Malignant Melanoma
Original Editors - Emily Erwin & Brooke Sowards from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Erwin, Brooke Sowards, Ellen Hosking, Lucinda hampton, Elaine Lonnemann, Kim Jackson, Vidya Acharya, Wendy Walker, Calli Paydo, WikiSysop and 127.0.0.1
Introduction[edit | edit source]
Definition/Description
[edit | edit source]
Malignant Melanoma is a cancer that begins in a specific type of skin cells known as melanocytes. This type of cancer may also be known as melanoma or cutaneous melanoma.
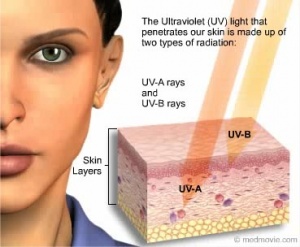
Melanocytes are located in the most superficial layer of skin, the epidermis. The epidermis protects the underlying dermis and subcutaneous tissue layers of the skin. Melanocytes are found in the basal layer, or the lowest layer, of the epidermis. These cells produce a brown pigment known as melanin, which gives the skin its tan appearance. After sun exposure, additional melanin is produced, resulting in a darkening or "tanning" of the skin. Melanin also plays an integral role in preventing skin damage from the sun's harmful rays. [1]
Malignant growths may occur following damage to skin cell DNA. If unrepaired, this damage initiates mutations that result in rapid proliferation of skin cells that form malignant tumors.[2] Malignant melanoma can occur anywhere on the body, but occurs more often in skin routinely exposed to sunlight such as the face, neck, hands, and arms. [3]
Prevalence/Risk Factors
[edit | edit source]
Compared to other cancers, melanoma of the skin is fairly common and represents 4.5% of all new cancer cases in the U.S. Although Malignant Melanoma accounts for less than 2% of total skin cancer cases, it causes a much larger percentage of skin cancer deaths. The American Cancer Society predicts for melanoma in the United States for 2017:
- Approximately 87,110 new melanomas will be diagnosed (52,170 in men and 34,940 in women)[1]
- Aproximately 9,730 people are expected to die of melanoma (6,380 men and 3,350 women)[1]
- The rate of melanoma have been rising for the last 30 years. [1]
Overall, melanoma is more common in men than women. However, before the age of 40 the risk is higher for women and after the age of 40 the risk is higher for men. The average age of diagnosis is 63. Although it is more likely to occur in the older population, it is one of the most common cancers in young individuals, particularly women under the age 30. [1]
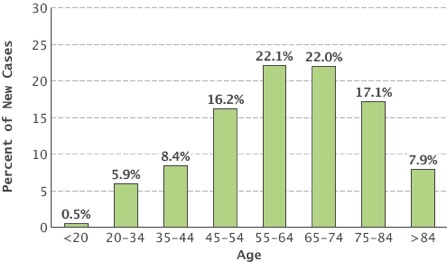
Percent of new cases by age group. SEER 2009-2013.
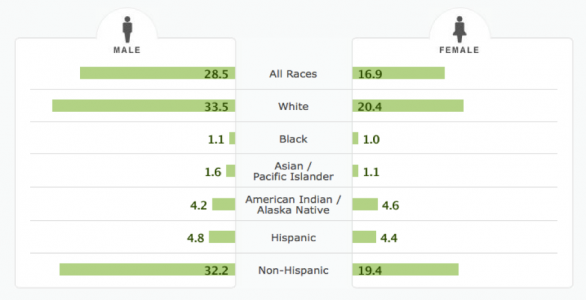
The incidence of new cases is higher among whites than any other racial/ethnic group. Overall, the lifetime risk of getting melanoma is about 2.5% (1 in 40) for whites, 0.1% (1 in 1000) for blacks and 0.5% (1 in 200) for Hispanics. [1]
Number of new cases per 100,000 persons by race/ethnicity and sex. SEER 2009-2013.
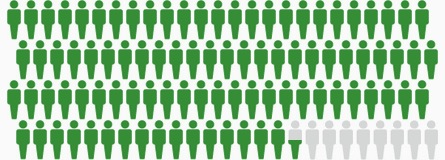
The five year survival rate for individuals diagnosed with malignant melanoma is 91.5%. Survival rate is closely related to cancer stage at the time of diagnosis. Typically, an earlier diagnosis is associated with a higher chance of survival. Additionally, localized melanomas have better outcomes than metastatic melanoma. The five year survival rate for localized melanoma is 98.4%.[4]
5-Year Survival for Malignant Melanoma. Green figures: survived 5 years or more. Gray figures: died from melanoma.
