Hemothorax: Difference between revisions
Kim Jackson (talk | contribs) No edit summary |
m (Added research from Th eLatest Specialities) |
||
| (2 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|Claire Knott]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:User Name|Claire Knott]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
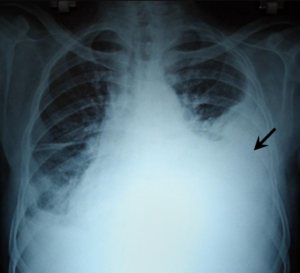
The term hemothorax can be defined as the entry of pleural fluid and blood into the pleural cavity. It needs to be pleural fluid with a hematocrit of 25% - 50% of the patient’s blood to be diagnosed as a hemothorax.<ref name=":0">Patrini D, Panagiotopoulos N, Pararajasingham J, Gvinianidze L, Iqbal Y, Lawrence DR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4387396/pdf/jtd-07-03-520.pdf Etiology and management of spontaneous haemothorax]. Journal of thoracic disease. 2015 Mar;7(3):520.</ref> | [[File:Hemothorax right side.png|thumb|[https://commons.wikimedia.org/wiki/File:PMC2567296_1757-1626-1-225-2.png Massive right-sided pleural effusion later shown to be a hemothorax]]]The term hemothorax can be defined as the entry of pleural fluid and blood into the pleural cavity. It needs to be pleural fluid with a hematocrit of 25% - 50% of the patient’s blood to be diagnosed as a hemothorax.<ref name=":0">Patrini D, Panagiotopoulos N, Pararajasingham J, Gvinianidze L, Iqbal Y, Lawrence DR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4387396/pdf/jtd-07-03-520.pdf Etiology and management of spontaneous haemothorax]. Journal of thoracic disease. 2015 Mar;7(3):520.</ref> | ||
== | == Pathophysiology == | ||
There are two layers of pleura. One of which covers the lung surface (visceral pleura) and the other the inside of the chest wall (parietal pleura). These layers of pleura adhere to each other to keep the lung from collapsing, even with the expiration of air from the lung. If air or fluid enters the pleural cavity in between these layers of pleura, it causes the lung to collapse due to its elastic recoil. If it is only air entering the pleural cavity it causes a [[pneumothorax]]. If it is fluid or blood entering the pleural cavity it could cause a pleural effusion or hemothorax. | There are two layers of pleura. One of which covers the lung surface (visceral pleura) and the other the inside of the chest wall (parietal pleura). (For more detailed information on [[Lung Anatomy|lung anatomy]]).These layers of pleura adhere to each other to keep the lung from collapsing, even with the expiration of air from the lung. If air or fluid enters the pleural cavity in between these layers of pleura, it causes the lung to collapse due to its elastic recoil. If it is only air entering the pleural cavity it causes a [[pneumothorax]]. If it is fluid or blood entering the pleural cavity it could cause a pleural effusion or hemothorax.<ref name=":1">Boersma WG, Stigt JA, Smit HJ. Treatment of haemothorax. Respiratory medicine. 2010 Nov 1;104(11):1583-7.</ref> | ||
== Aetiology == | |||
The primary cause of haemothorax is sharp or blunt trauma to the chest. Iatrogenic or spontaneous haemothorax occur less frequently. Iatrogenic haemothorax most likely occurs as a complication of cardiopulmonary surgery, placement of subclavian or jugular catheters, or lung and pleural-biopsies.<ref name=":0" /><ref name=":2">Yeam I, Sassoon C. Haemothorax and chylothorax. Curr Opin Pulm Med 1997;3:310e4.</ref> Spontaneous haemothorax is generally caused by rupture of pleural adhesions, neoplasm, pleural metastasis, and as a complication of anticoagulant therapy for pulmonary embolisms. <ref name=":3">Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, Luketich JD, Panacek EA, Sahn SA. AACP Pneumothorax Consensus Group. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest 2001 Feb;119(2):590e602.</ref> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
* Chest Pain | |||
* | * Dyspnoea | ||
* Fever | |||
* Tachycardia | |||
* Reduced breath sounds on the affected side | |||
* Pallor | |||
* Cold Sweats | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
* Chest X-ray | * [[Chest X-Rays|Chest X-ray]] | ||
* Ultrasound | * [[Ultrasound Scans|Ultrasound]] | ||
* CT scan | * [[CT Scans|CT scan]] | ||
* MRI scan | * [[MRI Scans|MRI scan]] | ||
== Medical Management == | == Medical Management == | ||
Initial management in most cases is through chest tube drainage where a large tube as an adequate initial approach unless an aortic dissection or rupture is suspected.<ref name=":2" /> (For more information on [[Chest Drains|chest drains]]). After the tube thoracostomy has been performed, a chest X-ray CXR should be repeated in order to identify the position of the chest tube, to reveal other intrathoracic pathology and to confirm whether the collection of blood within the pleural cavity has been fully drained.<ref name=":3" /><ref name=":1" /> The PLeural Effusion And Symptom Evaluation (PLEASE) Study findings reveal an improvement in breathlessness and exercise tolerance in most patients with symptomatic pleural effusion after drainage<ref>Muruganandan S, Azzopardi M, Thomas R, Fitzgerald DB, Kuok YJ, Cheah HM, Read CA, Budgeon CA, Eastwood PR, Jenkins S, Singh B. [https://pubmed.ncbi.nlm.nih.gov/32079642/ The PLeural Effusion And Symptom Evaluation (PLEASE) study of breathlessness in patients with a symptomatic pleural effusion.] European Respiratory Journal. 2020 Jan 1.</ref>. | |||
