Legg-Calve-Perthes Disease
Original Editor - Pamela Gonzalez, Bahire Evelyne
Lead Editors - Sarah Haerinck, Admin, Evelyne Bahire, Pamela Gonzalez, Lucinda hampton, Fien Wijnant, Samuel Adedigba, Lauren Kwant, Abbey Wright, Simisola Ajeyalemi, Kim Jackson, Rachael Lowe, Olajumoke Ogunleye, Benjamin Desmedt, 127.0.0.1, Rucha Gadgil, Wanda van Niekerk, Blessed Denzel Vhudzijena, Vidya Acharya, Eric Robertson, Meaghan Rieke, Jess Bell and Glenn Demeyer
Introduction[edit | edit source]
Legg-Calvé-Perthes disease (LCPD), refers to idiopathic osteonecrosis of the femoral epiphysis seen in children.
It is a diagnosis of exclusion and other causes of osteonecrosis (including sickle cell disease, leukaemia, corticosteroid administration, Gaucher disease) must be ruled out[1].
Etiology[edit | edit source]
The cause of LCPD is not known. It may be idiopathic or due to other etiology that would disrupt blood flow to the femoral epiphysis, eg trauma (macro or repetitive microtrauma), coagulopathy, and steroid use. Thrombophilia is present in approximately 50% of patients, and some form of coagulopathy is present in up to 75%[2].
Epidemiolgy[edit | edit source]
LCPD disease is relatively uncommon and in Western populations has an incidence approaching 5 to 15:100,000.
- Boys are five times more likely to be affected than girls.
- Presentation is typically at a younger age than slipped upper femoral epiphysis (SUFE) with peak presentation at 5-6 years, but confidence intervals are as wide as 2-14 years.[1]
Pathology[edit | edit source]
The specific cause of osteonecrosis in LPCD disease is unclear.
Fig.2: Summary of the pathogenesis of femoral head deformity following ischemic necrosis.
Osteonecrosis generally occurs secondary to the abnormal or damaged blood supply to the femoral epiphysis, leading to fragmentation, bone loss, and eventual structural collapse of the femoral head. In approximately 15% of cases, osteonecrosis occurs bilaterally[1].
Clinically Relevant Anatomy[edit | edit source]
The femoral head is supplied with blood from the medial circumflex femoral and lateral circumflex femoral arteries, which are branches of the profunda femoris artery.
- The medial femoral circumflex artery extends posteriorly and ascends proximally deep to the quadratus femorus muscle. At the level of the hip it joins an arterial ring at the base of the femoral neck.
- The lateral femoral circumflex artery extends anteriorly and gives off an ascending branch, which also joins the arterial ring at the base of the femoral neck.
This vascular ring gives rise to a group of vessels which run in the retinacular tissue inside the capsule to enter the femoral head at the base of the articular surface. There is also a small contribution from a small artery in the ligamentum teres to the top of the femoral head which is a branch of the posterior division of the obturator artery.
Staging[edit | edit source]
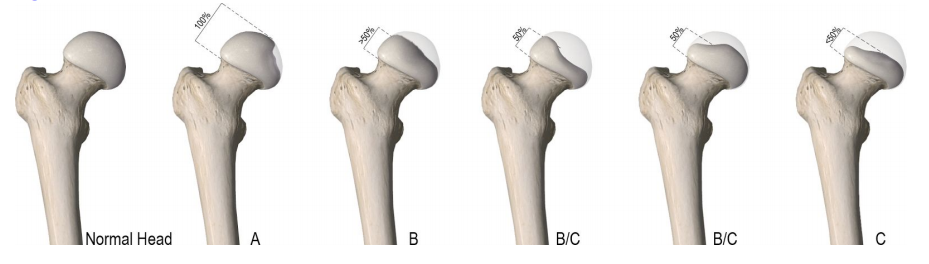
Multiple classifications can be utilized to describe Legg-Calve-Perthes disease. The lateral pillar, or Herring, classification is widely accepted with the best interobserver agreement. It is generally determined at the beginning of the fragmentation stage, approximately 6 months after initial symptom presentation. It cannot be used accurately if the patient has not entered the fragmentation stage
- Group A: The lateral pillar is at full height with no density changes. This group has a consistently good prognosis.