SEER 2006-2012.
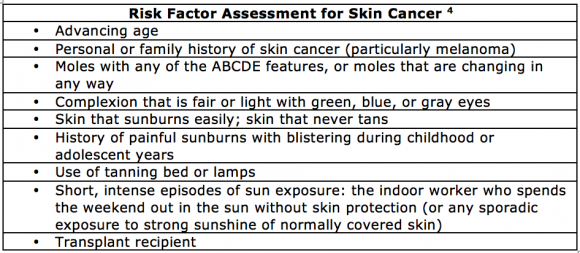
Individuals who have blonde or red hair color, fair skin, or light eyes are at an increased risk for developing melanoma. These individuals are at an increased risk because fair skin typically sunburns more easily. This population is believed to have a variation in the MC1R gene, which assists in making melanin to help protect the skin against harmful UV rays. [5]
Characteristics/Clinical Presentation[edit | edit source]
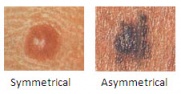
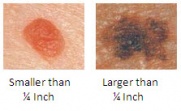
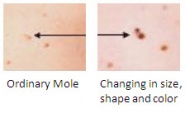
The most common early indication of malignant melanoma is often the presence of an abnormal mole. There are five specific characteristics that can help you identify whether a mole is cancerous or not. Health care professionals may educate patients on the “ABCDE” warning signs of melanoma. Research with digital imaging has confirmed that the ABCDE warning signs have a sensitivity ranging from 57% to 90% and a specificity from 59% to 90%.[6]
A = Asymmetry; uneven edges, lopsided in shape, one half unlike the other half. If you draw a line through the asymmetrical mole, the two halves will not match. [2][6]
B = Border; irregularity, irregular edges, scalloped, notched, or poorly defined edges[2][6]
C = Color; black, shades of brown, red, white, occasionally blue. Having multiple colors present is also an abnormal finding.[2][6]
D = Diameter; larger than a pencil eraser (1/4 in or 6 mm)[2][6]
E = Evolving; mole or skin lesion that looks different from the rest, or is changing in size, shape, or color. Other changes, such as bleeding, itching, or crusting, may also occur.[2][6]
However, some melanomas don’t fit these guidelines. Therefore, it is important to be aware of other warning signs including[1]:
• A sore that doesn’t heal
• Spread of pigment from the border of a spot into surrounding skin
• Redness or a new swelling beyond the border of the mole
• Change in sensation, such as itchiness, tenderness, or pain
• Change in the surface of a mole, such as scaliness, oozing, bleeding, or the appearance of a lump or bump
Staging of Melanoma[edit | edit source]
There are three common methods used when staging the severity of malignant melanoma.
The Breslow method determines stage based on the thickness of the melanoma. It is considered one of the important factors in predicting the disease progression. Typically, thin tumors have a very small chance of metastasizing and a better prognosis.[7]
- Thin Tumors: Less than 1.0 mm in depth
- Intermediate Tumors: 1.0-4.0 mm in depth
- Thick Tumors: Greater than 4.0 mm in depth[2]
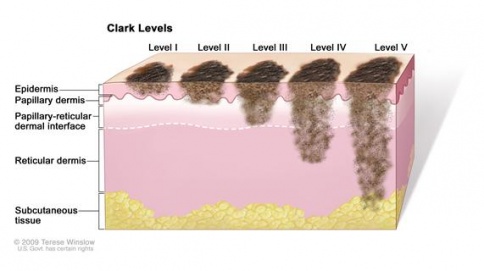
Clark's levels determine melanoma staging by assessing the levels of skin that are affected.
- Level 1: Found only in the epidermis; "in situ" melanoma
- Level 2: Progression into the papillary dermis
- Level 3: Throughout the entire papillary dermis
- Level 4: Progression into the reticular dermis
- Level 5: Progression into the subcutaneous tissue[7]
TNM staging combines the Breslow method and Clark's levels. This staging system is most often used for melanoma.
- T (Tumor): Primary, localized melanoma.
