Lumbar Spondylosis: Difference between revisions
Claire Knott (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) (Prepare Pages for Merging) |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Dries Meeusen|Dries Meeusen]], [[User:Robin Petroons|Robin Petroons]], [[User:Matthias Proost|Matthias Proost]], [[User:Kevin Ruelens|Kevin Ruelens]] and [[User:Marie Avau|Marie Avau]] Debby Decock, Farrie Bakalli, Laure-Anne Callewaert '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}<br> | |||
'''Page Owner''' - [[User:Nawal Farooq|Nawal Farooq]] as part of the [[One Page Project|One Page Project]]</div> | |||
== Definition/Description == | |||
[[File:Lumbar spondylosis2.JPG|right|frameless|400x400px]] | |||
< | Spondylosis may be applied nonspecifically to any and all degenerative conditions affecting the disks, vertebral bodies, and/or associated joints of the lumbar spine<ref name=":4">Middleton K, Fish DE. [https://link.springer.com/article/10.1007/s12178-009-9051-x Lumbar spondylosis: clinical presentation and treatment approaches.] Current Reviews in Musculoskeletal Medicine. 2009 Jun 1;2(2):94-104. Available from:https://link.springer.com/article/10.1007/s12178-009-9051-x (last accessed 8.9.2020)</ref>.<ref name=":0">Middleton, Kimberley, and David E. Fish. “Lumbar Spondylosis: Clinical Presentation and Treatment Approaches.” Current Reviews in Musculoskeletal Medicine 2, no. 2 (March 25, 2009): 94–104. | ||
== | </ref> | ||
* Low back pain (LBP) affects approximately 60–85% of adults during some point in their lives. | |||
Spondylosis | |||
* Not a clinical diagnosis but instead a descriptive term utilized to designate spinal problems. | |||
* Encompasses numerous associated pathologies including spinal stenosis, degenerative spondylolisthesis, osteoarthritis, ageing, trauma and just the daily use of the intervertebral discs, the vertebrae, and the associated joints.<ref>Gibson, J. N. Alastair, and Gordon Waddell. “Surgery for Degenerative Lumbar Spondylosis: Updated Cochrane Review.” Spine 30, no. 20 (October 15, 2005): 2312–20. | |||
</ref> | |||
* The lumbar region the most affected, because of the exposure to mechanical stress. | |||
Lumbar spondylosis is a complicated diagnosis. | |||
* Easy to identify radiographically - its pervasiveness throughout all patient populations makes the exact diagnosis of symptomatic cases extremely difficult. | |||
* 85.5% of individuals aged 45–64 years demonstrate osteophytes within the lumbar spine<ref name=":4" />. | |||
* Degenerative changes may appear in young individuals without no trauma history<ref name=":4" />. | |||
== Clinically Relevant Anatomy == | |||
[[File:Degenerative disc diseaseMRI.jpg|right|frameless|225x225px]] | |||
Spondylosis (degeneration of the lumbar spine) | |||
* Generally initiates from the intervertebral disc which cause progressive biochemical and structural changes to take place, leading to a modification in the physical properties of elasticity and mechanical resistance. | |||
* Disc lesions cause pathological changes in the vertebral bodies, where osteophytes appear, | |||
* Most osteophytes are anterior or lateral in projection. Posterior vertebral osteophytes are less common and only rarely impinge upon the spinal cord or nerve roots.<ref>Cherubino P. et al, Spondylosis and lumbar instability: pathologic changes., Chir Organi Mov. 1994 Jan-Mar;79(1):11-8. | |||
</ref><ref name=":0" /><ref>Zukowski et al. The influence of sex, age and BMI on the degeneration of the lumbar spine, Pubmed, 4 Nov 2011. | |||
</ref> | |||
See also [[Lumbar Anatomy]] | |||
== Epidemiology /Etiology == | |||
Spondylosis is a form of lower back pain and is an important clinical, social, economic and public health problem affecting the worldwide population. | |||
Can be seen as a cascaden of anatomical changes of the spine which lead to more degeneration and change in other spine structures. These changes combine to cause spondylosis and its symptoms.<ref>Brooks BK et al., Lumbar spine spondylolysis in the adult population: using computed tomography to evaluate the possibility of adult onset lumbar spondylosis as a cause of back pain.,Skeletal Radiol., 2010. (level of evidence 4) | |||
</ref> | |||
< | Spondylosis | ||
