Lateral Epicondylitis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 184: | Line 184: | ||
<rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1XgES5aR9nB76Akn-f96Jur17dpvEooITsW2_CWVDashdJr11y|charset=UTF-8|short|max=10</rss> | <rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1XgES5aR9nB76Akn-f96Jur17dpvEooITsW2_CWVDashdJr11y|charset=UTF-8|short|max=10</rss> | ||
< | <br> | ||
<br> | |||
</div> | |||
== References == | == References == | ||
Revision as of 00:13, 8 July 2013
Original Editors - Assia Dad as part of the Vrije Universiteit Brussel's Evidence-based Practice project, Hannah Norton, Elien Vanderlinden Charlotte Siragò, Kim Pisse, Joyce De Gelas, Tessa de Jongh
Top Contributors - Angeliki Chorti, Adam Vallely Farrell, Admin, Charlotte Sirago, Elien Vanderlinden, Nikhil Benhur Abburi, Vanwymeersch Celine, Kim Jackson, Johnathan Fahrner, Celien Van den Meerssche, Rachael Lowe, Evan Thomas, Hannah Norton, Assia Dad, Ruben Vellemans, Simisola Ajeyalemi, Kai A. Sigel, Quentin Desantoine, Jelien Wouters, Wanda van Niekerk, Maëlle Cormond, Pacifique Dusabeyezu, Naomi O'Reilly, Irene Leahy, Jolien Rottie, Wendy Walker and Candace Goh
Definition/Description[edit | edit source]
Lateral epicondylitis is the most common overuse syndrome in the elbow. Lateral epicondylitis or tennis elbow is an injury involving the extensor muscles of the forearm. These muscles originate on the lateral epicondylar region of the distal of the humerus.[1]
[2] [3] [4]The most common type of lateral elbow pain is lateral epiconylitis. In occupations requiring repetitive upper extremity activities and particularly those involving computer use, heavy lifting, forceful forearm pronation and supination, and repetitive vibration, lateral epicondylitis is repeatedly seen. The clinical examination of lateral epicondylitis is often clear. This is shown with local tenderness over the common forearm extensor tendon insertion at the lateral epicondyle. This can be extended to the extensor mass, with less annular ligament. Pain can be reproduced with resisted wrist and middle finger extension and with gripping activities. It is possible that symptoms are generated by passive wrist flexion with elbow extension. It is often seen that the flexibility and the strength in the wrist extensor and posterior shoulder muscles are deficient. However, in the workplace where repetitive elbow and wrist motion is involved, lateral epicondylitis occurs. On the lateral epicondyle it’s about 7 times more common than on the medial epicondyle.
In a lot of cases of this specific pathology, the insertion of the extensor carpi radialis brevis is involved. However the extensor carpi radialis longus and anterior extensor communis tendons rarely occur. The description of microscopic failure at the enthesis is a result of repetitive overuse of the extensor forearm muscles. Pathology research has added mucinioid degeneration and granulation tissue in the subtendinous space.
Today, the state of lateral epicondylitis is well known to arise spontaneously or in combination with other recreational and occupational pursuits.
Recently, researchers have advised using the terms “tendinosis” or “tendinopathy” to reflect the chronicity of the condition because a lack of acute inflammatory markers in patients with tennis elbow is indicated.
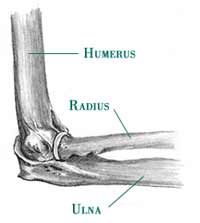
Clinically Relevant Anatomy[edit | edit source]
The elbow joint is made up of three bones: the humerus (upper arm bone), the radius and ulna (two bones in the forearm). At the distal end of the humerus there are two epicondyles, one lateral (on the outside) and one medial (on the inside).
Musculature involved is most commonly the extensor carpi radialis brevis (ECRB), but this injury can also involve the extensor carpi radialis longus (ECRL), extensor digitorum, and extensor carpi ulnaris.
The radial nerve is also in close proximity to this region, and divides into the superficial radial nerve and the posterior interosseous nerve.
Epidemiology /Etiology[edit | edit source]
Lateral epicondylitis is classified as an overuse injury. Overuse of the muscles and tendons of the forearm and elbow together with repetitive gripping or manual tasks can put too much strain on the elbow tendons. These gripping or manual tasks require manipulation of the hand that causes maladaptions in tendon structure that lead to pain over the lateral epicondyle. Mostly, the pain is located anterior and distal from the lateral epicondyle.
Epicondylitis occurs at least five times more often and predominantly occurs on the lateral rather than on the medial aspect of the joint, with a 4:1 to 7:1 ratio.
This injury is often work-related, any activity involving wrist extension, pronation or supination during manual labour, housework and hobbies are considered as important causal factors.