- N (Lymph Nodes): Regional metastasis to lymph nodes
- M (Distant Metastasis): Distant metastasis throughout the body[7][1]
Associated Comorbidities
[edit | edit source]
Individuals who have been diagnosed with dysplastic nevus syndrome often develop malignant melanoma later in life. This syndrome, also known as atypical mole syndrome, is a familial disorder that results in a significant number of large moles that have an irregular shape or color. They frequently appear on skin that is exposed to the sun but can develop anywhere on the body. The dysplastic nevi have up to a 50% chance of developing into malignant melanoma; therefore, they are often surgically removed to prevent cancer. Individuals with this syndrome are encouraged to have routine skin exams by a dermatologist and should preform monthly self-skin exams. [7][1]
There are no specific comorbidities that are closely linked to malignant melanoma. Comorbidities commonly reported in patients with cancer are hypertension, diabetes, arthritis, heart disease, and upper gastrointestinal disease. [8] Research has shown an association between comorbidities such as these with delay of melanoma diagnosis, more advanced stages of melanoma, and less aggressive treatments. Therefore, improved efforts to treat these comorbidities may result in decreased mortality rates among individuals with melanoma.[9]
Medications[edit | edit source]
Common FDA approved medications for the treatment of malignant melanoma are divided into three categories and listed below. [10]
Immunotherapies:
- Imlygic (talimogene laherparepvec "t-vec")
- Intron A (high-dose interferon alfa-2b)
- Keytruda (pembrolizumab)
- Opdivo (nivolumab)
- Opdivo (nivolumab) and Yervoy (ipilimumab) combination
- Proleukin / il-2 (interleukin-2)
- Sylatron (peginterferon alfa-2b)
- Yervoy (ipilimumab)
Targeted Therapies:
- Cotellic (cobimetinib) and Zelboraf (vemurafenib) combination
- Mekinist (trametinib)
- Mekinist (trametinib) and Tafinlar (dabrafenib) combination
- Tafinlar (dabrafenib)
- Zelboraf (vemurafenib)
Chemotherapy
- DTIC (dacarbazine)
Common side effects that may be experienced while undergoing cancer treatment include flu-like symptoms, fatigue, nausea, changes in taste and smell, loss of appetite, and depression. Flu-like symptoms may include fever, chills, headache, and muscle aches. These symptoms are more common in those receiving immunotherapy. Those receiving immunotherapy, chemotherapy, and radiation therapy often experience a feeling of intense tiredness or weakness not usually relieved with rest or sleep. Nausea can be a problematic side-effect not only because of the discomfort it causes, but it can also prevent proper nutrition. It is common in immunotherapy. Loss of appetite commonly results with immunotherapy, targeted therapy, chemotherapy and radiation therapy. Loss of appetite may be due to nausea, vomiting, depression, or changes in one’s taste or smell. Medications used to treat melanoma may induce depression or worsen preexisting depression. Monitoring and treating serious depression is an important part of care for patients with cancer. [10]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Malignant melanoma can be diagnosed through various tests, such as biopsy and diagnostic imaging.
There are numerous methods used to perform skin biopsies. Physicians will select the most appropriate method based on location and size of the cancerous area, as well as other factors. Types of biopsies include:
- Punch biopsy: A punch biopsy removes a deep sample of skin, including the dermis, epidermis, and subcutaneous tissues.[1]
- Incisional biopsy: An incisional biopsy removes a portion of a tumor that has invaded the deeper layers of the skin.[1]
- Excisional biopsy: An excisional biopsy removes an entire cancerous tumor that has invaded the deeper layers of the skin. It is the desired method of biopsy for potential melanomas.[1]
- Fine Needle Aspiration (FNA) biopsy: An FNA biopsy is used to biopsy enlarged, neighboring lymph nodes when a metastasis is suspected.[1]
- Surgical (excisional) Lymph Node biopsy: A surgical lymph node biopsy is used to remove an entire enlarged lymph node when a metastasis is suspected.[1]
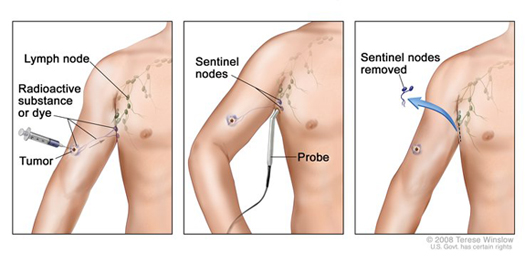
- Sentinel Lymph Node biopsy: A sentinel lymph node biopsy is used to determine lymph nodes that may be the first affected areas if the melanoma metastasizes. This is often performed after melanoma has been diagnosed and the cancer exhibits certain characteristics, such as an abnormal thickness.[1]
After the biopsy is performed, lab testing may be used to determine if melanoma cells are present in the tissue sample via testing such as immunohistochemistry (IHC), fluorescence in situ hybridization (FISH), and comparative genomic hybridization (CGH).[1]