* Has many possible etiologies and many definitions. | |||
* Incidence is 27-37% of the asymptomatic lower back pain population. eg In the United States, 3% of individuals aged 20-29 years and rising to more than 80% of individuals older than 40 years have lumbar spondylosis.<ref>Laxmaiah Manchikanti, Epidemiology of Low Back Pain,Pain Physician, Volume 3, Number 2, pp 167-192, 2000 (level of evidence 5) | |||
</ref> | |||
* Approximately 84% of men and 74% of women have vertebral osteophytes, most frequently at T9-10 and L3 levels. | |||
* Approximately 30% of men and 28% of women aged 55-64 years have lumbar osteophytes. | |||
* Approximately 20% of men and 22% of women aged 45-64 years have lumbar osteophytes. | |||
* Sex ratio reports have been variable but are essentially equal.<ref>Franz EW. et al ‘ Patient misconceptions concerning lumbar spondylosis diagnosis and treatment’ feb 27 2015 ( level of evidence 3B ) | |||
</ref> | |||
* Appears to be a nonspecific ageing phenomenon. | |||
* Most international studies suggest no relation to lifestyle, height, weight, body mass, physical activity, cigarette and alcohol consumption, or reproductive history. | |||
* Adiposity is seen as a risk factor in British populations, but not in Japanese populations. | |||
* The effects of heavy physical activity are controversial, as is a purported relation to disk degeneration.<ref>Yoshimura N, Dennison E, Wilman C, et al. Epidemiology of chronic disc degeneration and osteoarthritis of the lumbar spine in Britain and Japan: a comparative study. J Rheumatol. 2000 Feb. 27(2):429-33. | |||
</ref> | |||
< | == Characteristics/Clinical Presentation == | ||
[[File:Lower-back-pain.jpg|right|frameless]] | |||
Patients with lumbar spondylosis have pain in the axial spine. | |||
* The location of these degenerate changes is not surprising as nociceptive pain generators that were identified within facet joints, intervertebral disks, sacroiliac joints, nerve root dura and myofascial structures. | |||
These changes may peak in different clinical presentations such as | |||
* [http://www.physio-pedia.com/Lumbar_spinal_stenosis Spinal stenosis] | |||
* [http://www.physio-pedia.com/Disc_Herniation Disk herniation] | |||
* Bulging of the [http://www.physio-pedia.com/Ligamentum_flavum ligamentum flavum] | |||
* [https://www.physio-pedia.com/Spondylolisthesis Spondylolisthesis] | |||
* [[Lumbar Radiculopathy]] | |||
All the above result in a constellation of pain symptoms encompassed in the term neurogenic claudication (NC). | |||
* ie may include (to varying extents) lower back pain, leg pain, as well as numbness and motor weakness to lower extremities that worsen with upright stance and walking, and improve with sitting and supine positioning<ref name=":0" /> | |||
Clinical presentations of radiculopathy may emanate from spondylosis, all of which can be explained by the degenerative process. eg Hypertrophic changes to the superior articular process may intrude upon nerve roots within the upper nerve root canal, dural sac, or prior to exiting from next lower intervertebral canal, depending on their projection<ref name=":0" /> | |||
== Differential Diagnosis == | |||
When a patient is suffering from low back pain, there are a lot of possible pathologies that could be the cause of this pain. Along with lumbar spondylosis (and its sub-divisions), there are other causes as well. | |||
<br>• [http://www.physio-pedia.com/Rheumatoid_Arthritis Rheumatoid arthritis]- We can understand why some clinicians would include rheumatoid arthritis, because there are sub-divisions of lumbar spondylosis that have a lot of similarities with arthritis. <br>• Excessive exercise<br>•[http://www.physio-pedia.com/Ankylosing_Spondylitis Ankylosing Spondylitis]<br>• [http://www.physio-pedia.com/Coccygodynia_(Coccydynia,_Coccalgia,_Tailbone_Pain) Coccyx Pain]<br>• Spinal Masses<br>• [https://www.physio-pedia.com/Specific_Low_Back_Pain Infection]<br>• [http://www.physio-pedia.com/Spondylodiscitis Discitis]<br>• [http://www.physio-pedia.com/Lumbar_compression_fracture Lumbar Compression Fracture] <br>• [[Mechanical low back pain|Mechanical Low Back Pain<br>•]] [http://www.physio-pedia.com/Muscle_Injuries Overuse Injury]<ref>Beth B Froese, MD , Lumbar Spondylolysis and Spondylolisthesis Differential Diagnoses, American Academy of Physical Medicine and Rehabilitation, American Medical Association, Illinois State Medical Society, 2014. | |||