- Group B: The lateral pillar maintains greater than 50% height. There will be a poor outcome if the bone age is greater than 6.
- Group C: Less than 50% of the lateral pillar height is maintained. All patients will experience a poor outcome radiographically. The goal is to provide prognostic information. This classification is based on the height of the lateral pillar on the AP X-ray image.[2]
Fig.6: Modified Lateral Pillar Classification
Prognosis[edit | edit source]
According to a research article in the Journal of Bone and Joint Surgery, the strongest predictor of prognosis is the revised lateral pillar classification. Regardless of treatment strategy all group A hips and an overwhelming majority of group B hips have favourable results. The B/C border group has moderate results and all group C hips have poor results. The second strongest predictor of outcome is age at the onset of the disease.[4] An age of six years or less at the onset of the disease is usually, but not always, associated with a benign course and a good outcome.[5] Children between the ages of six and eight years at the onset of the disease are considered to have a variable prognosis and are thought to benefit from treatment. Patients who are eight years or older at the time of onset generally have poorer outcomes, albeit a better outcome with surgical treatment than they do with non-operative treatment.[4]
In other studies, good prognosis of a child with this disease under the age of eight has been shown to be up to 80%. This is with minimal treatment given to the patient. In this study, children between the ages of 4 and 5 and 11 months had a less favourable chance of a good outcome.
Characteristics/Clinical Presentation[edit | edit source]
LCPD is present in children 2-13 years of age and there is a four times greater incidence in males compared to females. The average age of occurrence is six years.
- Limp: A psoatic limp is typically present in these children secondary to weakness of the psoas major. The limp:[6] is worse after physical activities and improves following periods of rest. The limp becomes more noticeable late in the day, after prolonged walking.
- Pain: [6] The child is often in pain during the acute stages [7]. The pain is usually worse late in the day and with greater activity.[6] Night pains are frequent.[6]
- ROM: The child will show a decrease in extension and abduction active ranges of motion. There is also a limited internal rotation in both flexion and extension in the early phase of the disease [8].
- Unusual high activity level: [9] Children with LCPD are usually physically very active, and a significant percentage has true hyperactivity or attention deficit disorder.
- Abnormal growth patterns: [10] General pattern: The forearms and hands are relatively short compared to the upper arm. [11] The feet are relatively short compared to the tibia. [11]
Differential Diagnosis[edit | edit source]
Listed are some other disorders that should be included in the differential diagnosis for LCPD: All diseases which induce necrosis of the head or those resembling them are questioned in a differential diagnosis[12] :
- Septic arthritis or infectious arthritis: this is an infection of the joint.
- Sickle cell-Osteonecrosis of the hip can be a result of this disease
- Spondyloepiphyseal Dysplasia Tarda: this disease typically affects the spine and the larger more proximal joints
- Gaucher Disease: An autosomal recessive inherited genetic disorder of metabolism in which a dangerous level of a fatty substance called glucocerebroside collects in the liver, spleen, bone marrow, lungs, and at times in the brain
- Transient Synovitis of the hip is a self-limiting condition in which there is an inflammation of the inner lining (the synovium) of the capsule of the hip joint.
- Hip Labral Disorders: The hip labrum is a dense fibrocartilagenous structure, mostly composed of type 1 collagen that is typically between 2-3mm thick that outlines the acetabular socket and attaches to the bony rim of the acetabulum. Hip labral disorders are pathologies of this structure.
- Chondroblastoma: Chondroblastoma refers to a benign bony tumour that is caused by the rapid division of chondroblast cells which are found in the epiphysis of long bones. They have been described as calcified chondromatous giant cell tumours. [13]
- Juvenile Rheumatoid Arthritis : a chronic inflammatory disorder that occurs before the age 16 and can occur in all races.
- Multiple epiphyseal dysplasia - This is a disorder of cartilage and bone development primarily affecting the ends of the long bones in the arms and legs. [14]
Diagnostic Procedures[edit | edit source]
A MRI is usually obtained to confirm the diagnosis; however x-rays can also be of use to determine femoral head positioning.
Since LCPD has a variable end result, an imaging modality that can predict outcome at the initial stage of the disease before significant deformity has occurred is ideal.