A systematic review identified 3 risk factors: handling tools heavier than 1 kg, handling loads heavier than 20 kg at least 10 times per day, and repetitive movements for more than 2 hours per day. [5]
Other risk factors are overuse, repetitive movements, training errors, misalignments, flexibility problems, aging, poor circulation, strength deficits or muscle imbalance and psychological factors.
There are several opinions concerning the cause of lateral epicondylitis:
Inflammation:
• Although the term epicondylitis implies the presence of an inflammatory condition, inflammation is present only in the earliest stages of the disease process. [6]
Microscopic tearing:
• Nirschl and Pettrone attributed the cause to microscopic tearing with formation of reparative tissue (angiofibroblastic hyperplasia) in the origin of the extensor carpi radialis brevis (ECRB) muscle. This micro-tearing and repair response can lead to macroscopic tearing and structural failure of the origin of the ECRB muscle.
• That microscopic or macroscopic tears of the common extensor origin were involved in the disease process, was postulated by Cyriax in 1936.
• The first to describe macroscopic tearing in association with the histological findings were Coonrad and Hooper.
• Histology of tissue samples shows "collagen disorientation, disorganization, and fibre separation by increased proteoglycan content, increased cellularity, neovascularization, with local necrosis." Nirschl termed these histological findings bangiofibroblastic hyperplasia. The term has since been modified to bangiofibroblastic tendinosis. He noted that the tissue was characterized by disorganized, immature collagen formation with immature fibroblastic and vascular elements. This grey, friable tissue is found in association with varying degrees of tearing involving the extensor carpi radialis brevis.
Degenerative process:
The histopathological features of 11 patients who had lateral epicondylitis were examined by Regan et al. They determined that the cause of lateral epicondylitis was more indicative of a degenerative process than an inflammatory process. The condition is degenerative with increased fibroblasts, vascular hyperplasia, proteoglycans and glycosaminoglycans, and disorganized and immature collagen. Repetitive eccentric or concentric overloading of the extensor muscle mass is thought to be the cause of this angiofibroblastic tendinosis of the ECRB.
Hypovascularity:
Because this tendinous region contains areas that are relatively hypovascular, the tendinous unit is unable to respond adequately to repetitive forces transmitted through the muscle, resulting in declining functional tolerance. [7]
Characteristics/Clinical Presentation[edit | edit source]
Lateral epicondylitis has an annual incidence of 1-3% within the general population. [8]
The difference between men and women on lateral epicondylitis is still controversial.
Patients with lateral epicondylitis are typically 35 to 54 years. It’s less common in people under 30 years. Symptoms last, on average, from 6 months to 2 years. 89% of the patients recover within 1 year without any treatment except perhaps avoidance of the painful movements. [8][9][10]
Patients often report weakness in their grip strength or difficulty carrying objects in their hand, especially with the elbow extended. They have complaints of pain just distal to and localized tenderness over the lateral epicondyle. Patients will commonly have pain with palpation of the lateral epicondyle, resisted wrist, or second or third finger extension (Cozen's sign). [11]
Differential Diagnosis
[edit | edit source]
Radial Tunnel Syndrome [12]
Posterior Interosseous Nerve (PIN) Syndrome
Elbow osteoarthritis
- Pain
- Loss of range of motion
Fractures
- Radiating arm pain corresponding to the dermatomes
- Neck pain
- Parasthesia
- Muscle weakness in myotome
- Reflex impairment/loss
- Headaches
- Scapular pain
- Sensory and motor dysfunction in upper extremities and neck
Diagnostic Procedures[edit | edit source]
The diagnosis of lateral epicondylitis is substantiated by tenderness over the ECRB or common extensor origin. By the following methods, the therapist or physiotherapist should be able to reproduce the typical pain:
1. Digital palpation on the facet of the lateral epicondyle
2. Resisted wrist extension or resisted middle-finger extension with the elbow in extension
3. Having the patient grip an object
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
mASES
QuickDASH (reliability= .90, MCID not reported)
PSFS (reliability= .82-.92, MCID=2.0)
PrTEEQ - Patient-Rated Tennis Elbow Evaluation Questionnaire (Pain ICC = 0.89-0.99, Function ICC = 0.83-0.99, Total ICC = 0.89-0.99)[13][14][15]
Examination[edit | edit source]
• To examine the sincerity of the tennis elbow, there is a dynamometer and a Patient-rated Tennis Elbow Evaluation Questionnaire (PrTEEQ).[16][17] The dynamometer measures grip strength.[18][19] The PrTEEQ is a 15-item questionnaire, it’s designed to measure forearm pain and disability in patients with lateral epicondylitis. The patients have to rate their levels of tennis elbow pain and disability from 0 to 10, and consists of 2 subscales. There is the pain subscale (0 = no pain, 10 = worst imaginable) en the function subscale (0 = no difficulty, 10 = unable to do).
