fractures. InStatPearls [Internet] 2021 Aug 9. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK551675/ (accessed 11.12.2022)
- ↑ Streubel P., Ricci W., Wong A., Gardner M. Mortality After Distal Femur Fractures in Elderly Patients. Clinical Orthopaedics and Related Research [Internet]. 2011 Apr 1; 469(4):1188-1196.
- ↑ 4.0 4.1 4.2 Hoskins W., Bingham R., Griffin XL. Distal femur fractures in adults. Orthopaedics and Trauma [Internet]. 2017;31(2):93–101.
- ↑ 5.0 5.1 Piétu G., Ehlinger M. Minimally invasive internal fixation of distal femur fractures. Orthopaedics & Traumatology: Surgery & Research, 2017; 103(1): S161-S169.
- ↑ Mashru R., Perez E. Fractures of the distal femur current trends in evaluation and management. Current Opinion in Orthopaedics 2007;18(1):41–48.
- ↑ Crist B., Della Rocca G., Murtha Y. Treatment of Acute Distal Femur Fractures. ORTHOPEDICS. 2008 Jul;31(7):681-690.
- ↑ Murphy A., Ng J. AO classification of distal femur fractures. Reference article, Radiopaedia.org. Available: https://doi.org/10.53347/rID-94057 (accessed on 09 Aug 2022)
- ↑ 9.0 9.1 Schandelmaier P., Blauth M., Krettek C. Internal Fixation of Distal Femur Fractures with the Less Invasive Stabilizing System (LISS). Orthopaedics and Traumatology 2001; 9(3):166–184.
- ↑ Smith W., Stoneback J., Morgan S., Stahel P. Is immediate weight bearing safe for periprosthetic distal femur fractures treated by locked plating?. Patient Saf Surg 2016; 10:26.
- ↑ Mohammed S., Hussain M., Steven K., Daily M., Frank R., Avilucea M. Stable fixation and Immediate weight bearing after combined retrograde inter medullary nailing and open reduction internal fixation of noncomminuted distal interprosthetic femur fractures. Journal of Orthopaedic trauma. June 2018; 32(6):e237-e240.
- ↑ El-Tantawy A., Atef A. Comminuted distal femur closed fractures: a new application of the Ilizarov concept of compression–distraction. Eur J Orthop Surg Traumatolo 2015 Apr 1;25(3):555–562.
- ↑ Pennock A., Ellis H., Willimon S., Wyatt C., Broida S., Dennis M., Bastrom, T. Intra-articular Physeal Fractures of the Distal Femur: A Frequently Missed Diagnosis in Adolescent Athletes. Orthop J Sports Medi 2017 Oct 10;5(10):2325967117731567.
- ↑ Nabil Ebraheim. Distal Femur Supracondylar Fracture - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: https://www.youtube.com/watch?v=kXngbbqVa9g [last accessed 8/4/2019]