The extent of femoral head involvement depicted by non-contrast and contrast MRI showed no correlation at the initial stage of LCPD, indicating that they are assessing two different components of the disease process. In the initial stage of LCPD, contrast MRI provided a clearer depiction of the area of involvement. [15]
To quantify femoral head deformity in patients with LCPD novel three dimensional (3D) magnetic resonance imaging (MRI) reconstruction and volume based analysis can be used. The 3D MRI volume ratio method allows accurate quantification and demonstrated small changes (less than 10 percent) of the femoral head deformity in LCPD. This method may serve as a useful tool to evaluate the effects of treatment on femoral head shape.[16]
Outcome Measures[edit | edit source]
The questionnaires below can be used to assess the initial function of a person and progress and outcome of operative as well as non-operative treatments. The surveys test the patient on a functional level are useful to provide a baseline and monitor functional progress in the patient’s activities.
- Harris Hip ScoreThe total score reliability was excellent for physicians (r = 0.94) and physiotherapists (r = 0.95). The physiotherapist and the orthopaedic surgeon showed excellent test–retest reliability in the domains of pain (r = 0.93 and r = 0.98, respectively) and function (r = 0.95 and r = 0.93, respectively). The calculations were done with Pearson's and Spearman's correlation coefficients. The inter-rater correlations were good to excellent (0.74–1.0)[17]
- Hip Disability and Osteoarthritis Outcome Score (HOOS). The HOOS is suggested to be valuable for younger and more active people due to the subscales. [18][19]
As for the difference in outcome for non-operative and operative treatments, a meta-analysis performed in 2012 suggests that operative treatment is more likely to yield a spherical congruent femoral head than non-operative methods among six-year-olds or older. For patients who are younger than the age of six, operative and non-operative methods have the same likelihood to yield a good outcome. Children who were six years or older who were treated operatively had the same likelihood of a good radiographic outcome regardless of surgical intervention with a femoral or pelvic procedure. Patients younger than six had a greater benefit from pelvic procedures than femoral procedures.[20]
Examination[edit | edit source]
Gait[edit | edit source]
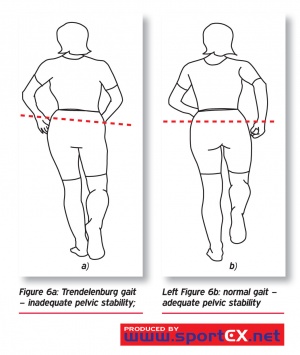
Is usually antalgic.[6] It is possible that the child has a Trendelenburg gait (a positive Trendelenburg sign on the affected side)[21]x
The child can also have a Duchenne gait, which is marked by a trunk lean toward the stance limb with the pelvis level or elevated on the unloaded side. [21]
There is insufficient evidence and lack of reliability and validity to support use of the observational gait assessment tools with this population. [23]
Range of movement[edit | edit source]
The restriction of hip motion is variable in the early stages of the disease. Many patients, may only have a minimal loss of motion at the extremes of internal rotation and abduction. At this stage there usually is no flexion contracture. Loss of hip ROM in patients with early LCPD without intra-articular incongruity is due to pain and muscle spasm. [24] This is why, if the child is examined for instance after a night of bed rest, the range will be much better then later in the day.
Further into the disease process, children with mild disease may maintain a minimal loss of motion at the extremes only and thereafter regain full mobility. Those with more severe disease will progressively lose motion, in particular abduction and internal rotation. Late cases may have adduction contractures and very limited rotation, but the range of flexion and extension is only seldom compromised.
Pain[edit | edit source]
Pain occurs during the acute disease.[7] The pain may be located in the groin, anterior hip area, or around the greater trochanter. Referral of pain to the knee is common.
It’s recommended that pain is assessed using the Numerical Rating Scale (NRS)[23].
Atrophy[edit | edit source]
In most cases there is atrophy of the gluteus, quadriceps[25] and hamstring muscles, depending upon the severity and duration of the disorder.
Medical Management[edit | edit source]
The approach to treatment is controversial. Prior to evaluating if a surgical intervention is necessary, there has to be a clear understanding of the disease prognosis.
Approaches to treatment can be divided in conservative or operative treatments.
Medications include non-steroidal anti-inflammatories (NSAIDs) for pain and/or inflammation.