• A positive sign is tenderness to palpation at the anterior epicondyle
• Cozen's sign:
The patient is positioned with the upper extremity relaxed. The examiner stabilizes the patient’s elbow with one hand and the patient is instructed to make a fist, pronate the forearm, and radially deviate the wrist. At last, the patient is instructed to extend the wrist against resistance that is provided by the examiner. An altenative is resisted extension of the middle finger that can cause pain at the extensor carpi radialis brevis origin. The test is positive if the patient experiences a sharp, sudden, severe pain over the lateral epicondyle.[20][21]
• Chair test: The patient grasps the back of the chair while standing behind it and attempts to raise it by putting their hands on the top of the chair back. Pain reproduction at the lateral epicondyle is a positive test.
• Mill's Test: The patient is positioned in standing with the upper extremity relaxed at side and the elbow extended. The examiner passively stretches the wrist in flexion and pronation. Pain at the lateral epicondyle or proximal musculotendinous junction of wrist extensors is positive for lateral epicondylitis.
• The coffee cup test (by Coonrad and Hooper) where picking up a full cup of coffee is painful.
Medical Management
[edit | edit source]
Medical management of lateral epicondylalgia has historically included NSAIDs, advice regarding rest, use of an elbow counterforce brace, and corticosteroid injection(s). Histologic research and the discovery of the true nature of this condition has led to more appropriate diagnosis and treatment in regard to the degeneration that is occurring at the site. Current medical treatment and research involves the use of interventions like prolotherapy, autologous blood injections, and even surgery (usually after failed conservative treatment for >6 mos)(Emedicine). Low level laser therapy has also been found to be an ineffective treatment modality for lateral epicondylalgia. [22]
Physical Therapy Management
[edit | edit source]
There are different types of therapies to treat lateral epicondylitis, all with the same aim: reduce pain and improve function. One of those is the Cyriax physiotherapy.
Cyriax physiotherapy
It’s a very common intervention that combines the use of deep transverse friction(DTF) with manipulations, which was used with success by Cyriax and Cyriax for treating lateral epicondylitis.
Contraindications: active infections, bursitis, disorders of the nerve structures, ossification and calcification of the soft tissues, active rheumatoid arthritis, anticoagulant.
Technics:
• DEEP TRANSVERSE FRICTION: Level of evidence: 1B
The therapist must try to reach an analgesic effect applying the DTF at the point of the lesion for 10 min till a numbing effect has been reached ,that all for preparing the tendon for the manipulations. Pain during the friction massage is considered as a wrong indication. An interval of 48 hours between two sessions is necessary.Level of evidence: 1B
The purpose of the deep friction massage is to maintain the mobility within the soft tissue structures.[34] It seems to have a pain relief function , due to modulation of the nociceptive impulses (gate control theory), a better alignment of connective tissue fibrils, softens the scar tissue, and blood flow increases, but further studies are needed.
Foto [30]
”Seated with arm fully supinated in 90° of elbow flexion, identify the area of tenderness on the lateral epicondyle and apply pressure(DTF) ,with the tip of the thumb on the lateral epicondyle, in a posterior direction on the teno-osseous junction. The other hand stabilized the patient’s wrist.”[30][31] Level of evidence: 1B
• MILL’S MOBILISATION: Level of evidence 1A
The commonly used Mill's manipulation, is a small-amplitude high-velocity thrust performed at the end of elbow extension while the wrist and hand are held flexed.[36] “ It’s used to pull apart the two edges of the tear and relieve tension on the painful scar lying between the edges, imitating the mechanism of spontaneous recovery. This motion allows the self-perpetrating post-traumatic inflammation to subside with permanent lengthening of the tendon. This approach was described by Mills.” [36]
Mill’s intention was to shift the annular ligament and replace it. Cyriax found out that the annular ligament applies the greatest possible stretching tension to the extensor carpi radialis muscles, that’s why the manipulative procedure should be carried out with a sharp jerk, in order to open the tear in the tendon and relieve tension on the tendon scar by converting a tear. [36]
This manipulation must only be performed if a fully pain-free elbow extension can be achieved, and with a properly technique. To prevent symptoms worsening, fully wrist flexion must be achieved during the procedure. [36]
Foto [33][37]
Patient seated with the affected extremity in 90° abduction and internal rotation (olecranon faced up).Therapist stands behind the patient , stabilized the patient’s wrist in full pronation and flexion, while the other hand is placed on the olecranon. The high-velocity low amplitude (HVLA) thrust at the end range of elbow extension, is a quick movement in the direction illustrated.
