Malignant Melanoma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 73: | Line 73: | ||
== Staging of Melanoma == | == Staging of Melanoma == | ||
[[Image:Clark levels.jpg|484x271px|right|frameless]]Prognostic staging for malignant melanoma is accomplished using either the Breslow thickness or Clark level 1, 2. | |||
Breslow thickness | |||
# <0.76 mm: 5-year survival rate: 95% to 100% | |||
# 0.76-1.5 mm: 5-year survival rate: 80% to 96% | |||
# 1.5-4 mm: 5-year survival rate: 60% to 75% | |||
# >4 mm: 5-year survival rate: 37% to 50% | |||
Clark level | |||
# level I: tumour cells are maintained above the basement membrane | |||
# level II: tumour cells have infiltrated the papillary dermis | |||
# level III: tumour cells extend between papillary and reticular dermis, but do not invade the reticular dermis | |||
# level IV: tumour cells have infiltrated the reticular dermis | |||
# level V: tumour cells extend into subcutaneous tissue<ref name=":0" /><u></u> | |||
<u></u><u></u> | |||
== <u></u>Associated Comorbidities == | |||
Individuals who have been diagnosed with dysplastic nevus syndrome often develop malignant melanoma later in life. This syndrome, also known as atypical mole syndrome, is a familial disorder that results in a significant number of large moles that have an irregular shape or color. They frequently appear on skin that is exposed to the sun but can develop anywhere on the body. The dysplastic nevi have up to a 50% chance of developing into malignant melanoma; therefore, they are often surgically removed to prevent cancer. Individuals with this syndrome are encouraged to have routine skin exams by a dermatologist and should preform monthly self-skin exams. <ref name="Goodman2">Goodman CC, Fuller KS. The Integumentary System. In: Pathology Implications for the Physical Therapist. 3rd ed. St. Louis, MO: Saunders Elsevier; 2009: 392-452.</ref><ref name="ACS">Melanoma Skin Cancer. American Cancer Society. Available at http://www.cancer.org/cancer/skincancer-melanoma/index. Accessed March 17, 2014.</ref><br> | |||
Individuals who have been diagnosed with dysplastic nevus syndrome often develop malignant melanoma later in life. This syndrome, also known as atypical mole syndrome, is a familial disorder that results in a significant number of large moles that have an irregular shape or color. They frequently appear on skin that is exposed to the sun but can develop anywhere on the body. The dysplastic nevi have up to a 50% chance of developing into malignant melanoma; therefore, they are often surgically removed to prevent cancer. Individuals with this syndrome are encouraged to have routine skin exams by a dermatologist and should preform monthly self-skin exams. <ref name="Goodman2" /><ref name="ACS" /><br> | |||
There are no specific comorbidities that are closely linked to malignant melanoma. Comorbidities commonly reported in patients with cancer are hypertension, diabetes, arthritis, heart disease, and upper gastrointestinal disease. <ref name="Medline">Alappattu M, Coronado R, Lee D, Bour B, George S. Clinical characteristics of patients with cancer referred for outpatient physical therapy. Physical Therapy [serial on the Internet]. (2015, Apr), [cited April 5, 2017]; 95(4): 526-538. Available from: MEDLINE.</ref> Research has shown an association between comorbidities such as these with delay of melanoma diagnosis, more advanced stages of melanoma, and less aggressive treatments. Therefore, improved efforts to treat these comorbidities may result in decreased mortality rates among individuals with melanoma.<ref name="Comorbidity">A F Grann, T Frøslev, A B Olesen, H Schmidt, T L Lash. The impact of comorbidity and stage on prognosis of Danish melanoma patients, 1987–2009: a registry-based cohort study [Internet]. British Journal of Cancer. 2013. p. 265–71. Available from: http://www.nature.com/bjc/journal/v109/n1/full/bjc2013246a.html</ref> | There are no specific comorbidities that are closely linked to malignant melanoma. Comorbidities commonly reported in patients with cancer are hypertension, diabetes, arthritis, heart disease, and upper gastrointestinal disease. <ref name="Medline">Alappattu M, Coronado R, Lee D, Bour B, George S. Clinical characteristics of patients with cancer referred for outpatient physical therapy. Physical Therapy [serial on the Internet]. (2015, Apr), [cited April 5, 2017]; 95(4): 526-538. Available from: MEDLINE.