Handling the Child with Cerebral Palsy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
<div class="editorbox"> '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
=== This page is currently under development | === This page is currently under development- and Review. Please come back soon to see the finished work!! === | ||
=== Introduction === | === Introduction === | ||
Revision as of 21:53, 17 April 2023
This page is currently under development- and Review. Please come back soon to see the finished work!![edit | edit source]
Introduction[edit | edit source]
Children with cerebral palsy present with abnormal muscle tone and movement, resulting in abnormal posture that makes it difficult to handle them [1]. Parents, caregivers, or therapists of Children with cerebral palsy, need to have knowledge and handling skills, to be able to support them. Children with cerebral palsy show atypical movements that restrict their ability to develop naturally [2], and if the child remains in an atypical position for long time, deformities may occur, and lead to a permanent disability[3]. Handling skills are important in all interventions for cerebral palsy. Good handling facilitates more purposeful active movements for a child with cerebral palsy[4].
What is Handling?[edit | edit source]
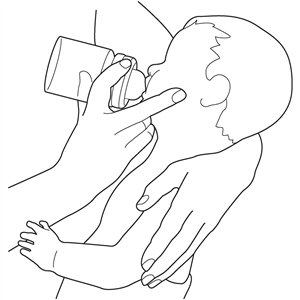
Handling is the ability of a person to position, carry/hold, and move a child with cerebral palsy [1]or other neurodevelopmental disability in such a way that his/her body achieves postural control.
It is necessary for both parents and caregivers, to have both the knowledge and handling skills, as they stay many hours per day with children. Proper handling will help a child to improve her / his physical abilities.[2].
Different research has highlighted the importance of different handling techniques that are used in handling children with cerebral palsy and their effect on muscle activation[5], and promoting postural control, among children with Cerebral Palsy[6][7][8].
Effect of sensory stimulus trough handling the child with Cerebral Palsy[edit | edit source]
Our body changes its position according to external sensory feedback[4], and this is called system sensory feedback/ feed-forward control. It is necessary to observe the child, prior to handling, because any sensory feedback from hands, or equipment will result in typical or atypical movement. Knowledge of neurologic control of the musculoskeletal system is necessary to master appropriate handling[2]. Appropriate handling of a child with cerebral Palsy leads to postural control and other benefits[9] such as:
- Normalization of tone or reduction of its abnormal influence on the body
- Maintenance of skeletal alignment and prevent future deformities.
- Providing a stable base of support to promote maximum functioning.
- Promoting tolerance to the desired position
- Promoting comfort and relaxation
- Facilitation of normal movement patterns or control of abnormal movement patterns
- Regulating pressure or preventing the development of pressure sores
- Reduction of fatigue
- Improving autonomic nervous system function (cardiac, digestive, and respiratory)
- Facilitation of maximum function with minimal pathology
Points to Consider while Handling a Child with Cerebral Palsy.[edit | edit source]
Handling a child with Cerebral Palsy needs to take into consideration the followings:
1. Observing the child first:[edit | edit source]
Through Observation, the person has information on atypical movement patterns and the presentation of the child in general.
2. Have Knowledge about the Physiopathology of Cerebral Palsy.[edit | edit source]
It is very important to know why abnormal movement patterns occur in a child with cerebral palsy and what you can do to influence the near-normal movement pattern. This knowledge will also help you make sense of what you observe and where to start while placing your hands through handling. It is also good to understand that you will not take away Cerebral palsy, but you can help the child to learn and develop to their full potential and continue to leave and enjoy life like other children without cerebral Palsy.
3. Feel the movement using your hands:[edit | edit source]
After observing a child, the person places the hands cautiously to feel the movement and see the reaction of the child.
4. Talk to the Child while handling him/Her[edit | edit source]
It is necessary to talk to the child while handling him/her because physical, communicative, and intellectual skills cannot be learned in isolation.
5. Help the child to practice![edit | edit source]
It is important to allow the child to practice the skill learned through playing and while doing all their activities of daily living such as bathing, combing, dressing, eating, toileting, etc. to master appropriate movement and posture.
6. Don't Remove support if the child has not yet mastered the skills.[edit | edit source]
Even if the child can maintain a good posture for some time, you must understand that what you have accomplished in one session will not necessarily continue when you take your hands away. It takes time and needs to be practiced in the child's daily life.
7. Make handling Fun and Active![edit | edit source]
In a natural way, children learn while they are playing, it is necessary for making the handling playful to help the child maximize their learning and be actively engaged throughout the session.