This manipulation may produce mild discomfort at the instant of its performance.
The clinician applies this procedure a 2-3 times a week until cure, with a range of 4-12 sessions. 30][31][33] Level of evidence:1 B
Evidence based
The study of Nagrale et all. demonstrate that Cyriax physiotherapy is a better treatment compared to phonophoresis and exercise for treating lateral epicondylalgia. The cyriax physiotherapy group had significantly better scores for all measurements at follow up (p<0.05). [31] Level of evidence: 1B
Rajadurai et all demonstrate that supervised exercise program may be the first treatment in managing tennis elbow in comparison to Cyriax physiotherapy. Much more studies should be done to prove the evidence of using manual treatment like Cyriax physiotherapy.[30]
Physical therapy interventions including elbow joint mobilization with movement combined with exercise has been shown to have better results than corticosteroid injection at 6 weeks and to wait and see at 6 weeks but not 52 weeks. Recent research regarding cervicothoracic joint mobilization in conjunction with local treatment for lateral epicondylalgia has shown improvements in strength, pain, and tolerance to activity compared to local treatment alone. [23]
Physical therapy management including only the use of ultrasound, massage, and exercise has been shown to be no better than a "wait and see" treatment method. [24] Activity modification, when possible, can help prevent recurrent episodes of lateral epicondylalgia, as well as use of a counterforce brace as needed.
- Stretching[25][26]The literature on the treatment of a Lateral Epicondylitis suggests that strengthening and stretching exercises are the most important components of exercise programmes, for the reason that tendons should not only be strong but
also flexible. The stretching exercises are intended to improve the flexibility of the extensor group of the wrist. These exercises ought to be instituted and continued until the range of motion of the wrist is the same as that of the uninvolved side.
These programmes should occur early in the treatment, to facilitate correct tissue remodelling. Early strength training should focus on low load and high-repetition training programmes, to prevent symptom aggravation.
The best stretching position for the Extensor Carpi Radialis Brevis tendon, is reached with the elbow in extension, forearm in pronation, wrist in flexion and with ulnar deviation of the wrist, according to the patient’s tolerance.
This stretching should be held for 30- 45 s and 3 times before and after the eccentric exercises, during each treatment session with a 30 s rest interval. - Eccentric exercisesThere are three principles of eccentric exercises. These are load ( resistance), speed (velocity) and frequency of contractions.There are three principles of eccentric exercises. These are load ( resistance), speed (velocity) and frequency of contractions. Load ( resistance)
Increasing the load ensures the tendon is subjected to greater stress and forms the fundamental basis of the progression of the exercise programme.
The basis of all physical training programmes is formed by this principle of progressive overloading.
According to the patient’s symptoms, it is important that the load of these eccentric exercises should be increased. If it’s not increased then the possibility of re-injury will be high. Speed ( velocity)
The speed (velocity) of contractions is also a fundamental principle of successful eccentric exercises. In each treatment session the speed of the eccentric training should be increased. Hence the load on the tendon increases to stimulate the mechanism of the injury.
However the therapists must ensure that the patients perform the eccentric exercises slowly to avoid pain. Frequency of contractions
The frequency of contractions is the third principle of eccentric exercises. There can be variations of sets and repetitions in the literature.
According to the therapists 3 sets of 10 repetitions can normally be performed without overloading the injured tendon, as determined by the tolerance of the patient. The elbow is in full extension, forearm in pronation and the arm is supported.
The greatest strengthening result for the extensor tendons of the wrist is reached in this position.
This is a recommendation and the frequency must be patient specific. - [27]Flexbar® exercise The Flexbar® is an effective and beneficial eccentric exercise for patients with lateral epicondylitis.
This resistance device is easy to use at home and is an excellent example of true “evidence-based practice” in physical therapy. Instructions for the 5 Steps of the Exercise:
A. Hold FlexBar® in the affected (right) hand. Make sure it's in full wrist extension..
B. The other end of the device must be held with your unaffected (left) hand.
C. Twist FlexBar® with unaffected wrist while holding. Demonstration of the exercise
The FlexBar® exercise is performed each day for 3 sets of 15. It takes 4 seconds to complete each repetition and between each set of 15 repetitions there is 30 seconds of rest. Once the patients can perform 3 sets of 15, they progress to another colour FlexBar® with a higher intensity of eccentric resistance. After an average of 7 weeks (with 10 clinic visits) the patient will have a resolution of symptoms. The treatment should be continued until this resolution occurs.