</ref> Research has shown an association between comorbidities such as these with delay of melanoma diagnosis, more advanced stages of melanoma, and less aggressive treatments. Therefore, improved efforts to treat these comorbidities may result in decreased mortality rates among individuals with melanoma.<ref name="Comorbidity">A F Grann, T Frøslev, A B Olesen, H Schmidt, T L Lash. The impact of comorbidity and stage on prognosis of Danish melanoma patients, 1987–2009: a registry-based cohort study [Internet]. British Journal of Cancer. 2013. p. 265–71. Available from: http://www.nature.com/bjc/journal/v109/n1/full/bjc2013246a.html</ref> | ||
Revision as of 08:03, 3 September 2020
Original Editors - Emily Erwin & Brooke Sowards from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Erwin, Ellen Hosking, Brooke Sowards, Lucinda hampton, Elaine Lonnemann, Kim Jackson, Vidya Acharya, WikiSysop, 127.0.0.1, Wendy Walker and Calli Paydo
Introduction[edit | edit source]
A melanoma (see image R, nodular melanoma) is a tumor produced by the malignant transformation of melanocytes.
- Melanocytes are derived from the neural crest; consequently, melanomas, although they usually occur on the skin, can arise in other locations where neural crest cells migrate, such as the gastrointestinal tract and brain.
- Metastatic melanoma is known for its aggressive nature and for its ability to metastasise to a variety of atypical locations, which is why it demonstrates poor prognostic characteristics[1]
- The five-year relative survival rate for patients with stage 0 melanoma is 97%, compared with about 10% for those with stage IV disease[2].
The below 2 minute video shows the different type of skin cancers (including melanoma)
Etiology[edit | edit source]
The causes may be related to:
- Family history - Positive family history in 5% to 10% of patients; a 2.2-fold higher risk with at least one affected relative
- Personal characteristics - Blue eyes, fair and/or red hair, pale complexion; skin reaction to sunlight (easily sunburned); freckling; benign and/or dysplastic melanocytic nevi (number has better correlation than size); immunosuppressive states (transplantation patients, hematologic malignancies)
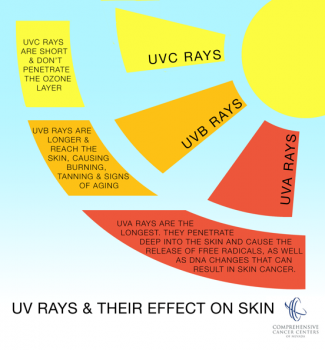
- Sun exposure over a lifetime - High UVB and UVA radiation exposure (Recent evidence has shown that the risk of melanoma is higher in people who use sunscreen. Because sunscreen mostly blocks UVB, people using sunscreen may be exposed to UVA more than the general public, provided those people are exposed to the sun more than the public at large); low latitude; number of blistering sunburns; use of tanning beds
- Atypical mole syndrome (formerly termed B-K mole syndrome, dysplastic nevus syndrome, familial atypical multiple mole melanoma) - Over ten years, 10.7% risk of melanoma (vs 0.62% of controls); higher risk of melanoma depending on number of family members affected (nearly 100% risk if two or more relatives have dysplastic nevi and melanoma)
- Socioeconomic status - Lower socioeconomic status may be linked to more advanced disease at the time of detection. One survey of newly-diagnosed patients found that low-SES individuals have decreased melanoma risk perception and knowledge of the disease.[2]
Epidemiology[edit | edit source]
The incidence of malignant melanoma is rapidly increasing worldwide, and this increase is occurring at a faster rate than that of any other cancer except lung cancer in women[2].
- Melanoma accounts for ~5% of all skin cancers, however, it remains the leading cause of death amongst skin cancers.
- The risk of metastatic progression has a strong association with the site of the initial primary melanoma, with melanomas arising from the head, neck and trunk carrying a higher risk of metastatic progression than those melanomas arising from the limbs[1]
- Melanoma is more common in Whites than in Blacks and Asians.