</ref> | |||
== Diagnostic Procedures == | |||
see [[Common Diagnostic Imaging of the Lumbar Spine]] | |||
It is important that diagnostic procedures are only ordered when warranted. For simple low back pain with no red flags a conservative approach incorporating pain medication and physiotherapy should be taken in the acute stage. When chronic pain is present diagnostic tools should be considered. The below 2 minute video outlines this. | |||
{{#ev:youtube|https://www.youtube.com/watch?v=PpWdBY5WJo8|width}}<ref>Potea. Accurate diagnosis of low back pain. Available from: https://www.youtube.com/watch?v=PpWdBY5WJo8 (last accessed 9.3.2019)</ref> | |||
== Outcome Measures == | |||
* [ | * [http://www.physio-pedia.com/Numeric_Pain_Rating_Scale Numeric pain rating scale (NPRS)] | ||
* [http://www.physio-pedia.com/Roland%E2%80%90Morris_Disability_Questionnaire Roland Morris disability questionnaire (RMDQ)] | |||
* [http://www.physio-pedia.com/Oswestry_Disability_Index Oswestry disability index (ODI)] | |||
* [http://www.physio-pedia.com/Pain_Self-Efficacy_Questionnaire_(PSEQ) Pain self-efficacy questionnaire (PSEQ)] | |||
* [http://www.physio-pedia.com/Patient_Specific_Functional_Scale The patient-specific functional scale (PSFS)] | |||
== Examination == | |||
[[File:LBP Triage.png|right|frameless|645x645px]] | |||
For a more comprehensive guide see [[Lumbar Assessment]] | |||
<br>1. General examination of the spine | |||
* Inspection of the entire spine | |||
* Look for any obvious swellings or surgical scars. | |||
* Assess for deformity: scoliosis, kyphosis, loss of lumbar lordosis or hyperlordosis of the lumbar spine. Look for shoulder asymmetry and pelvic tilt. | |||
2. Palpation | |||
* Palpate for tenderness over bone and soft tissues. | |||
* Perform an abdominal examination to identify any masses and consider a rectal examination to exclude other pathologies in this region | |||
3. Movement | |||
* Flexion, extension, lateral flexion and rotation. Examination of the spine must also include examination of the shoulders and examination of the hips to exclude these joints as a cause of the symptoms. | |||
4. Neurovascular examination | |||
* Sensation, tone, power and reflexes should be assessed. All peripheral pulses should also be checked, as vascular claudication in the upper and lower limbs can mimic symptoms of radiculopathy or canal stenosis. | |||
== Medical Management == | |||
There is little consensus about the definitive treatment approach due to a lack of information about the sources of chronic lower back pain, | |||
* [[File:Facet joint injection.png|right|frameless]]There is a surprisingly high percentage of the patients that have misconceptions regarding the diagnosis and the treatment of lumbar spondylosis and these misconceptions persist in patients with a history of spine surgery. | |||
* Patients over-emphasize the value of radiological studies and have mixed perceptions of the relative risk and effectiveness of surgical intervention cf conservative management. | |||
* These misconceptions have the potential to alter patient expectations and decrease satisfaction potentially negatively impacting patient outcomes and subjective valuation of physician performance. | |||
# '''Non-surgical Management''' | |||
See | |||
* [[Pharmacology in Pain Management]] | |||
* [[Therapeutic Corticosteroid Injection]] | |||
* [[Lumbar Facet Joint Injections]] | |||
'''2. Surgical Management'''<u></u> | |||
Each type comes with its own risks and benefits. | |||
* Spinal fusion. This is the most common surgery for chronic nonspecific back pain with degenerative changes (joining of vertebrae together aimed at limiting the motion between vertebrae stretch on associated nerves). | |||
* Laminectomy. This is the most common surgery for lumbar spinal stenosis (removal of part of the bone, bone spurs, or ligaments, aimed at relieving pressure on spinal nerves, can make your spine less stable) | |||
* Foraminotomy. This surgery is used to relieve pain associated with a compressed nerve in the spine. | |||
* Diskectomy. | |||