Psychological factors are also considered. Persons with a history of LCPD are 1.5 times more likely to develop attention deficit disorders compared to their peers. They also have a higher risk of developing depression.[26]
Physical Therapy Management[edit | edit source]
There is no consensus concerning the possible benefits of physiotherapy in LCPD, or in which phase of the development of the health problem it should be used.
Some studies mention physiotherapy as a pre- and/or postoperative intervention, while others consider it a form of conservative treatment associated with other treatments, such as skeletal traction, orthesis, and plaster cast.
In studies comparing different treatments[27], physiotherapy was applied in children with a mild course of the disease. The characteristics of the patients were:
- Children with less than 50% femoral head necrosis (Catterall groups 1 or 2) [27]
- Children with more than 50% femoral head necrosis, under six years, whose femoral head cover is good (>80%)[27]
- Herring type A or B[28]
- Salter Thompson type A[28]
For patients with a mild course, physiotherapy can produce improvement in articular range of motion, muscular strength and articular dysfunction[28]. The physiotherapeutic treatment included:
- Passive mobilisations for musculature stretching of the involved hip.
- Straight leg raise exercises, to strengthen the musculature of the hip involved for the flexion, extension, abduction, and adduction of muscles of the hip.
- They started with isometric exercises and after eight session, isotonic exercises.
- A balance training initially on stable terrain, and later on unstable terrain.
For children over 6 years at diagnosis with more than 50% of femoral head necrosis, proximal femoral varus osteotomy gave a significantly better outcome than orthosis and physiotherapy[27].
There is an evidence-based care guideline concerning post-operative management of LCPD in children for age 3 to 12 and an evidence-based care guideline for conservative management of LCPD in children age 3 to 12. These studies are mostly based on ‘local consensus’ of the members of the LCPD team from Cincinnati Children’s Hospital Medical Center. These guidelines express the evidence regarding physical therapy (PT) treatment pathways, post-operatively and conservative management (see appendix 3 about evidence levels) [23]. The following recommendations are made:
Conservative management[edit | edit source]
Physical therapy interventions have been shown to improve ROM and strength in this patient population (3).
Individuals who participate in supervised clinic visits demonstrate greater improvement in muscle strength, functional mobility, gait speed, and quality of exercise performance than those who receive a home exercise program alone or no instruction at all (2).
Individuals who receive regular positive feedback from a physical therapist are more likely to be compliant with a supplemental home exercise program. (4)
It is recommended that supervised physical therapy is supplemented with a customized written home exercise program in all phases of rehabilitation. (2)
Improve ROM: (see appendix 1 for exercise prescription)
- Static stretch for lower extremity musculature (2)
- Dynamic ROM (2)
- Perform AROM and AAROM (active assistive range of motion) following passive stretching to maintain newly gained ROM (2)
Improve strength: (see appendix 2 for exercise prescription)
- Begin with isometric exercise and progress to isotonic exercises in a gravity lessened position with further progression to isotonic exercises against gravity. It is appropriate to include concentric and eccentric contractions (3).
- Begin with 2 sets of 10 to 15 repetitions of each exercise (2), with progression to 3 sets of each exercise to be used (2)
- Local consensus would also do exercises to improve balance and gait and interventions to reduce pain.[23]
The hip overloading pattern should be avoided in children with LCPD. Gait training to unload the hip might become an integral component of conservative treatment in children with LCPD. [29]
Non-surgical treatment with a brace is a reliable alternative to surgical treatment in LCPD between 6 and 8 years of age at onset with Herring B involvement. However, they could not know whether the good results were influenced by the brace or stemmed from having good prognosis of these patients. [30]
Post-operative management[edit | edit source]
The rehabilitation is described with reference to the various stages of rehabilitation.