- Overall, melanoma is the fifth most common malignancy in men and the seventh most common malignancy in women, accounting for 5% and 4% of all new cancer cases, respectively.
- The average age at diagnosis is 57 years, and up to 75% of patients are younger than 70 years.
- Melanoma is notorious for affecting young and middle-aged people, unlike other solid tumors which mainly affect older adults. It is commonly found in patients younger than 55 years, and it accounts for the third highest number of lives lost across all cancers[2].
Pathophysiology[edit | edit source]
Melanomas
- May develop in or near a previously existing precursor lesion or in healthy-appearing skin.
- Solar irradiation induces many of these melanomas.
- May occur in unexposed areas of the skin, including the palms, soles, and perineum.
Certain lesions are considered to be precursor lesions of melanoma. These include the following nevi (moles):
- Common acquired nevus
- Dysplastic nevus
- Congenital nevus
- Cellular blue nevus
Melanomas have 2 growth phases,
- Radial malignant - Cells grow in a radial fashion in the epidermis
- Vertical - With time, most melanomas progress to the vertical growth phase, in which the malignant cells invade the dermis and develop the ability to metastasize.
Clinically, lesions are classified according to their depth, as follows:
- Thin - 1 mm or less
- Moderate - 1 mm to 4 mm
- Thick- greater than 4 mm
The 4 major types of melanoma, classified according to growth pattern, are as follows:
- Superficial spreading melanoma constitutes approximately 70% of melanomas; usually flat but may become irregular and elevated in later stages; the lesions average 2 cm in diameter, with variegated colors, as well as peripheral notches, indentations, or both
- Nodular melanoma accounts for approximately 15% to 30% of melanoma diagnoses; the tumors typically are blue-black but may lack pigment in some circumstances
- Lentigo maligna melanoma represents 4% to 10% of melanomas; the tumors are often larger than 3 cm, flat, and tan, with marked notching of the borders; they begin as small, freckle-like lesions
- Acral lentiginous melanoma constitutes 2% to 8% of melanomas in Whites and 35% to 60% of them in dark-skinned people; may appear on the palms and soles as flat, tan, or brown stains with irregular borders; subungual lesions can be brown or black, with ulcerations in later stages.
Characteristics/Clinical Presentation[edit | edit source]
Most commonly, the history includes either changing characteristics in an existing mole or the identification of a new mole.
The characteristics of melanoma are commonly known by the acronym ABCDE and include the following:
- A - Asymmetry
- B - Irregular border
- C - Color variations, especially red, white, and blue tones in a brown or black lesion
- D - Diameter greater than 6 mm
- E - Elevated surface
Melanomas may itch, bleed, ulcerate, or develop satellites.
Patients who present with metastatic disease or with primary sites other than the skin have signs and symptoms related to the affected organ system(s).
Important to examine all lymph node groups.[2]
Staging of Melanoma[edit | edit source]
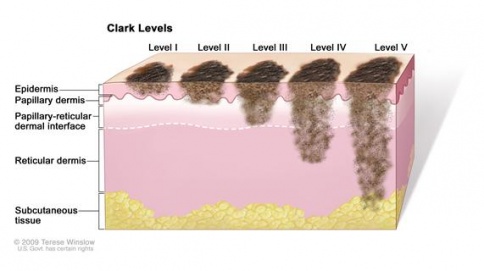
Prognostic staging for malignant melanoma is accomplished using either the Breslow thickness or Clark level 1, 2.