* Disk replacement. | |||
* Interlaminar implant<ref>Webmd [https://www.webmd.com/back-pain/back-surgery-types#1 Spinal surgery] Available from:https://www.webmd.com/back-pain/back-surgery-types#1 (last accessed 9.9.2020)</ref>.<u></u> | |||
== Physical Therapy Management<u></u> == | |||
Educating the patient: may include reviews of lumbar anatomy, explanations of the concept of posture, ergonomics and giving appropriate back exercises.<ref>Sahin, N., et al., Effectiveness of back school for treatment of pain and functional disability in patients with chronic low back pain: A randomized controlled trial. Volume 43, Issue 3, Pages: 224-229. (level of evidence 1B) | |||
</ref><ref>Book: Evidence-Based Management of Low Back Pain by Simon Dagenais, Scott Haldeman (level of evidence 5) | |||
</ref> | |||
See [[Interventions for LBP]] | |||
* [[Manual Therapy Techniques For The Lumbar Spine]] | |||
* [[Mckenzie Method]] | |||
* [[Massage]] | |||
* [[Transcutaneous Electrical Nerve Stimulation (TENS)|TENS]] | |||
* [[Yoga]] | |||
* [[Tai Chi and the Older Person|TaiChi]] | |||
* [[Back School]] | |||
Other modalities include | |||
'''Lumbar Back Support:''' Can be beneficial for patients suffering from chronic LBP. It occurs to limit spine motion, stabilize, correct deformity and reduce mechanical forces. There is no consensus if it may function as a placebo or really improve pain and functional ability. (level of evidence 1A) Sitting decreases lumbar lordosis and increase disc pressure, squeeze on the ischium and muscle activity in the lower back. These are all associated with low back pain. The study of Makhsous et al. resulted in a diminished lumbar spine load and lumbar muscular activity with lumbar back support. This may possibly lessen low back pain while sitting.<ref>Makhsous, M., et al., Biomechanical effects of sitting with adjustable ischial and lumbar support on occupational low back pain: evaluation of sitting load and back muscle activity. BMC Musculoskeletal Disorders, 2009. (level of evidence 5) | |||
</ref> | |||
'''Taping:''' Another non-surgical management could be taping. A lot of studies have shown that taping helps to relieve pain in the lower back. This tape could be standard tape or kinesiotape as it is shown that there is no difference between both tapes. It is also important to note that taping alone is not enough, it should be used during the therapy to improve ROM etc.<ref>Nelson, N. L. (2016). Kinesio taping for chronic low back pain: A systematic review. Journal of Bodywork and Movement Therapies. (level of evidence 1A) | |||
</ref><ref>Luz Júnior, M. A., Sousa, M. V., Neves, L. A., Cezar, A. A., & Costa, L. O. (2015). Kinesio Taping® is not better than placebo in reducing pain and disability in patients with chronic non-specific low back pain: a randomized controlled trial. Brazilian journal of physical therapy, (AHEAD), 0-0. (level of evidence 1B) | |||
</ref> | |||
'''Lumbar Support:''' Lumbar support with the help of braces are used for stabilization and reducing mechanical forces, they are also produced to limit spine motion and correct deformity of the spine. There is limited evidence-based research available about the efficacy of lumbar supports regarding patient improvement and functional ability to go back to work. An example of a brace for Lumbal support is [[The_Lyon_Antikyphosis_Brace|The Lyon Antikyphosis Brace]]. This brace has the best results for patients with scoliosis but could also help patients suffering from lumbar spondylosis.<ref>De Mauroy, Jean Claude, et al. "The Lyon brace." Disability and Rehabilitation: Assistive Technology 3.3 (2008): 139-145. [Level of evidence 5] | |||
</ref> Braces may have effects by massaging and heating the painful areas, there is also a probability that the lumbar supports work as a placebo. | |||
'''Bio-psychosocial Approach:''' Multidisciplinary back therapy may be needed. A bio-psychosocial approach involved reinforcement, modified expectations, imagery/relaxation techniques, and learned control of physiological responses aim to reduce a patient’s perception of disability and pain symptoms. | |||
== Key Evidence == | |||
Busanich, Brian M., and Susan D. Verscheure. "Does McKenzie therapy improve outcomes for back pain?." Journal of athletic training 41.1 (2006): 117. | |||