Key Research[edit | edit source]
Cyriax, Cyriax physiotherapy, Cyriax manipulation, Cyriax method, Cyriax orthopaedic medicine, manual therapy, orthopaedic medicine, James Cyriax,, cyriax technique, tennis elbow therapy, lateral epicondylalgia, therapy/treatment, manipulations tennis elbow
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
- Nirschl, RP, Pettrone FA, Tennis elbow and the surgical treatment of lateral epicondylitis. Journal of Bone and Joint Surgery. 61A:832, 1979.
- Wright JG. Evidence-based orthopaedics: the best answers to clinical questions. Philadelphia: Saunders Elsevier, 2008.
- Whaley AL, Baker CL. Lateral epicondylitis. Clin Sports Med 23 (2004) 677–691.
- Davenport TE, Kulig K, Matharu Y, Blanco CE. The EdUReP Model for Nonsurgical Management of Tendinopathy. Phys Ther. 2005;85(10):1093-103. http://ptjournal.apta.org/content/85/10/1093.long
- Sambrook P, Schrieber L, Taylor T, Ellis A. The musculoskeletal system. Churchill Livingstone, 2001
- Staples MP, Forbes A, Ptasznik R, Gordon J, Buchbinder R. A randomized controlled trial of extracorporeal shock wave therapy for lateral epicondylitis (tennis elbow). J Rheumatol. 2008;35(10):2038-46. A2 http://www.ncbi.nlm.nih.gov/pubmed/18792997 (accessed 17 Nov 2010)
- Rompe JD et al., Repetitive Low-Energy Shock Wave Treatment for Chronic Lateral Epicondylitis in Tennis Players, Am J Sports Med. 2004 Apr-May;32(3):734-43. A2 http://chroniccure.net/physicians/research/2004-03-11-AJSMRompe-Epicondylitis.pdf (accessed 1 Nov 2010)
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1XgES5aR9nB76Akn-f96Jur17dpvEooITsW2_CWVDashdJr11y|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
1. ↑ http://emedicine.medscape.com/article/1231903-overview (accessed 17 Nov 2010) Level of evidence: 2A
2. ↑ Nirschl RP, Ashman ES, Review Elbow tendinopathy: tennis elbow. Clin Sports Med. 2003 Oct; 22(4):813-36. (Level of Evidence 2A)
3. ↑ Stasinopoulos D, Johnson MI Med Hypotheses, 'Lateral elbow tendinopathy' is the most appropriate diagnostic term for the condition commonly referred-to as lateral epicondylitis. 2006; 67(6):1400-2. (Level of Evidence 3B)
4. ↑ 3. DeLee, Jesse, David Drez, and Mark D. Miller. DeLee &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Drez's Orthopaedic Sports Medicine Principles and Practice. St. Louis, MO: Elsevier Science, 2009, Volume II, chapter 19 forarm and elbow, tendinopathies around the elbow, lateral epicondylitis. (Level of Evidence 3A)
5. ↑ Van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford). May 2009;48(5):528-36. A1 http://rheumatology.oxfordjournals.org/content/48/5/528.full.pdf (accessed 17 Nov 2010)
6. ↑ Baker CL, Plancher KD. Operative treatment of elbow injuries. New York: Springer, 2002.
7. ↑ Davenport TE, Kulig K, Matharu Y, Blanco CE. The EdUReP Model for Nonsurgical Management of Tendinopathy. Phys Ther. 2005;85(10):1093-103. http://ptjournal.apta.org/content/85/10/1093.long Level of evidence: 5
8. ↑ 8.0 8.1 Wright JG. Evidence-based orthopaedics: the best answers to clinical questions. Philadelphia: Saunders Elsevier, 2008.