- Initial Phase (0-2 weeks post-cast removal)
Goals of the Initial Phase
- Minimize pain
- Hot pack for relaxation and pain management with stretching (2)
- Cryotherapy (5)
- Medication for pain (5)
- Optimize ROM of hip, knee and ankle (see appendix 1 for exercises)
- Passive static stretch (2) (A hot pack may be used, based on patient preference and comfort (2))
- Dynamic ROM (2)
- Perform AROM and AAROM following passive stretching to maintain newly gained ROM (2)
- Increase strength for hip flexion, abduction, and extension and knee and ankle (see appendix 2 for exercises)
- Begin with isometric exercises at the hip and progress to isotonic exercises in a gravity lessened position (3)
- Begin with isometric exercises at the knee and ankle, progressing to isotonic exercises in a gravity lessened position with further progression to isotonic exercises against gravity (3)
- Begin with 2 sets of 10 to 15 repetitions of each exercise with progression to 3 sets of each exercise to be used (2)
- Improve gait and functional mobility
- Follow the referring physician’s guidelines for WB status (5)
- Transfer training and bed mobility to maximize independence with ADL’s (5)
- Gait training with the appropriate assistive device, focusing on safety and independence (5).
- Improving skin integrity
- Scar massage and desensitization to minimize adhesions (5)
- Warm bath to improve skin integrity following cast removal, if feasible in the home environment (5)
- Warm whirlpool may be utilized if the patient is unable to safely utilize a warm bath for skin integrity management (5)
PT is supervised at a frequency of 2-3 time per week (weekly) (5)
- Intermediate Phase (2-6 weeks post-cast removal)
Goals of the Intermediate Phase
- Minimize pain (see ‘initial phase’)
- Normalize ROM of the knee and ankle and optimize ROM of hip in all directions
- See ‘initial phase’ and see appendix 1 for exercises
- Increase strength of the knee and hip (see appendix 2 for exercises)
- Isotonic exercises of the hip in gravity lessened positions and advancing to against gravity positions (3)
- Isotonic exercises of the knee and ankle in gravity lessened and against gravity positions (3)
- Maintain independence with functional mobility maintaining WB status and use of appropriate assistive devices (5)
- Improving gait and functional mobility (5)
- Follow the referring physician’s guidelines for WB status (5)
- Continue gait training with the appropriate assistive device focusing on safety and independence (5)
- Begin slow walking in chest deep pool water with arms submerged (5)
- Improving Skin Integrity
- Continue with scar massage and desensitization (5)
PT is supervised at a frequency of 2-3 time per week (weekly) (5)
It is recommended that activities outside of PT are restricted at this time due to WB status. If the referring physician allows, swimming is permitted (5)
- Advanced Phase (6-12 weeks post-cast removal)
Goals
- Minimize pain (see ‘initial phase’)
- optimize ROM and flexibility of the hip, knee, and ankle
- see ‘initial phase’ and see appendix 1 for exercises
- Increase strength of the knee and hip, except for hip abductors, to at least 70% of the uninvolved lower extremity and increase strength of the hip abductors to at least 60% of the uninvolved lower extremity due to mechanical disadvantage (4 + 5) (see appendix 2 for exercises)
- Isotonic exercises of the hip, knee, and ankle in gravity lessened and against gravity positions, including concentric and eccentric contractions (3)
- WB and non-weight bearing (NWB) activities can be used in combination based on the patient’s ability (4) and goals of the treatment session (5)
- Begin upper extremity supported functional dynamic single limb activities (e.g. step ups, side steps) (5)
- Continue with double limb closed chain exercises with resistance, progressing to single limb closed chain exercises with light resistance if WB status allows (5)
- Use of a stationary bike in an upright or recumbent position keeping the hip in less than 90 degrees of flexion (5)
- Ambulation without use of an assistive device or pain (5)
- Negotiate stairs independently using step to pattern with upper extremity (UE) support (5)
- Improve balance to greater than 69% of the maximum Pediatric Balance Score (39/56) or single limb stance of the uninvolved side (5)
- Improving gait and functional mobility (5)
PT is supervised at a frequency of 1-2 time per week (weekly) (5)
It is recommended that activities outside of PT are limited to swimming if the referring physician allows (5).
Note: Running and jumping activities are restricted at this time (5).
- Pre-Functional Phase (12 weeks to 1+ year post-cast removal)
Goals
- Minimize pain (see ‘initial phase’)
- Optimize ROM and flexibility of the hip, knee, and ankle
- Static stretch (2)
- Increase strength of the knee and hip, except for hip abductors, to at least 80% of the uninvolved lower extremity and increase strength of the hip abductors to at least 75% of the uninvolved lower extremity due to mechanical disadvantage (4 + 5)
- see ‘advanced phase’ and see appendix 1 for exercises
- Negotiate stairs independently with reciprocal pattern an upper extremity support (5)
- Improve balance to 80% or greater of the maximum Pediatric Balance Score (at least 45/56) or single limb stance of the uninvolved side (5)
- Non-painful gait pattern with minimal deficits and normal efficiency (5)
PT is supervised at a frequency of 1-2 time per week (weekly) (5)
It is recommended that activities outside of PT include swimming and bike riding as guided by the referring physician (5).