Breslow thickness
- <0.76 mm: 5-year survival rate: 95% to 100%
- 0.76-1.5 mm: 5-year survival rate: 80% to 96%
- 1.5-4 mm: 5-year survival rate: 60% to 75%
- >4 mm: 5-year survival rate: 37% to 50%
Clark level
- level I: tumour cells are maintained above the basement membrane
- level II: tumour cells have infiltrated the papillary dermis
- level III: tumour cells extend between papillary and reticular dermis, but do not invade the reticular dermis
- level IV: tumour cells have infiltrated the reticular dermis
- level V: tumour cells extend into subcutaneous tissue[1]
Associated Comorbidities[edit | edit source]
Individuals who have been diagnosed with dysplastic nevus syndrome often develop malignant melanoma later in life. This syndrome, also known as atypical mole syndrome, is a familial disorder that results in a significant number of large moles that have an irregular shape or color. They frequently appear on skin that is exposed to the sun but can develop anywhere on the body. The dysplastic nevi have up to a 50% chance of developing into malignant melanoma; therefore, they are often surgically removed to prevent cancer. Individuals with this syndrome are encouraged to have routine skin exams by a dermatologist and should preform monthly self-skin exams. [3][4]
There are no specific comorbidities that are closely linked to malignant melanoma. Comorbidities commonly reported in patients with cancer are hypertension, diabetes, arthritis, heart disease, and upper gastrointestinal disease. [5] Research has shown an association between comorbidities such as these with delay of melanoma diagnosis, more advanced stages of melanoma, and less aggressive treatments. Therefore, improved efforts to treat these comorbidities may result in decreased mortality rates among individuals with melanoma.[6]
Medications[edit | edit source]
Common FDA approved medications for the treatment of malignant melanoma are divided into three categories and listed below. [7]
Immunotherapies:[edit | edit source]
- Imlygic (talimogene laherparepvec "t-vec")
- Intron A (high-dose interferon alfa-2b)
- Keytruda (pembrolizumab)
- Opdivo (nivolumab)
- Opdivo (nivolumab) and Yervoy (ipilimumab) combination
- Proleukin / il-2 (interleukin-2)
- Sylatron (peginterferon alfa-2b)
- Yervoy (ipilimumab)
Targeted Therapies:[edit | edit source]
- Cotellic (cobimetinib) and Zelboraf (vemurafenib) combination
- Mekinist (trametinib)
- Mekinist (trametinib) and Tafinlar (dabrafenib) combination
- Tafinlar (dabrafenib)
- Zelboraf (vemurafenib)
Chemotherapy:[edit | edit source]
- DTIC (dacarbazine)
Common side effects that may be experienced while undergoing cancer treatment include flu-like symptoms, fatigue, nausea, changes in taste and smell, loss of appetite, and depression. Flu-like symptoms may include fever, chills, headache, and muscle aches. These symptoms are more common in those receiving immunotherapy. Those receiving immunotherapy, chemotherapy, and radiation therapy often experience a feeling of intense tiredness or weakness not usually relieved with rest or sleep. Nausea can be a problematic side-effect not only because of the discomfort it causes, but it can also prevent proper nutrition. It is common in immunotherapy. Loss of appetite commonly results with immunotherapy, targeted therapy, chemotherapy and radiation therapy. Loss of appetite may be due to nausea, vomiting, depression, or changes in one’s taste or smell. Medications used to treat melanoma may induce depression or worsen preexisting depression. Monitoring and treating serious depression is an important part of care for patients with cancer. [7]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Malignant melanoma can be diagnosed through various tests, such as biopsy and diagnostic imaging.
There are numerous methods used to perform skin biopsies. Physicians will select the most appropriate method based on location and size of the cancerous area, as well as other factors. Types of biopsies include:
- Shave (tangential) biopsy: The top layer of the skin is shaved off with a small surgical blade. Useful when the risk of melanoma is very low. Generally not used if melanoma is strongly suspected because the sample may not be thick enough to measure how deeply the cancer has invaded the skin.[4]
- Punch biopsy: A punch biopsy removes a deep sample of skin, including the dermis, epidermis, and subcutaneous tissues.[4]
- Incisional biopsy: An incisional biopsy removes a portion of a tumor that has invaded the deeper layers of the skin.[4]