9. ↑ Cyriax JH. The pathology and treatment of tennis elbow. J Bone Joint Surg 1936; 18: 921–40. http://www.ejbjs.org/cgi/reprint/18/4/921.pdf (accessed 30 Dec 2010)
10. ↑ Smidt N, van der Windt D, Assendelft W, Devillé W, Korthals-de Bos I, Bouter L. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet 2002; 359: 657–62. A2 http://www.physio-pedia.com/images/9/9e/Smidt_et_al_RCT_lateral_elbow.pdf (accessed 30 Dec 2010) Level of evidence: 1A
11. ↑ Bisset L, Beller E, Jull E, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. BMJ 2006;doi:10.1136/bmj.38961.584653. B https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1633771/ (accessed 20 Nov 2010) ) Level of evidence: 1A
12. ↑ Roles NC, Maudsley RH. Radial tunnel syndrome: Resistant tennis elbow as nerve entrapment. J Bone Joint Surg Br 54:499-508, 1972. http://web.jbjs.org.uk/cgi/reprint/54-B/3/499 (accessed 20 Nov 2010) Level of evidence:2C
13. ↑ Leung HB, Yen CH, Tse PYT. Reliability of Hong Kong Chinese version of the Patient ratedfckLRForearm Evaluation Questionnaire for lateral epicondylitis. Hong Kong Med J 2004;10:172-7. Level of evidence:2B
14. ↑ Newcomer KL, Martinez-Silvestrini JA, Schaefer MP, Gay RE, Arendt KW. Sensitivity of the Patient-rated Forearm Evaluation Questionnaire in lateral epicondylitis. J Hand Ther 2005;18:400-6. Level of evidence: 2B
15. ↑ Overend TJ, Wuori-Fearn JL, Kramer JF, MacDermid JC. Reliability of a patient-rated forearm evaluation questionnaire for patients with lateral epicondylitis. J Hand Ther 1999;12:31-7. Level of evidence: 2B
16. ↑ Rompe JD, Overend TJ, MacDermid JC. Validation of the Patient-rated Tennis Elbow Evaluation Questionnaire. J Hand Ther. 2007 Jan-Mar;20(1):3-10. http://www.ncbi.nlm.nih.gov/pubmed/17254903 (accessed 30 Dec 2010) Level of evidence: 2B
17. ↑ MacDermid JC. The Patient-Rated Tennis Elbow Evaluation (PRTEE)© User Manual. 2007 http://www.srs-mcmaster.ca/Portals/20/pdf/research_resources/PRTE_UserManual_Dec2007.pdf (accessed 30 Dec 2010) Level of evidence: 2A
18. ↑ Mathiowetz V. Comparison of Rolyan and Jamar dynamometers for measuring grip strength. Occup Ther Int. 2002;9(3):201-9. Level of evidence: 2B
19. ↑ http://www.fysio-web.nl/Handheld_Dynamometer_1_2_11_jun.pdf (accessed 30 Dec 2010)
20. ↑ Cooper G. Pocket guide to musculoskeletal diagnosis. New Jersey: Humana Press, 2006 Level of evidence: 5
21. ↑ Bhargava AS, Eapen C, Kumar SP. Grip strength measurements at two different wrist extension positions in chronic lateral epicondylitis-comparison of involved vs. uninvolved side in athletes and non athletes: a case-control study. Sports Med Arthrosc Rehabil Ther Technol. 2010 Sep 7;2:22. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2944326/pdf/1758-2555-2-22.pdf (accessed 30 Dec 2010) . Level of evidence: 3B
22. ↑ Bjordal JM, Rodrigo AB Lopes-Martins, Joensen J, Couppe C, Ljunggren AE, Stegioulas A, Johnson MI. A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow). BMC Musc Dis. 2008;9:75,1471-2474 http://www.biomedcentral.com/1471-2474/9/75 Level of evidence: 1A
23. ↑ Cleland JA, Flynn TW, Palmer JA. Incorporation of manual therapy directed at the cervicothoracic spine in patients with lateral epicondylalgia: a pilot clinical trial. J Man and Manip Ther. 2005;13(3):143-151.
24. ↑ Smidt N, Van der Windt DAWM, Assendelft WJJ, Deville WLFM, Korthals-de Bos IBC, Bouter LM. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. LANCET. 2002;359:657-662. Level of evidence: 1B
25. ↑ Waseem M., et al, Lateral epicondylitis: A review of the Literature, 2012, J Back Musculoskelet Rehabil (Level of Evidence 2A)
26. ↑ Viswas R., et al. Comparison of Effectiveness of Supervised Exercise Program and Cyriax Physiotherapy in Patients with Tennis Elbow (Lateral Epicondylitis): A Randomized Clinical Trial, 2012, Scientific World Journal (Level of Evidence 1B)
27. ↑ Phil Page, et al, A new exercise for tennis elbow that works, 2010, North American Journal of Sports Physical Therapy. (Level of Evidence 2C)
28. ↑ 7. Vaisière, V., 2009-2010, Revue de littérature des traitements de l’épicondylite, Mémoire de master 2 à INSTITUT DES SCIENCES DE LA MOTRICITE. Université libre de Bruxelles, Bruxelles. (Level of Evidence 2A)