Note: Running and jumping activities are restricted at this time (5).
- Functional phase
Goals
- Reduce pain to 1/10 or less (see ‘initial phase’)
- Normalizing ROM: Increase ROM to 90% or greater of the uninvolved side for the hip, knee, and ankle, except for hip abduction (5) and Increase hip abduction ROM to 80% or greater due to potential bony block (4)
- Static stretch (2)
- Normalizing strength: Increase strength of the knee and hip, except for hip abductors, to 90% or greater of the uninvolved lower extremity (5) and Increase strength of the hip abductors to at least 85% of the uninvolved lower extremity due to mechanical disadvantage (4+5)
- Progress isotonic exercises of the hip, knee, and ankle and include concentric and eccentric contractions (3).
- WB and NWB activities used in combination based on the patient’s ability (4) and goals of the treatment session.
- Functional dynamic single limb activities (e.g. step ups, side steps) with upper extremity support as needed for patient safety (5)
- Progress single leg closed chain exercises with resistance (4)
- Use of a stationary bike in an upright or recumbent position keeping the hip in less than 90 degrees of flexion
- Ambulation with a non-painful limp and normal efficiency (5)
- Negotiation of stairs independently using a reciprocal pattern without UE support (5)
- Improve balance to 90% or greater of the maximum score on the Pediatric Balance Scale (at least 51/56) or single limb stance of the uninvolved side (5) It is recommended that progression to the Functional Phase occur when the physician has determined there is sufficient re-ossification of the femoral head based on radiographs (5). Note: Jumping and other impact activities are still limited and only progressed per instruction from the physician based on healing and progression of the disease process (5). [31]
Appendices[edit | edit source]
Appendix 1: ROM exercise prescription
| Intervention | Parameters | Intensity | Notes | Muscle groups |
|---|---|---|---|---|
| Passive static stretch | 2 minutes of stretching per day, per muscle group (2)
30 second hold time, doing 4 repetitions per muscle group (2) |
Gentle static hold
Within patient pain tolerance and without muscle guarding so as to prevent tissue damage and inflammatory response (2) |
This is the preferred method of stretching to gain flexibility and/or ROM (2)
Stretching to be done after warm up, but prior to active exercises to maintain newly gained ROM (2) |
· Hip adductors
· Hip internal rotators · Hip external rotators · Hip flexors (5) |
| Dynamic ROM | 5 second hold, done with 24 repetitions per muscle group per day to meet 2 minute stretching time required (2) | Self-selected intensity by patient as long as not causing pain (5) | Done with patient activation of antagonistic muscle group (2)
Done with slow movement to end range for full benefit (2) |
· Hip adductors
· Hip internal rotators · Hip external rotators · Hip flexors (5) |
Appendix 2: Strengthening exercise prescription
| Intervention | Parameters | Intensity | Notes | Muscle groups |
|---|---|---|---|---|
| Isometric strengthening | 10 seconds hold with 10 repetitions per muscle, for total of 100 seconds (5) | Performed at approximately 75% maximal contraction (5) | Performed with hip in neutral position (5) | Hip adductors
· Hip internal rotators · Hip external rotators · Hip flexors · Hip extensors (4) |
| Isotonic strengthening | Hing repetitions (10-15 reps) and 2 to 3 sets (2)
Perform both concentric and eccentric contractions |
Low resistance (2) | Hip adductors
· Hip internal rotators · Hip external rotators · Hip flexors · Hip extensors (4) |
Table with levels of evidence of the guideline[23][31]
Appendix 3: Guide to levels of evidence referenced in guidelines
| Evidence level | Description |
|---|---|
| 1 | Systematic review, meta-analysis, or metasynthesis of multiple studies |
| 2 | Best study design for domain |
| 3 | Fair study design for domain |
| 4 | Weak study design for domain |
| 5 | Local Consensus Other: General review, , case report, consensus report, or guideline |
Key Research[edit | edit source]
In August 2016 researchers from the Universities of Liverpool and Manchester have been awarded £278k to help investigate the best surgical treatments for hip diseases in childhood. It will focus on people with two common hip diseases, LCPD and Slipped Capital Femoral Epiphysis (SCFE). Using measurements of the hip and clinical symptoms the researchers will develop methods to predict likely outcomes of the disease, and to choose the most appropriate treatment.[32]
Resources[edit | edit source]
- Books: John Anthony Herring, MD, editors. Legg-Calvé-Perthes Disease. Rosemont; American Academy of Orthopaedic Surgeons; 1996 p. 6-16
Clinical Bottom Line[edit | edit source]
Legg-Calve-Perthes Disease is an idiopathic juvenile avascular necrosis resulting in malformation of the femoral head. It’s a self healing condition and the long term outcome and therapy strongly depends on the severity of the osteonecrosis and the ultimate shape of the femoral head. Although more prevalent amongst males, females generally have worse outcome as well as do older children compared to younger ones.