Occasionally a surgical exploration may be used. This may be indicated if there is blood loss via the chest drain over 1,500 ml in 24 hours or 200 ml per hour during several successive hours and the need for repeated blood transfusions to maintain haemodynamic stability.<ref>Ali HA, Lippmann M, Mundathaje U, Khaleeq G. Spontaneous hemothorax: a comprehensive review. Chest 2008;134:1056e65.</ref><ref>Liu D-W, Liu H-P, Lin PJ, et al. Video-assisted thoracic surgery in treatment of chest trauma. J Trauma 1997;42:670e4.</ref><ref>Lowdermilk GA, Naunheim KS. Thoracoscopic evaluation and treatment of thoracic trauma. Surg Clin North Am 2000;80: 1535e42.</ref> Patients who present with active blood loss but stable haemodynamics may be treated with Video-Assisted Thoracoscopic Surgery (VATS). This may be used to stop the bleeding and also in the evacuation of blood clots and breakdown of adhesions. A thoracotomy is the procedure of choice for surgical exploration of the chest when a massive haemothorax or persistent bleeding is present.<ref name=":1" /> | |||
== Physiotherapy Management == | == Physiotherapy Management == | ||
| Line 28: | Line 32: | ||
* The patient's clinical picture should lead the physiotherapist in deciding what treatment is suitable. | * The patient's clinical picture should lead the physiotherapist in deciding what treatment is suitable. | ||
* If the patient has a chest tube and intercostal drain in, the treatment might be different from when the patient had surgery. | * If the patient has a chest tube and intercostal drain in, the treatment might be different from when the patient had surgery. | ||
* Help to improve ventilation, oxygenation and to re-inflate | * Help to improve ventilation, oxygenation and to re-inflate atelectatic lung areas. This could be done through deep breathing exercise techniques. | ||
* Help to improve the patient's exercise tolerance and mobility. This could be done by assisting with mobilisation or general strengthening exercises. | * Help to improve the patient's exercise tolerance and mobility. This could be done by assisting with mobilisation or general strengthening exercises. | ||
* Help to maintain airway clearance. This could be done by showing the patient assisted coughing techniques to help clear any secretions. | * Help to maintain airway clearance. This could be done by showing the patient assisted coughing techniques to help clear any secretions. | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Through imaging, the diagnosis of a [[pneumothorax]] needs to be | Through imaging, the diagnosis of a [[pneumothorax]] needs to be canceled out. The hematocrit of the fluid from the pleural cavity could also be tested to see if it could be diagnosed as a pleural effusion or a hemothorax. | ||
== References == | |||
<references /> | <references /> | ||
[[Category:Primary Contact]] | [[Category:Primary Contact]] | ||
[[Category:Acute Care]] | [[Category:Acute Care]] | ||
[[Category:Medical]] | [[Category:Medical]] | ||
Latest revision as of 09:20, 8 May 2020
Introduction[edit | edit source]
The term hemothorax can be defined as the entry of pleural fluid and blood into the pleural cavity. It needs to be pleural fluid with a hematocrit of 25% - 50% of the patient’s blood to be diagnosed as a hemothorax.[1]
Pathophysiology[edit | edit source]
There are two layers of pleura. One of which covers the lung surface (visceral pleura) and the other the inside of the chest wall (parietal pleura). (For more detailed information on lung anatomy).These layers of pleura adhere to each other to keep the lung from collapsing, even with the expiration of air from the lung. If air or fluid enters the pleural cavity in between these layers of pleura, it causes the lung to collapse due to its elastic recoil. If it is only air entering the pleural cavity it causes a pneumothorax. If it is fluid or blood entering the pleural cavity it could cause a pleural effusion or hemothorax.[2]
Aetiology[edit | edit source]
The primary cause of haemothorax is sharp or blunt trauma to the chest. Iatrogenic or spontaneous haemothorax occur less frequently. Iatrogenic haemothorax most likely occurs as a complication of cardiopulmonary surgery, placement of subclavian or jugular catheters, or lung and pleural-biopsies.[1][3] Spontaneous haemothorax is generally caused by rupture of pleural adhesions, neoplasm, pleural metastasis, and as a complication of anticoagulant therapy for pulmonary embolisms. [4]
Clinical Presentation[edit | edit source]
- Chest Pain
- Dyspnoea
- Fever
- Tachycardia
- Reduced breath sounds on the affected side
- Pallor
- Cold Sweats
Diagnostic Procedures[edit | edit source]
Medical Management[edit | edit source]
Initial management in most cases is through chest tube drainage where a large tube as an adequate initial approach unless an aortic dissection or rupture is suspected.[3] (For more information on chest drains). After the tube thoracostomy has been performed, a chest X-ray CXR should be repeated in order to identify the position of the chest tube, to reveal other intrathoracic pathology and to confirm whether the collection of blood within the pleural cavity has been fully drained.[4][2] The PLeural Effusion And Symptom Evaluation (PLEASE) Study findings reveal an improvement in breathlessness and exercise tolerance in most patients with symptomatic pleural effusion after drainage[5].