29. ↑D Stasinopoulos, M I Johnson, “Cyriax physiotherapy for tennis elbow/lateral epicondylitis”, Br J Sports Med 2004;38:675–677. doi: 10.1136/bjsm.2004.013573 Level of evidence: 2A
30. ↑Rajadurai Viswas,1 Rejeeshkumar Ramachandran,1 and Payal Korde Anantkumar2, “Comparison of Effectiveness of Supervised Exercise Program and Cyriax Physiotherapy in Patients with Tennis Elbow Lateral Epicondylitis): A Randomized Clinical Trial”, The ScientificWorld Journal Volume 2012, Article ID 939645, 8 pages doi:10.1100/2012/939645 Level of evidence: 1B
31. ↑Amit V. Nagrale, MPhT1; Christ opher R. Herd , PT, DPT, CSCS 2; Shyam Ganvir, MPhT3; Gopichand Ramteke, MPhT4,Cyriax Physiotherapy Versus Phonophoresis with Supervised Exercise in Subjects with LateralEpicondylalgia: A Randomized Clinical Trial, J Man Manip Ther. 2009; 17(3): 171-178 Level of evidence:1B
32. ↑L. Bisset1,2, N. Smidt3,4, D. A. Van der Windt5,6, L. M. Bouter5, G. Jull1, P. Brooks7 and B. Vicenzino1 Conservative treatments for tennis elbowdo subgroups of patients respond differently? Rheumatology 2007;46:1601-1605 Level of evicende: 1A
33. ↑SHIRLEY KUSHNER, BScPT, BPE,* DAVID C. REID, MD, MCh(Orth), FRCS(C)t, Manipulation in the Treatment of Tennis Elbow, 01 96-601 1 /86/0705-0264$02.00/0THE J OURNAOFL O RTHOPAEOA~NC0 SPORTPSH YSICATLH ERAPY Copyright O 1986 by The Orthopaedic and Sports Physical Therapy Sections of th American Physical Therapy Association Level of evidence:2A
34. ↑GAIL J. CHAMBERLAIN, MA, PT*, Cyriax's Friction Massage: A Review, 0196-601 1 /82/0401-0016$02.00/0 THE JOURNAL OF ORTHOPAEDIC AND SPORTSP HYSICALT HERAPY Copyright O 1982 by The Orthopaedic and Sports Physical Therapy Sections of the American Physical Therapy Association Level of evidence:2 A
35. ↑Christopher R. Herd, PT, DPT, CSCS1, Brent B. Meserve, DPT2, A Systematic Review of the Effectiveness of Manipulative Therapy in Treating Lateral Epicondylalgia, J Man Manip Ther. 2008;16(4):225-37. Level of evidence: 1A
36. ↑Bill Vicenzino, PT, PhD, Joshua A. Cleland, PT, PhD, OCS, FAAOMPT, and Leanne Bisset, PT, MPhty (Sports), Joint Manipulation in the Management of Lateral Epicondylalgia: A Clinical Commentary, J Man Manip Ther. 2007; 15(1): 50–56 Level of evidende:2A
37. ↑Franklin Schoenoltz, DC, DABCO Arcadia, California, Manipulative management of tennis elbow, ACA Journal of Chiropractic /June 1978 Level of evidence: 4
38. ↑Dr. Vijay Kage M.P.T, Dr. Sanjiv Kumar MPT,PM&IR,Ph.D,Comparison of Cyriax Physiotherapy and Taping Technique in subjects with tennis elbow: A Randomized Clinical Trial Reg.No LD0110001 KLE University Institute of Physioterapy Belgaum 2011-2012 Level of evidence: 1B
- ↑ http://emedicine.medscape.com/article/1231903-overview (accessed 17 Nov 2010)
- ↑ Nirschl RP, Ashman ES, Review Elbow tendinopathy: tennis elbow. Clin Sports Med. 2003 Oct; 22(4):813-36. (Level of Evidence 2A)
- ↑ Stasinopoulos D, Johnson MI Med Hypotheses, 'Lateral elbow tendinopathy' is the most appropriate diagnostic term for the condition commonly referred-to as lateral epicondylitis. 2006; 67(6):1400-2. (Level of Evidence 3B)
- ↑ 3. DeLee, Jesse, David Drez, and Mark D. Miller. DeLee &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Drez's Orthopaedic Sports Medicine Principles and Practice. St. Louis, MO: Elsevier Science, 2009, Volume II, chapter 19 forarm and elbow, tendinopathies around the elbow, lateral epicondylitis. (Level of Evidence 3A)
- ↑ Van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford). May 2009;48(5):528-36. A1 http://rheumatology.oxfordjournals.org/content/48/5/528.full.pdf (accessed 17 Nov 2010)
- ↑ Baker CL, Plancher KD. Operative treatment of elbow injuries. New York: Springer, 2002.
- ↑ Davenport TE, Kulig K, Matharu Y, Blanco CE. The EdUReP Model for Nonsurgical Management of Tendinopathy. Phys Ther. 2005;85(10):1093-103. http://ptjournal.apta.org/content/85/10/1093.long
- ↑ 8.0 8.1 Wright JG. Evidence-based orthopaedics: the best answers to clinical questions. Philadelphia: Saunders Elsevier, 2008.
