Lateral Epicondyle Tendinopathy (Tennis Elbow) Toolkit: Difference between revisions
Kim Jackson (talk | contribs) (Updated link to new page) |
Kim Jackson (talk | contribs) No edit summary |
||
| (8 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Kim Jackson|Kim Jackson]] for '''The BC Physical Therapy Tendinopathy Task Force:''' | '''Original Editor '''- [[User:Kim Jackson|Kim Jackson]] for '''The BC Physical Therapy Tendinopathy Task Force:''' | ||
Dr. Joseph Anthony, Paul Blazey, Dr. Allison Ezzat, Dr. Angela Fearon, Diana Hughes, Carol Kennedy, Dr. Alex Scott, Michael Yates and Alison Hoens | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction== | == Introduction== | ||
Translation of knowledge to practice in health care is a significant challenge<ref name="Groth 20112">Groth G. Predicting intentions to use research evidence for carpal tunnel syndrome treatment decisions among certified hand therapists. J Occup Rehabil. 2011;21(4):559-72.</ref><ref name="Mitton 20072">Mitton C, Adair CE, McKenzie E, Patten SB, Waye Perry B. Knowledge transfer and exchange: Review and synthesis of the literature. The Milbank Quarterly.2007;85(4):729-768.</ref><ref name="Oborn 20102">Oborn E, et al: Knowledge translation in healthcare: A review of the literature. Cambridge Judge Business School. Cambridge. 2010.</ref>. Clinicians want to provide evidence-informed management of tendinopathy but many struggle with accessing, appraising and synthesizing the vast array of literature available on this topic. As a result a [[British Columbia Physical Therapy Knowledge Broker Project|project]] was undertaken by a unique partnership of physical therapy researchers, educators and expert clinicians to address the gap between evidence and practice in the management of Lateral | Translation of knowledge to practice in health care is a significant challenge<ref name="Groth 20112">Groth G. Predicting intentions to use research evidence for carpal tunnel syndrome treatment decisions among certified hand therapists. J Occup Rehabil. 2011;21(4):559-72.</ref><ref name="Mitton 20072">Mitton C, Adair CE, McKenzie E, Patten SB, Waye Perry B. Knowledge transfer and exchange: Review and synthesis of the literature. The Milbank Quarterly.2007;85(4):729-768.</ref><ref name="Oborn 20102">Oborn E, et al: Knowledge translation in healthcare: A review of the literature. Cambridge Judge Business School. Cambridge. 2010.</ref>. Clinicians want to provide evidence-informed management of tendinopathy but many struggle with accessing, appraising and synthesizing the vast array of literature available on this topic. As a result a [[British Columbia Physical Therapy Knowledge Broker Project|project]] was undertaken by a unique partnership of physical therapy researchers, educators and expert clinicians to address the gap between evidence and practice in the management of Lateral Epicondyle Tendinopathy (LET). The original toolkit was produced in June 2013, and since its release it has been viewed more than 100,000 times worldwide. | ||
To keep the toolkit contemporary, a | To keep the toolkit contemporary, a British Columbia (BC) Physical Therapy Knowledge-Broker facilitated project team reviewed and re-released an updated version of the [https://physicaltherapy.med.ubc.ca/physical-therapy-knowledge-broker/lateral-epicondyle-tendinopathy-let-toolkit/ Lateral Epicondyle Tendinopathy toolkit] in 2022. The 2022 update includes the latest evidence, new sections to support clinical decision-making, and an engaging new look and feel! What follows is a modified version of the toolkit for Physiopedia produced in collaboration with the authorship team. | ||
==The Lateral | ==The Lateral Epicondyle Tendinopathy Toolkit == | ||
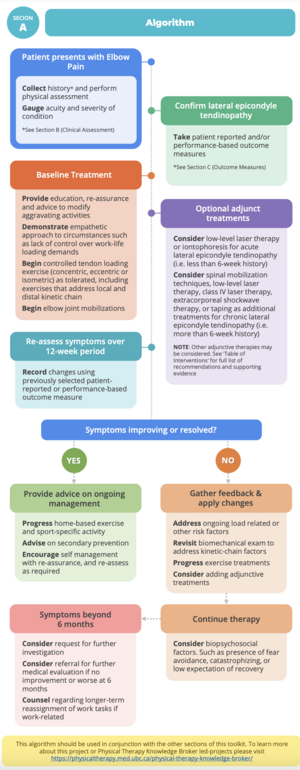
This [[Clinical Decision Making in Physiotherapy Practice|decision‐making tool]] is evidence‐informed and where there is insufficient evidence, expert‐informed. It is not intended to replace the clinician’s clinical reasoning skills and inter‐professional collaboration. ‘Acute’ refers primarily to symptoms of less than 3 months duration and 'chronic' to greater than 3 months. For studies which (1) included participants with symptoms that encompassed both acute and chronic stages or (2) did not clarify the duration of symptoms, the results have been | This [[Clinical Decision Making in Physiotherapy Practice|decision‐making tool]] is evidence‐informed and where there is insufficient evidence, expert‐informed. It is not intended to replace the clinician’s clinical reasoning skills and inter‐professional collaboration. ‘Acute’ refers primarily to symptoms of less than 3 months duration and 'chronic' to greater than 3 months. For studies which: (1) included participants with symptoms that encompassed both acute and chronic stages or (2) did not clarify the duration of symptoms, the results have been reported within the 'chronic' stage.. | ||