Garet, Matthew, et al. "Nonoperative treatment in lumbar spondylolysis and spondylolisthesis a systematic review." Sports health: a multidisciplinary approach (2013): 1941738113480936. | |||
== Clinical Bottom Line == | |||
Lumbar spondylosis can be described as a degeneration of the [[Lumbar Vertebrae|lumbar vertebrae.]] | |||
* It is a form of [[Low Back Pain|low back pain]] and is an important clinical, social, economic and public health problem affecting the worldwide population. | |||
* It is a disorder with many possible etiologies and many definitions. | |||
* For the clinical diagnosis of lumbar spondylosis, a thorough investigation is necessary to ensure that other pathologies are excluded. In clinical practice we use: [[MRI Scans|MRI]], [[CT Scans|CT]], SPECT and [[X-Rays|X-ray]] and a general examination of the spine. | |||
* The medical management can be approached by a surgical or non-surgical treatment, there is no consensus about the most effective therapy. | |||
* The physical therapy management consists of a multidisciplinary approach, which includes lumbar traction, manipulation of the spine, massage therapy, TENS, [[Back School|back school]] and Lumbar back supports. | |||
* The choice on which therapy to use, depends on the individual wishes and needs of the patient; there is no standard assessment for every pathology. | |||
== References == | |||
<references /> | <references /> | ||
[[Category:Lumbar Spine]] | |||
[[Category:Lumbar Spine - Conditions]] | |||
[[Category:Conditions]] | |||
[[Category:One Page Project]] | |||
Revision as of 17:45, 30 November 2020
Page Owner - Nawal Farooq as part of the One Page Project
Definition/Description[edit | edit source]
Spondylosis may be applied nonspecifically to any and all degenerative conditions affecting the disks, vertebral bodies, and/or associated joints of the lumbar spine[1].[2]
- Low back pain (LBP) affects approximately 60–85% of adults during some point in their lives.
Spondylosis
- Not a clinical diagnosis but instead a descriptive term utilized to designate spinal problems.
- Encompasses numerous associated pathologies including spinal stenosis, degenerative spondylolisthesis, osteoarthritis, ageing, trauma and just the daily use of the intervertebral discs, the vertebrae, and the associated joints.[3]
- The lumbar region the most affected, because of the exposure to mechanical stress.
Lumbar spondylosis is a complicated diagnosis.
- Easy to identify radiographically - its pervasiveness throughout all patient populations makes the exact diagnosis of symptomatic cases extremely difficult.
- 85.5% of individuals aged 45–64 years demonstrate osteophytes within the lumbar spine[1].
- Degenerative changes may appear in young individuals without no trauma history[1].
Clinically Relevant Anatomy[edit | edit source]
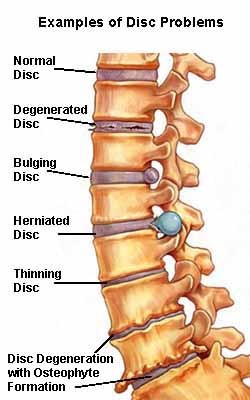
Spondylosis (degeneration of the lumbar spine)
- Generally initiates from the intervertebral disc which cause progressive biochemical and structural changes to take place, leading to a modification in the physical properties of elasticity and mechanical resistance.
- Disc lesions cause pathological changes in the vertebral bodies, where osteophytes appear,
- Most osteophytes are anterior or lateral in projection. Posterior vertebral osteophytes are less common and only rarely impinge upon the spinal cord or nerve roots.[4][2][5]
See also Lumbar Anatomy
Epidemiology /Etiology[edit | edit source]
Spondylosis is a form of lower back pain and is an important clinical, social, economic and public health problem affecting the worldwide population.
Can be seen as a cascaden of anatomical changes of the spine which lead to more degeneration and change in other spine structures. These changes combine to cause spondylosis and its symptoms.[6]
Spondylosis
- Has many possible etiologies and many definitions.
- Incidence is 27-37% of the asymptomatic lower back pain population. eg In the United States, 3% of individuals aged 20-29 years and rising to more than 80% of individuals older than 40 years have lumbar spondylosis.[7]
- Approximately 84% of men and 74% of women have vertebral osteophytes, most frequently at T9-10 and L3 levels.