- ↑ Cyriax JH. The pathology and treatment of tennis elbow. J Bone Joint Surg 1936; 18: 921–40. http://www.ejbjs.org/cgi/reprint/18/4/921.pdf (accessed 30 Dec 2010)
- ↑ Smidt N, van der Windt D, Assendelft W, Devillé W, Korthals-de Bos I, Bouter L. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet 2002; 359: 657–62. A2 http://www.physio-pedia.com/images/9/9e/Smidt_et_al_RCT_lateral_elbow.pdf (accessed 30 Dec 2010)
- ↑ Bisset L, Beller E, Jull E, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. BMJ 2006;doi:10.1136/bmj.38961.584653. B https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1633771/ (accessed 20 Nov 2010)
- ↑ Roles NC, Maudsley RH. Radial tunnel syndrome: Resistant tennis elbow as nerve entrapment. J Bone Joint Surg Br 54:499-508, 1972. http://web.jbjs.org.uk/cgi/reprint/54-B/3/499 (accessed 20 Nov 2010)
- ↑ Leung HB, Yen CH, Tse PYT. Reliability of Hong Kong Chinese version of the Patient ratedfckLRForearm Evaluation Questionnaire for lateral epicondylitis. Hong Kong Med J 2004;10:172-7.
- ↑ Newcomer KL, Martinez-Silvestrini JA, Schaefer MP, Gay RE, Arendt KW. Sensitivity of the Patient-rated Forearm Evaluation Questionnaire in lateral epicondylitis. J Hand Ther 2005;18:400-6.
- ↑ Overend TJ, Wuori-Fearn JL, Kramer JF, MacDermid JC. Reliability of a patient-rated forearm evaluation questionnaire for patients with lateral epicondylitis. J Hand Ther 1999;12:31-7.
- ↑ Rompe JD, Overend TJ, MacDermid JC. Validation of the Patient-rated Tennis Elbow Evaluation Questionnaire. J Hand Ther. 2007 Jan-Mar;20(1):3-10. http://www.ncbi.nlm.nih.gov/pubmed/17254903 (accessed 30 Dec 2010)
- ↑ MacDermid JC. The Patient-Rated Tennis Elbow Evaluation (PRTEE)© User Manual. 2007 http://www.srs-mcmaster.ca/Portals/20/pdf/research_resources/PRTE_UserManual_Dec2007.pdf (accessed 30 Dec 2010)
- ↑ Mathiowetz V. Comparison of Rolyan and Jamar dynamometers for measuring grip strength. Occup Ther Int. 2002;9(3):201-9.
- ↑ http://www.fysio-web.nl/Handheld_Dynamometer_1_2_11_jun.pdf (accessed 30 Dec 2010)
- ↑ Cooper G. Pocket guide to musculoskeletal diagnosis. New Jersey: Humana Press, 2006
- ↑ Bhargava AS, Eapen C, Kumar SP. Grip strength measurements at two different wrist extension positions in chronic lateral epicondylitis-comparison of involved vs. uninvolved side in athletes and non athletes: a case-control study. Sports Med Arthrosc Rehabil Ther Technol. 2010 Sep 7;2:22. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2944326/pdf/1758-2555-2-22.pdf (accessed 30 Dec 2010)
- ↑ Bjordal JM, Rodrigo AB Lopes-Martins, Joensen J, Couppe C, Ljunggren AE, Stegioulas A, Johnson MI. A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow). BMC Musc Dis. 2008;9:75,1471-2474 http://www.biomedcentral.com/1471-2474/9/75
- ↑ Cleland JA, Flynn TW, Palmer JA. Incorporation of manual therapy directed at the cervicothoracic spine in patients with lateral epicondylalgia: a pilot clinical trial. J Man and Manip Ther. 2005;13(3):143-151.
- ↑ Smidt N, Van der Windt DAWM, Assendelft WJJ, Deville WLFM, Korthals-de Bos IBC, Bouter LM. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. LANCET. 2002;359:657-662.
- ↑ Waseem M., et al, Lateral epicondylitis: A review of the Literature, 2012, J Back Musculoskelet Rehabil (Level of Evidence 2A)
- ↑ Viswas R., et al. Comparison of Effectiveness of Supervised Exercise Program and Cyriax Physiotherapy in Patients with Tennis Elbow (Lateral Epicondylitis): A Randomized Clinical Trial, 2012, Scientific World Journal (Level of Evidence 1B)
- ↑ Phil Page, et al, A new exercise for tennis elbow that works, 2010, North American Journal of Sports Physical Therapy. (Level of Evidence 2C)