The following algorithm, taken from the toolkit, suggests the steps to follow to help guide the treatment and improve outcomes of a patient presenting with LET: | The following algorithm, taken from the toolkit, suggests the steps to follow to help guide the treatment and improve outcomes of a patient presenting with LET: | ||
[ | [[File:LET Algorithm.png|frameless]] | ||
The other sections provide physical therapists with summary of the evidence and recommendations for interventions (Section D | The other sections provide physical therapists with summary of the evidence and recommendations for interventions ([[Lateral Epicondyle Tendinopathy Toolkit: Section D - Summary of the Evidence|Section D]]) commonly used to manage tendinopathy of the lateral epicondyle, as well as insights into: | ||
* '''Clinical assessment of LET -''' Section B | * '''Clinical assessment of LET -''' [[Lateral Epicondyle Tendinopathy Toolkit: Section B - Clinical Assessment|Section B]] of the toolkit discusses the clinical evaluation of somebody who has been diagnosed with Lateral Epicondyle Tendinopathy - identifies the potential risk factors association with LET, the Subjective Symptoms, Biopsychological Factors, Objective Signs, Imaging and Differential Diagnosis. | ||
* '''Outcome Measures''' - Section C | * '''Outcome Measures''' - [[Lateral Epicondyle Tendinopathy Toolkit: Section C - Outcome Measures|Section C]] presents patient-reported and performance-based outcome measures that are commonly reported in the literature, supported by expert opinion or often used clinically. | ||
* '''Summary of the evidence''' - [[Lateral Epicondyle Tendinopathy Toolkit: Section D - Summary of the Evidence|Section D]] provides a summary of the evidence and recommendations for interventions | * '''Summary of the evidence''' - [[Lateral Epicondyle Tendinopathy Toolkit: Section D - Summary of the Evidence|Section D]] provides a summary of the evidence and recommendations for interventions | ||
** Manual therapy (elbow joint & spinal mobilizations; soft tissue techniques) | ** Manual therapy (elbow joint & spinal mobilizations; soft tissue techniques) | ||
| Line 37: | Line 35: | ||
* '''Exercise prescription''' - [[Lateral Epicondyle Tendinopathy Toolkit: Section E - Exercise Prescription|Section E]] will guide you through the recommended isometric, concentric and eccentric exercises based on patient preference, and clinical evaluation. | * '''Exercise prescription''' - [[Lateral Epicondyle Tendinopathy Toolkit: Section E - Exercise Prescription|Section E]] will guide you through the recommended isometric, concentric and eccentric exercises based on patient preference, and clinical evaluation. | ||
* '''Manual therapy''' - [[Lateral Epicondyle Tendinopathy Toolkit: Section F - Manual Therapy|Section F]] This section will provide you with an overview of manual therapy techniques that are effective at treating LET | * '''Manual therapy''' - [[Lateral Epicondyle Tendinopathy Toolkit: Section F - Manual Therapy|Section F]] This section will provide you with an overview of manual therapy techniques that are effective at treating LET | ||
* '''LASER dosage calculation''' - Section G | * '''LASER dosage calculation''' - [[Lateral Epicondyle Tendinopathy Toolkit: Section G - LASER Dosage Calculation|Section G]] discusses the current recommendations and dosage calculation for prescribing low level laser therapy | ||
* '''Braces, splints and taping''' - Section H | * '''Braces, splints and taping''' - [[Lateral Epicondyle Tendinopathy Toolkit: Section H - Braces, Splints, and Taping|Section H]] Describes various devices and interventions that are effective in the treatment of LET | ||
==Resources== | ==Resources== | ||
Latest revision as of 16:40, 12 February 2024
Original Editor - Kim Jackson for The BC Physical Therapy Tendinopathy Task Force:
Dr. Joseph Anthony, Paul Blazey, Dr. Allison Ezzat, Dr. Angela Fearon, Diana Hughes, Carol Kennedy, Dr. Alex Scott, Michael Yates and Alison Hoens
Top Contributors - Evan Thomas, Kim Jackson, Admin, Simisola Ajeyalemi, Wanda van Niekerk, Cindy John-Chu, Lucy Aird and Rucha GadgilIntroduction[edit | edit source]
Translation of knowledge to practice in health care is a significant challenge[1][2][3]. Clinicians want to provide evidence-informed management of tendinopathy but many struggle with accessing, appraising and synthesizing the vast array of literature available on this topic. As a result a project was undertaken by a unique partnership of physical therapy researchers, educators and expert clinicians to address the gap between evidence and practice in the management of Lateral Epicondyle Tendinopathy (LET). The original toolkit was produced in June 2013, and since its release it has been viewed more than 100,000 times worldwide.