- Approximately 30% of men and 28% of women aged 55-64 years have lumbar osteophytes.
- Approximately 20% of men and 22% of women aged 45-64 years have lumbar osteophytes.
- Sex ratio reports have been variable but are essentially equal.[8]
- Appears to be a nonspecific ageing phenomenon.
- Most international studies suggest no relation to lifestyle, height, weight, body mass, physical activity, cigarette and alcohol consumption, or reproductive history.
- Adiposity is seen as a risk factor in British populations, but not in Japanese populations.
- The effects of heavy physical activity are controversial, as is a purported relation to disk degeneration.[9]
Characteristics/Clinical Presentation[edit | edit source]
Patients with lumbar spondylosis have pain in the axial spine.
- The location of these degenerate changes is not surprising as nociceptive pain generators that were identified within facet joints, intervertebral disks, sacroiliac joints, nerve root dura and myofascial structures.
These changes may peak in different clinical presentations such as
- Spinal stenosis
- Disk herniation
- Bulging of the ligamentum flavum
- Spondylolisthesis
- Lumbar Radiculopathy
All the above result in a constellation of pain symptoms encompassed in the term neurogenic claudication (NC).
- ie may include (to varying extents) lower back pain, leg pain, as well as numbness and motor weakness to lower extremities that worsen with upright stance and walking, and improve with sitting and supine positioning[2]
Clinical presentations of radiculopathy may emanate from spondylosis, all of which can be explained by the degenerative process. eg Hypertrophic changes to the superior articular process may intrude upon nerve roots within the upper nerve root canal, dural sac, or prior to exiting from next lower intervertebral canal, depending on their projection[2]
Differential Diagnosis[edit | edit source]
When a patient is suffering from low back pain, there are a lot of possible pathologies that could be the cause of this pain. Along with lumbar spondylosis (and its sub-divisions), there are other causes as well.
• Rheumatoid arthritis- We can understand why some clinicians would include rheumatoid arthritis, because there are sub-divisions of lumbar spondylosis that have a lot of similarities with arthritis.
• Excessive exercise
•Ankylosing Spondylitis
• Coccyx Pain
• Spinal Masses
• Infection
• Discitis
• Lumbar Compression Fracture
• Mechanical Low Back Pain
• Overuse Injury[10]
Diagnostic Procedures[edit | edit source]
see Common Diagnostic Imaging of the Lumbar Spine
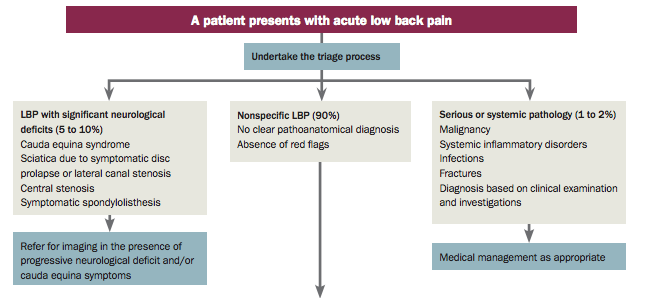
It is important that diagnostic procedures are only ordered when warranted. For simple low back pain with no red flags a conservative approach incorporating pain medication and physiotherapy should be taken in the acute stage. When chronic pain is present diagnostic tools should be considered. The below 2 minute video outlines this.
Outcome Measures[edit | edit source]
Examination[edit | edit source]
For a more comprehensive guide see Lumbar Assessment
1. General examination of the spine
- Inspection of the entire spine
- Look for any obvious swellings or surgical scars.
- Assess for deformity: scoliosis, kyphosis, loss of lumbar lordosis or hyperlordosis of the lumbar spine. Look for shoulder asymmetry and pelvic tilt.
2. Palpation
- Palpate for tenderness over bone and soft tissues.
- Perform an abdominal examination to identify any masses and consider a rectal examination to exclude other pathologies in this region
3. Movement
- Flexion, extension, lateral flexion and rotation. Examination of the spine must also include examination of the shoulders and examination of the hips to exclude these joints as a cause of the symptoms.
4. Neurovascular examination
- Sensation, tone, power and reflexes should be assessed. All peripheral pulses should also be checked, as vascular claudication in the upper and lower limbs can mimic symptoms of radiculopathy or canal stenosis.