- Excisional biopsy: An excisional biopsy removes an entire cancerous tumor that has invaded the deeper layers of the skin. It is the desired method of biopsy for potential melanomas.[4]
- “Optical” biopsy: New methods have been developed that don’t require removal of a skin sample. An example is Reflectance Confocal Microscopy (RCM).[4]
- Fine Needle Aspiration (FNA) biopsy: An FNA biopsy is used to biopsy enlarged, neighboring lymph nodes when a metastasis is suspected.[4]
- Surgical (excisional) Lymph Node biopsy: A surgical lymph node biopsy is used to remove an entire enlarged lymph node when a metastasis is suspected.[4]
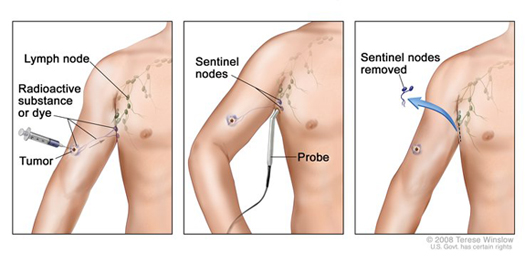
- Sentinel Lymph Node biopsy: A sentinel lymph node biopsy is used to determine lymph nodes that may be the first affected areas if the melanoma metastasizes. This is often performed after melanoma has been diagnosed and the cancer exhibits certain characteristics, such as an abnormal thickness.[4]
After the biopsy is performed, lab testing may be used to determine if melanoma cells are present in the tissue sample via testing such as immunohistochemistry (IHC), fluorescence in situ hybridization (FISH), and comparative genomic hybridization (CGH).[4]
Diagnostic imaging may be used to determine possible areas of metastasis. Imaging tests include:
- Chest X-Ray: A chest x-ray may be used to identify potential lung metastasis.[4]
- Computed Tomography (CT) scan: A CT scan can be helpful in locating enlarged lymph nodes or determining if other organs, such as lungs or liver, contain cancerous cells.[4]
- Magnetic Resonance Imaging (MRI) scan: An MRI provides similar information as a CT scan, but is often used when looking at the brain and spinal cord.[4]
- Positron Emission Tomography (PET) scan: A PET scan is typically used for individuals with advanced melanoma to determine if the cancer has metastasized to lymph nodes or other organs.[4]
Systemic Involvement[edit | edit source]
The most common sites of distant metastases include the lungs, lymph nodes, brain, and surrounding visceral pleura.
- Lungs: The earliest symptoms of pulmonary metastases are often dyspnea or pleural pain. Patient may report and increase in symptoms with deep breathing or physical activity. Patients may also experience a cough with bloody or rust colored sputum. Pleural pain may not be experienced until tumor cells have expanded to reach the pain fibers in the parietal pleura. [8]
- Lymph nodes: With metastases to lymph tissue, patients may have enlarged palpable lymph nodes. They may also report other symptoms such as fever, night sweats, weight loss, or infection. [8]
- Brain: Up to two thirds of patients with metastatic malignant melanoma will have brain metastases and one third will have metastases to the meninges. Brain metastases can produce a wide variety of signs and symptoms depending on the size and location of the lesion. [9]However, some of the most common symptoms include headache, vomiting, personality change, and seizures. Brain tumors may also result in paraneoplastic syndrome. This syndrome can cause unusual symptoms that occur in areas far from the site of metastases. [8]
Individuals who are diagnosed with malignant melanoma often have to undergo conventional cancer treatments such as chemotherapy. These treatments are cytotoxic and nonspecific, destroying all types of rapidly dividing cells including bone marrow, hair follicles, and mucosal cells in the mouth, digestive system, and reproductive system. Cancer treatment can result in numerous physical side effects including:[8]
- bone marrow suppression (leukopenia, anemia, thrombocytopenia)
- mouth sores
- nausea/vomiting
- easy bruising or bleeding
- fatigue
- loss of hair
Late effects may persist after cessation of treatment and may include:[8]
- lymphedema
- osteoporosis
- reproductive/hormonal changes
- muscle shortening and loss of muscle activity
Medical Management[edit | edit source]
Five types of standard treatment are used to treat patients with malignant melanoma[10]:
- Surgery: Surgical removal of the tumor is the primary treatment for all stages of melanoma. Wide, local excision is used to remove the melanoma as well as some of the normal tissue surrounding it. Skin grafting may be needed to cover the wound. If the cancer has spread to the lymph nodes, a lymphadenectomy may be performed to remove cancerous cells.
- Chemotherapy: Chemotherapy uses drugs to stop cancer cell growth either by killing the cells or by stopping them from dividing. Systemic chemotherapy is when the drugs enter the bloodstream by mouth or injection. Regional chemotherapy is when drugs are placed directly into the cerebrospinal fluid, organ, or body cavity.