Low Resource Settings[edit | edit source]
Children with cerebral Palsy from Low and Middle -income countries (LMICs) face different challenges compared to peers from developed countries [10]. They are confronted with family conflict and discrimination, poverty, lack of qualified human resources for rehabilitation, Cultural and religious beliefs, etc.
In such context, skills are transferred to parents and caregivers to improve the quality of life of children with cerebral palsy and that of their Families. Different successful interventions such as Hambisela project, and Baby Ubuntu project have nice resources for handling children with Cerebral Palsy[11][12].
References[edit | edit source]
- ↑ 1.0 1.1 Nancy Finnie,Handling the Young Child with Cerebral Palsy at Home, 4th Edition edited by Eva Bower, Annabel Milne, 2008
- ↑ 2.0 2.1 2.2 Archie Hinchcliffe, Children with cerebral palsy: A manual for therapists, parents and community workers, second edition published in 2007.
- ↑ Pérez-de la Cruz S. Parálisis cerebral infantil y el uso de sistemas de posicionamiento para el control postural : estado actual delarte.Neurología.2017;32:610—615.
- ↑ 4.0 4.1 Freeman Miller, MD, Cerebral Palsy, 2005, ISBN 0-387-20437-7
- ↑ Paludo, T., Zardo, F., de Mattos, B. T. P., Frata, B., Ling, C. C., de Castro Barroso, G., & Cechetti, F. (2022). Measuring muscle activation using electromyography during neurodevelopmental treatment in individuals with severe cerebral palsy. Journal of back and musculoskeletal rehabilitation, 10.3233/BMR-220113. Advance online publication. https://doi.org/10.3233/BMR-220113
- ↑ Bain K, Chapparo C. The impact of neurodevelopmental treatment on the performance of daily living tasks by children with cerebral palsy. Developmental medicine and child neurology, 2012, 54, 51 | added to CENTRAL: 31 October 2014 | 2014 Issue 10 https://doi.org/10.1111/j.1469-8749.2012.04289.x
- ↑ Acar, G., Ejraei, N., Turkdoğan, D., Enver, N., Öztürk, G., & Aktaş, G. (2022). The Effects of Neurodevelopmental Therapy on Feeding and Swallowing Activities in Children with Cerebral Palsy. Dysphagia, 37(4), 800–811. https://doi.org/10.1007/s00455-021-10329-w
- ↑ Ejraei, N., Ozer, A. Y., Aydogdu, O., Turkdogan, D., & Polat, M. G. (2021). The effect of neck-trunk stabilization exercises in cerebral palsy: randomized controlled trial. Minerva pediatrics, 10.23736/S2724-5276.21.06206-6. Advance online publication. https://doi.org/10.23736/S2724-5276.21.06206-6
- ↑ Warutkar, V. B., & Krishna Kovela, R. (2022). Review of Sensory Integration Therapy for Children With Cerebral Palsy. Cureus, 14(10), e30714. https://doi.org/10.7759/cureus.30714
- ↑ Bizzego, A., Lim, M., Schiavon, G., & Esposito, G. (2020). Children with Developmental Disabilities in Low- and Middle-Income Countries: More Neglected and Physically Punished. International journal of environmental research and public health, 17(19), 7009. https://doi.org/10.3390/ijerph17197009
- ↑ Benfer, K. A., Novak, I., Morgan, C., Whittingham, K., Khan, N. Z., Ware, R. S., Bell, K. L., Bandaranayake, S., Salt, A., Ghosh, A. K., Bhattacharya, A., Samanta, S., Moula, G., Bose, D., Tripathi, S., & Boyd, R. N. (2018). Community-based parent-delivered early detection and intervention programme for infants at high risk of cerebral palsy in a low-resource country (Learning through Everyday Activities with Parents (LEAP-CP): protocol for a randomised controlled trial. BMJ open, 8(6), e021186. https://doi.org/10.1136/bmjopen-2017-021186
- ↑ Tann, Cally J; Kohli-Lynch, Maya; Nalugya, Ruth; Sadoo, Samantha; Martin, Karen; Lassman, Rachel; Nanyunja, Carol; Musoke, Margaret; Sewagaba, Margaret; Nampijja, Margaret; Seeley, Janet; Webb, Emily L; (2020) Surviving and Thriving: Early Intervention for Neonatal Survivors With Developmental Disability in Uganda. Infants & Young Children, 34 (1). pp. 17-32. ISSN 0896-3746 DOI: https://doi.org/10.1097/IYC.0000000000000182