Medical Management[edit | edit source]
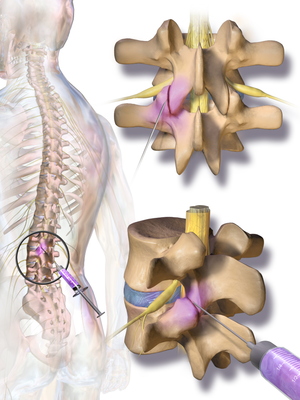
There is little consensus about the definitive treatment approach due to a lack of information about the sources of chronic lower back pain,
- There is a surprisingly high percentage of the patients that have misconceptions regarding the diagnosis and the treatment of lumbar spondylosis and these misconceptions persist in patients with a history of spine surgery.
- Patients over-emphasize the value of radiological studies and have mixed perceptions of the relative risk and effectiveness of surgical intervention cf conservative management.
- These misconceptions have the potential to alter patient expectations and decrease satisfaction potentially negatively impacting patient outcomes and subjective valuation of physician performance.
- Non-surgical Management
See
2. Surgical Management
Each type comes with its own risks and benefits.
- Spinal fusion. This is the most common surgery for chronic nonspecific back pain with degenerative changes (joining of vertebrae together aimed at limiting the motion between vertebrae stretch on associated nerves).
- Laminectomy. This is the most common surgery for lumbar spinal stenosis (removal of part of the bone, bone spurs, or ligaments, aimed at relieving pressure on spinal nerves, can make your spine less stable)
- Foraminotomy. This surgery is used to relieve pain associated with a compressed nerve in the spine.
- Diskectomy.
- Disk replacement.
- Interlaminar implant[12].
Physical Therapy Management[edit | edit source]
Educating the patient: may include reviews of lumbar anatomy, explanations of the concept of posture, ergonomics and giving appropriate back exercises.[13][14]
Other modalities include
Lumbar Back Support: Can be beneficial for patients suffering from chronic LBP. It occurs to limit spine motion, stabilize, correct deformity and reduce mechanical forces. There is no consensus if it may function as a placebo or really improve pain and functional ability. (level of evidence 1A) Sitting decreases lumbar lordosis and increase disc pressure, squeeze on the ischium and muscle activity in the lower back. These are all associated with low back pain. The study of Makhsous et al. resulted in a diminished lumbar spine load and lumbar muscular activity with lumbar back support. This may possibly lessen low back pain while sitting.[15]
Taping: Another non-surgical management could be taping. A lot of studies have shown that taping helps to relieve pain in the lower back. This tape could be standard tape or kinesiotape as it is shown that there is no difference between both tapes. It is also important to note that taping alone is not enough, it should be used during the therapy to improve ROM etc.[16][17]
Lumbar Support: Lumbar support with the help of braces are used for stabilization and reducing mechanical forces, they are also produced to limit spine motion and correct deformity of the spine. There is limited evidence-based research available about the efficacy of lumbar supports regarding patient improvement and functional ability to go back to work. An example of a brace for Lumbal support is The Lyon Antikyphosis Brace. This brace has the best results for patients with scoliosis but could also help patients suffering from lumbar spondylosis.[18] Braces may have effects by massaging and heating the painful areas, there is also a probability that the lumbar supports work as a placebo.
Bio-psychosocial Approach: Multidisciplinary back therapy may be needed. A bio-psychosocial approach involved reinforcement, modified expectations, imagery/relaxation techniques, and learned control of physiological responses aim to reduce a patient’s perception of disability and pain symptoms.
Key Evidence[edit | edit source]
Busanich, Brian M., and Susan D. Verscheure. "Does McKenzie therapy improve outcomes for back pain?." Journal of athletic training 41.1 (2006): 117.
Garet, Matthew, et al. "Nonoperative treatment in lumbar spondylolysis and spondylolisthesis a systematic review." Sports health: a multidisciplinary approach (2013): 1941738113480936.
Clinical Bottom Line[edit | edit source]
Lumbar spondylosis can be described as a degeneration of the lumbar vertebrae.
- It is a form of low back pain and is an important clinical, social, economic and public health problem affecting the worldwide population.
- It is a disorder with many possible etiologies and many definitions.
- For the clinical diagnosis of lumbar spondylosis, a thorough investigation is necessary to ensure that other pathologies are excluded. In clinical practice we use: MRI, CT, SPECT and X-ray and a general examination of the spine.