- Radiation Therapy: Radiation therapy uses radiation to kill cancer cells or stop them from growing. External radiation therapy uses a machine to send radiation towards the cancer. Internal radiation therapy uses needles, seeds, wires, or catheters filled with a radioactive substance and are placed directly into or near the cancer.
- Immunotherapy: Immunotherapy uses the immune system to fight cancer. This is also called biotherapy. Substances made by the body or in a laboratory are used to boost direct or restore the body’s natural defenses against cancer. These may be delivered intravenously, topically, or orally.
- Targeted Therapy: Targeted therapy uses drugs or other substances to attack cancer cells and usually cause less harm to normal cells than chemotherapy or radiation therapy. Types of targeted therapy include signal transduction inhibitor therapy, oncolytic virus therapy, and angiogenesis inhibitors.
If detected early, conservative treatments such as immunotherapy can be used. If conservative treatment fails, surgical excision may be indicated. Surgery may also be used as the initial treatment if the tumor is small and localized.[4]
If melanoma has metastasized to distant organs, it may be impossible to excise all of the cancerous cells during surgery. In this case, chemotherapy may be used to treat the cancer. Chemotherapy is typically not as effective in curing melanoma as it is in other cancer types; however, it may reduce symptoms or decrease mortality. Recent research suggests that combining chemotherapy with immunotherapy drugs, such as interferons or interleukins, may be more effective than chemotherapy alone. This combination is known as biochemotherapy or chemoimmunotherapy.[11] Other combinations, such as chemotherapy with bone marrow transplantation, have also been studied. Research has shown that initial response to this treatment is positive, but generally lasts for less than six months.[12]
Physical Therapy Management[edit | edit source]
Physical Therapists should be aware of potential signs of skin cancer when evaluating patients. Therapists should look for abnormal spots, particularly areas that are exposed to the sun, or any of the ABCDE warning signs. If any abnormal findings are observed, the patient should be referred to their primary care physician for further testing. [3]
Physical Therapists can play an integral role in treating or managing side effects of melanoma treatments. This can include minimizing lymphedema, wound management, and pain control. Therapists may also work with these patients to address symptoms from conventional cancer treatments such as fatigue, muscle weakness, and atrophy. [3]
Physical Therapists should also be aware of contraindications to aerobic exercise for chemotherapy patients. Therapists should monitor vital signs and RPE during exercise. Observation for signs of infection, thrombocytopenia, DVT, dehydration, and electrolyte balance is also recommended. [8]
| Platelet count | <50,000/mm3 |
| Hemoglobin | <10 g/dL |
| WBC count | <3,000/mm3 |
| Absolute granulocytes | <2,500/mm3 |
Physical therapists have the training and skills to effectively manage cancer related treatment effects. Evidence supports the efficacy of aerobic training and strengthening exercises for preventing and managing cancer related fatigue and deconditioning during and after cancer treatment.[13]
Differential Diagnosis[edit | edit source]
The following differential diagnoses should be considered:[9]
- Atypical Mole (Clark Nevus or Dysplastic Nevus)
- Basal Cell Carcinoma
- Blue Nevi
- Cherry Hemangioma
- Cutaneous Squamous Cell Carcinoma
- Dermatofibroma
- Halo nevus
- Keloid and Hypertrophic Scar
- Keratoacanthoma
- Lentigo
- Melanocytic Nevi
- Seborrheic Keratosis
- Spitz Nevi
- Vitiligo
- Mycosis Fungoides
- Benign Melanocytic Lesions
- Sebaceous Carcinoma
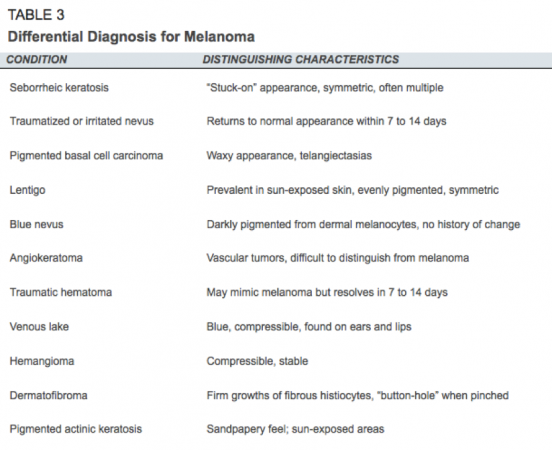
Table 3, below, may also be useful in helping the healthcare provider differentiate between diagnoses.