To keep the toolkit contemporary, a British Columbia (BC) Physical Therapy Knowledge-Broker facilitated project team reviewed and re-released an updated version of the Lateral Epicondyle Tendinopathy toolkit in 2022. The 2022 update includes the latest evidence, new sections to support clinical decision-making, and an engaging new look and feel! What follows is a modified version of the toolkit for Physiopedia produced in collaboration with the authorship team.
The Lateral Epicondyle Tendinopathy Toolkit[edit | edit source]
This decision‐making tool is evidence‐informed and where there is insufficient evidence, expert‐informed. It is not intended to replace the clinician’s clinical reasoning skills and inter‐professional collaboration. ‘Acute’ refers primarily to symptoms of less than 3 months duration and 'chronic' to greater than 3 months. For studies which: (1) included participants with symptoms that encompassed both acute and chronic stages or (2) did not clarify the duration of symptoms, the results have been reported within the 'chronic' stage..
The following algorithm, taken from the toolkit, suggests the steps to follow to help guide the treatment and improve outcomes of a patient presenting with LET:
The other sections provide physical therapists with summary of the evidence and recommendations for interventions (Section D) commonly used to manage tendinopathy of the lateral epicondyle, as well as insights into:
- Clinical assessment of LET - Section B of the toolkit discusses the clinical evaluation of somebody who has been diagnosed with Lateral Epicondyle Tendinopathy - identifies the potential risk factors association with LET, the Subjective Symptoms, Biopsychological Factors, Objective Signs, Imaging and Differential Diagnosis.
- Outcome Measures - Section C presents patient-reported and performance-based outcome measures that are commonly reported in the literature, supported by expert opinion or often used clinically.
- Summary of the evidence - Section D provides a summary of the evidence and recommendations for interventions
- Manual therapy (elbow joint & spinal mobilizations; soft tissue techniques)
- Exercise
- Acupuncture
- Dry needling
- Low-Level Laser Therapy
- High-Intensity LASER
- Ultrasound
- Extracorporeal Shock Wave Therapy
- Iontophoresis
- Orthotic Devices
- Taping
- Exercise prescription - Section E will guide you through the recommended isometric, concentric and eccentric exercises based on patient preference, and clinical evaluation.
- Manual therapy - Section F This section will provide you with an overview of manual therapy techniques that are effective at treating LET
- LASER dosage calculation - Section G discusses the current recommendations and dosage calculation for prescribing low level laser therapy
- Braces, splints and taping - Section H Describes various devices and interventions that are effective in the treatment of LET
Resources[edit | edit source]
References[edit | edit source]
- ↑ Groth G. Predicting intentions to use research evidence for carpal tunnel syndrome treatment decisions among certified hand therapists. J Occup Rehabil. 2011;21(4):559-72.
- ↑ Mitton C, Adair CE, McKenzie E, Patten SB, Waye Perry B. Knowledge transfer and exchange: Review and synthesis of the literature. The Milbank Quarterly.2007;85(4):729-768.
- ↑ Oborn E, et al: Knowledge translation in healthcare: A review of the literature. Cambridge Judge Business School. Cambridge. 2010.