- The medical management can be approached by a surgical or non-surgical treatment, there is no consensus about the most effective therapy.
- The physical therapy management consists of a multidisciplinary approach, which includes lumbar traction, manipulation of the spine, massage therapy, TENS, back school and Lumbar back supports.
- The choice on which therapy to use, depends on the individual wishes and needs of the patient; there is no standard assessment for every pathology.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Middleton K, Fish DE. Lumbar spondylosis: clinical presentation and treatment approaches. Current Reviews in Musculoskeletal Medicine. 2009 Jun 1;2(2):94-104. Available from:https://link.springer.com/article/10.1007/s12178-009-9051-x (last accessed 8.9.2020)
- ↑ 2.0 2.1 2.2 2.3 Middleton, Kimberley, and David E. Fish. “Lumbar Spondylosis: Clinical Presentation and Treatment Approaches.” Current Reviews in Musculoskeletal Medicine 2, no. 2 (March 25, 2009): 94–104.
- ↑ Gibson, J. N. Alastair, and Gordon Waddell. “Surgery for Degenerative Lumbar Spondylosis: Updated Cochrane Review.” Spine 30, no. 20 (October 15, 2005): 2312–20.
- ↑ Cherubino P. et al, Spondylosis and lumbar instability: pathologic changes., Chir Organi Mov. 1994 Jan-Mar;79(1):11-8.
- ↑ Zukowski et al. The influence of sex, age and BMI on the degeneration of the lumbar spine, Pubmed, 4 Nov 2011.
- ↑ Brooks BK et al., Lumbar spine spondylolysis in the adult population: using computed tomography to evaluate the possibility of adult onset lumbar spondylosis as a cause of back pain.,Skeletal Radiol., 2010. (level of evidence 4)
- ↑ Laxmaiah Manchikanti, Epidemiology of Low Back Pain,Pain Physician, Volume 3, Number 2, pp 167-192, 2000 (level of evidence 5)
- ↑ Franz EW. et al ‘ Patient misconceptions concerning lumbar spondylosis diagnosis and treatment’ feb 27 2015 ( level of evidence 3B )
- ↑ Yoshimura N, Dennison E, Wilman C, et al. Epidemiology of chronic disc degeneration and osteoarthritis of the lumbar spine in Britain and Japan: a comparative study. J Rheumatol. 2000 Feb. 27(2):429-33.
- ↑ Beth B Froese, MD , Lumbar Spondylolysis and Spondylolisthesis Differential Diagnoses, American Academy of Physical Medicine and Rehabilitation, American Medical Association, Illinois State Medical Society, 2014.
- ↑ Potea. Accurate diagnosis of low back pain. Available from: https://www.youtube.com/watch?v=PpWdBY5WJo8 (last accessed 9.3.2019)
- ↑ Webmd Spinal surgery Available from:https://www.webmd.com/back-pain/back-surgery-types#1 (last accessed 9.9.2020)
- ↑ Sahin, N., et al., Effectiveness of back school for treatment of pain and functional disability in patients with chronic low back pain: A randomized controlled trial. Volume 43, Issue 3, Pages: 224-229. (level of evidence 1B)
- ↑ Book: Evidence-Based Management of Low Back Pain by Simon Dagenais, Scott Haldeman (level of evidence 5)
- ↑ Makhsous, M., et al., Biomechanical effects of sitting with adjustable ischial and lumbar support on occupational low back pain: evaluation of sitting load and back muscle activity. BMC Musculoskeletal Disorders, 2009. (level of evidence 5)
- ↑ Nelson, N. L. (2016). Kinesio taping for chronic low back pain: A systematic review. Journal of Bodywork and Movement Therapies. (level of evidence 1A)
- ↑ Luz Júnior, M. A., Sousa, M. V., Neves, L. A., Cezar, A. A., & Costa, L. O. (2015). Kinesio Taping® is not better than placebo in reducing pain and disability in patients with chronic non-specific low back pain: a randomized controlled trial. Brazilian journal of physical therapy, (AHEAD), 0-0. (level of evidence 1B)
- ↑ De Mauroy, Jean Claude, et al. "The Lyon brace." Disability and Rehabilitation: Assistive Technology 3.3 (2008): 139-145. [Level of evidence 5]