There is next to no empirical evidence due to a lack of experimental research and the therapies prescribed are mostly based on heuristic models.
Treatments generally attempt to maintain and improve range of motion and strength as well as manage pain.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Radiopedia Perthes Disease Available: https://radiopaedia.org/articles/perthes-disease (accessed 15.10.2021)
- ↑ 2.0 2.1 Mills S, Burroughs KE. Legg Calve Perthes Disease. StatPearls [Internet]. 2020 Jul 13.Available:https://www.statpearls.com/articlelibrary/viewarticle/24174/ (accessed 15.10.2021)
- ↑ Ilesanmi OO. Pathological basis of symptoms and crises in sickle cell disorder: implications for counselling and psychotherapy. Hematol Rep 2010 26; 2(1): e2. doi: [10.4081/hr.2010.e2]
- ↑ 4.0 4.1 Herring JA, Kim HT, Browne R. Legg-Calvé-Perthes Disease Part II: Prospective Multicenter Study of the Effect of Treatment on Outcome. J Bone Joint Surg Am 2004;86:2121-2134
- ↑ Rosenfeld SB, Herring JA, Chao JC. Legg-Calvé-Perthes Disease: A Review of Cases with Onset Before Six Years of Age. J Bone Joint Surg Am 2007;89:2712-2722
- ↑ 6.0 6.1 6.2 6.3 6.4 Herring JA, editor. Legg-Calvé-Perthes Disease. 1st edition. Rosemont: American Academy of Orthopaedic Surgeons, 1996 p.6-16
- ↑ 7.0 7.1 Lynn T. Staheli. Practice of Pediatric Orthopedics. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 2006 p.182-183
- ↑ Wenger DR Ward WT, Herring JA. Current concepts review: Legg-Calvé-Perthes Disease. J Bone Joint Surg 1991;73:778-788
- ↑ Loder RT, Schwartz EM, Hensinger RN. Behavioral characteristics of children with Legg-Calve-Perthes Disease. J Pediatr Orthoped 1993;13(5):676-700
- ↑ Burwell RG. Perthes' disease: growth and aetiology. Arch Dis Child 1988;63(11):1408-1412
- ↑ 11.0 11.1 Burwell RG, Dangerfield PH, Hall DJ, Vernon CL, Harrison MHM. Perthes' disease. An anthropometric study revealing impaired and disproportionate growth. J Bone Joint Surg [Br] 1978;60-B(4):461-477
- ↑ Manig, M. Legg-Calvé-Perthes disease (LCPD). Principles of diagnosis and treatment. Orthopäde 2013;42(10):891-90
- ↑ Bain LG, Sun QF, Zhao WG, Shen JK, Tirakotai W, Bertalanffy H. Temporal bone chondroblastoma: A review. Neuropathology 2005;25:159–164
- ↑ Hunter JB. (iv) Legg Calvé Perthes’ disease. Curr Orthopaed 2004;18(4):273-83.