Table 3: Differential Diagnosis for Melanoma. American Family Physician 2001.
Case Reports/ Case Studies[edit | edit source]
An Unusual Case of Desmoplastic Malignant Melanoma
Clinical and Pathological Analysis of Two Cases of Cutaneous Malignant Melanoma
Malignant Melanoma- A Case Report with Literature Review
A Case Report of Primary Recurrent Malignant Melanoma of the Urinary Bladder
In situ malignant melanoma on nevus spilus in an elderly patient
Primary malignant melanoma of the esophagus: A case report
Resources[edit | edit source]
National Cancer Institute: Melanoma: www.cancer.gov/cancertopics/types/melanoma
American Cancer Society: Melanoma Skin Cancer: www.cancer.org/%20cancer/skincancer-melanoma/index
Skin Cancer Foundation: Melanoma: www.skincancer.org/skin-cancer-information/melanoma
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 Radiopedia Malignant melanoma Available from:https://radiopaedia.org/articles/metastatic-melanoma?lang=gb (last accessed 3.9.2020)
- ↑ 2.0 2.1 2.2 2.3 2.4 Heistein JB, Acharya U. Cancer, Malignant Melanoma. InStatPearls [Internet] 2019 Mar 12. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK470409/ (last accessed 3.9.2020)
- ↑ 3.0 3.1 3.2 Goodman CC, Fuller KS. The Integumentary System. In: Pathology Implications for the Physical Therapist. 3rd ed. St. Louis, MO: Saunders Elsevier; 2009: 392-452.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 Melanoma Skin Cancer. American Cancer Society. Available at http://www.cancer.org/cancer/skincancer-melanoma/index. Accessed March 17, 2014.
- ↑ Alappattu M, Coronado R, Lee D, Bour B, George S. Clinical characteristics of patients with cancer referred for outpatient physical therapy. Physical Therapy [serial on the Internet]. (2015, Apr), [cited April 5, 2017]; 95(4): 526-538. Available from: MEDLINE.
- ↑ A F Grann, T Frøslev, A B Olesen, H Schmidt, T L Lash. The impact of comorbidity and stage on prognosis of Danish melanoma patients, 1987–2009: a registry-based cohort study [Internet]. British Journal of Cancer. 2013. p. 265–71. Available from: http://www.nature.com/bjc/journal/v109/n1/full/bjc2013246a.html
- ↑ 7.0 7.1 FDA Approved Drugs for Melanoma [Internet]. AIM at Melanoma. [cited 2017Apr3]. Available from: https://www.aimatmelanoma.org/melanoma-treatment-options/fda-approved-drugs-for-melanoma/
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Goodman CC, Snyder TE. Screening for Cancer. In: Differential Diagnosis for Physical Therapists, Screening for Referral. W B Saunders Company; 2012: 487-543.
- ↑ 9.0 9.1 Secondary CNS Melanomas. Medscape. Available at: http://emedicine.medscape.com/article/1158059-overview. Accessed on: April 4, 2017.
- ↑ Melanoma Treatment [Internet]. National Cancer Institute. [cited 2017Apr3]. Available from: https://www.cancer.gov/types/skin/patient/melanoma-treatment-pdq
- ↑ Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364(26):2517-26.
- ↑ Ho, R. C. S. (1995), Medical management of stage IV malignant melanoma. Medical issues. Cancer, 75: 735–741. doi: 10.1002/1097-0142(19950115)75:2+<735::AID-CNCR2820751418>3.0.CO;2-Q
- ↑ The role of physical therapy in cancer [Internet]. World Physical Therapy Day. World Confederation for Physical Therapy; 2011 [cited 2017Apr4]. Available from: http://www.wcpt.org/sites/wcpt.org/files/files/WPTDay11_Cancer_Fact_sheet_C6.pdf