Occasionally a surgical exploration may be used. This may be indicated if there is blood loss via the chest drain over 1,500 ml in 24 hours or 200 ml per hour during several successive hours and the need for repeated blood transfusions to maintain haemodynamic stability.[6][7][8] Patients who present with active blood loss but stable haemodynamics may be treated with Video-Assisted Thoracoscopic Surgery (VATS). This may be used to stop the bleeding and also in the evacuation of blood clots and breakdown of adhesions. A thoracotomy is the procedure of choice for surgical exploration of the chest when a massive haemothorax or persistent bleeding is present.[2]
Physiotherapy Management[edit | edit source]
There are no published data regarding the physiotherapy management of patients with pneumothorax or hemothorax.
The following can be regarded as recommendations for management of patients with hemothorax:
- The patient's clinical picture should lead the physiotherapist in deciding what treatment is suitable.
- If the patient has a chest tube and intercostal drain in, the treatment might be different from when the patient had surgery.
- Help to improve ventilation, oxygenation and to re-inflate atelectatic lung areas. This could be done through deep breathing exercise techniques.
- Help to improve the patient's exercise tolerance and mobility. This could be done by assisting with mobilisation or general strengthening exercises.
- Help to maintain airway clearance. This could be done by showing the patient assisted coughing techniques to help clear any secretions.
Differential Diagnosis[edit | edit source]
Through imaging, the diagnosis of a pneumothorax needs to be canceled out. The hematocrit of the fluid from the pleural cavity could also be tested to see if it could be diagnosed as a pleural effusion or a hemothorax.
References[edit | edit source]
- ↑ 1.0 1.1 Patrini D, Panagiotopoulos N, Pararajasingham J, Gvinianidze L, Iqbal Y, Lawrence DR. Etiology and management of spontaneous haemothorax. Journal of thoracic disease. 2015 Mar;7(3):520.
- ↑ 2.0 2.1 2.2 Boersma WG, Stigt JA, Smit HJ. Treatment of haemothorax. Respiratory medicine. 2010 Nov 1;104(11):1583-7.
- ↑ 3.0 3.1 Yeam I, Sassoon C. Haemothorax and chylothorax. Curr Opin Pulm Med 1997;3:310e4.
- ↑ 4.0 4.1 Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, Luketich JD, Panacek EA, Sahn SA. AACP Pneumothorax Consensus Group. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest 2001 Feb;119(2):590e602.
- ↑ Muruganandan S, Azzopardi M, Thomas R, Fitzgerald DB, Kuok YJ, Cheah HM, Read CA, Budgeon CA, Eastwood PR, Jenkins S, Singh B. The PLeural Effusion And Symptom Evaluation (PLEASE) study of breathlessness in patients with a symptomatic pleural effusion. European Respiratory Journal. 2020 Jan 1.
- ↑ Ali HA, Lippmann M, Mundathaje U, Khaleeq G. Spontaneous hemothorax: a comprehensive review. Chest 2008;134:1056e65.
- ↑ Liu D-W, Liu H-P, Lin PJ, et al. Video-assisted thoracic surgery in treatment of chest trauma. J Trauma 1997;42:670e4.
- ↑ Lowdermilk GA, Naunheim KS. Thoracoscopic evaluation and treatment of thoracic trauma. Surg Clin North Am 2000;80: 1535e42.