- ↑ Kim, HK, Kaste, S, Dempsey M, Wilkes D. A comparison of non-contrast and contrast-enhanced MRI in the initial stage of Legg-Calvé-Perthes disease. Pediatr Radiol 2013;43:1166. doi:10.1007/s00247-013-2664-7
- ↑ Standefer KD, Dempsey M, Jo C, Kim HKW. 3D MRI quantification of femoral head deformity in Legg‐Calvé‐Perthes disease." J Orthop Res 2016;35(9):2051-2058
- ↑ Kirmit L, Karatosun V, Unver B, Bakirhan S, Sen A, Gocen Z. The reliability of hip scoring systems for total hip arthroplasty candidates: assessment by physical therapists. Clin Rehabil 2005;19(6):659-661
- ↑ Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther 1999;79:371-383.
- ↑ Nilsdotter A, Bremander A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res 2011;63:S200-S207. doi:10.1002/acr.20549
- ↑ Nguyen NA, Klein G, Dogbey G, McCourt JB, Mehlman CT. Operative versus nonoperative treatments for Legg-Calvé-Perthes disease: a meta-analysis. J Pediatr Orthop. 2012;32(7):697-705. doi:10.1097/BPO.0b013e318269c55d.
- ↑ 21.0 21.1 Westhoff B, Petermann A, Hirsch MA, Willers R, Krauspe R. Computerized gait analysis in Legg Calve Perthes disease - Analysis of the frontal plane. Gait Posture October 2006;24(2):196-202
- ↑ Sallam A, Ziegler CM, Jansson V, Heimkes B. The underused hip in ipsilaterally orthotics-dependent children."J child orthop 2015;9(4):255-262.
- ↑ 23.0 23.1 23.2 23.3 23.4 Cincinnati Children's Hospital Medical Center. Evidence-based clinical care guideline for Conservative Management of Legg-Calve-Perthes Disease. Guideline 39. 2011. Available from: https://www.cincinnatichildrens.org/-/media/cincinnati%20childrens/home/service/j/anderson-center/evidence-based-care/recommendations/type/legg-calve-perthes%20disease%20guideline%2039
- ↑ Stanitski CL. Hip range of motion in Perthes’ disease: comparison of pre-operative and intra-operative values. J Child Orthop March 2007;1(1):33-35
- ↑ Robben SG, Lequin MH, Meradji M, Diepstraten AF, Hop WC. Atrophy of the quadriceps muscle in children with a painful hip. Clin Physiol. 1999 Oct;19(5):385-93.
- ↑ Hailer YD, Nilsson O. Legg-Calvé-Perthes disease and the risk of ADHD, depression, and mortality: A registry study involving 4057 individuals. Acta orthop. 2014;85(5):501-5.
- ↑ 27.0 27.1 27.2 27.3 Wiig O, Terjesen T, Svenningsen S. Prognostic factors and outcome of treatment in Perthes’ disease. J Bone Joint Surg 2008;90-B(10):1364-1371
- ↑ 28.0 28.1 28.2 Brecht GC, Guarnieiro R. Evaluation of physiotherapy in the treatment of Legg-Calvé-Perthes disaese. Clinics (Sao Paolo) 2006;61(6):521-528
- ↑ Švehlík M, Kraus T, Steinwender G, Zwick EB, Linhart WE. Pathological gait in children with Legg-Calvé-Perthes disease and proposal for gait modification to decrease the hip joint loading. Int Orthop 2012;36(6):1235-1241
- ↑ Cıtlak A, Kerimoğlu S, Baki C, Aydın H. Comparison between conservative and surgical treatment in Perthes disease. Arch Orthop Trauma Surg. 2012;132(1):87-92
- ↑ 31.0 31.1 Cincinnati Children's Hospital Medical Center: Evidence-based clinical care guideline for Post-Operative Management of Legg-Calve-Perthes Disease in children aged 3 to 12 years. Guideline 41. 2013. Available from: https://www.cincinnatichildrens.org/-/media/cincinnati%20childrens/home/service/j/anderson-center/evidence-based-care/recommendations/type/legg-calve-perthes%20disease%20guideline%2041(2)
- ↑ University of Liverpool. Researchers develop tool to treat child hip diseases. 2016. Available from:https://news.liverpool.ac.uk/2016/08/17/researchers-develop-tool-to-treat-child-hip-diseases/
![[3]](/images/thumb/0/02/Femoral_arteries.jpg/291px-Femoral_arteries.jpg)