Diagnostic imaging may be used to determine possible areas of metastasis. Imaging tests include:
- Chest X-Ray: A chest x-ray may be used to identify potential lung metastasis.[1]
- Computed Tomography (CT) scan: A CT scan can be helpful in locating enlarged lymph nodes or determining if other organs, such as lungs or liver, contain cancerous cells.[1]
- Magnetic Resonance Imaging (MRI) scan: An MRI provides similar information as a CT scan, but is often used when looking at the brain and spinal cord.[1]
- Positron Emission Tomography (PET) scan: A PET scan is typically used for individuals with advanced melanoma to determine if the cancer has metastasized to lymph nodes or other organs.[1]
Etiology/Cause
[edit | edit source]
Individuals who have blonde or red hair color, fair skin, or light eyes are at an increased risk for developing melanoma. These individuals are at an increased risk because fair skin typically sunburns more easily. This population is believed to have a variation in the MC1R gene, which assists in making melanin to help protect the skin against harmful UV rays. [7]
Another major risk factor for developing melanoma is the excessive exposure to UV radiation through sunlight and tanning booths. There are three types of UV rays; UVA, UVB, UVC. UVA and UVB, which are found in sunlight and tanning booths, cause damage to skin cell DNA which promotes the development of melanoma. This unrepaired DNA damage can lead to rapid cell division and genetic mutations that cause cancer.[2] UVC rays are not found in sunlight therefore are not damaging or associated with melanoma. [1]
An individual’s risk of developing melanoma is greater if an immediate relatives such as a parent, brother, sister, or child, has had melanoma. Around 10% of all people with melanoma report a positive family history of the disease. This increased risk could be associated with a similar lifestyle of frequent sun exposure, a common characteristic of fair skin, or a combination of factors. It may also be caused by gene mutations that are hereditary. In families that have a high rate of melanoma, up to 40% have a known gene mutation.[1]
Systemic Involvement[edit | edit source]
The most common sites of distant metastases include the lungs, lymph nodes, brain, and surrounding visceral pleura.
- Lungs: The earliest symptoms of pulmonary metastases are often dyspnea or pleural pain. Patient may report and increase in symptoms with deep breathing or physical activity. Patients may also experience a cough with bloody or rust colored sputum. Pleural pain may not be experienced until tumor cells have expanded to reach the pain fibers in the parietal pleura. [6]
- Lymph nodes: With metastases to lymph tissue, patients may have enlarged palpable lymph nodes. They may also report other symptoms such as fever, night sweats, weight loss, or infection. [6]
- Brain: Up to two thirds of patients with metastatic malignant melanoma will have brain metastases and one third will have metastases to the meninges. Brain metastases can produce a wide variety of signs and symptoms depending on the size and location of the lesion. [11] However, some of the most common symptoms include headache, vomiting, personality change, and seizures. Brain tumors may also result in paraneoplastic syndrome. This syndrome can cause unusual symptoms that occur in areas far from the site of metastases. [6]
Individuals who are diagnosed with malignant melanoma often have to undergo conventional cancer treatments such as chemotherapy. These treatments are cytotoxic and nonspecific, destroying all types of rapidly dividing cells including bone marrow, hair follicles, and mucosal cells in the mouth, digestive system, and reproductive system. Cancer treatment can result in numerous physical side effects including:[6]
- bone marrow suppression (leukopenia, anemia, thrombocytopenia)
- mouth sores
- nausea/vomiting
- easy bruising or bleeding
- fatigue
- loss of hair
Late effects may persist after cessation of treatment and may include:[6]
- lymphedema
- osteoporosis
- reproductive/hormonal changes
- muscle shortening and loss of muscle activity
Medical Management (current best evidence)[edit | edit source]
If detected early, conservative treatments such as immunotherapy can be used. This involves the use of medications to improve the immune system's ability to recognize and destroy cancer cells. Immunotherapy may be delivered intravenously, topically, or orally.
If conservative treatment fails, surgical excision may be indicated. Surgery may also be used as the initial treatment if the tumor is small and localized. With surgical excision, the entire tumor may be successfully removed. If the melanoma has metastasized to nearby lymph nodes, the surgeon may elect to remove the lymph nodes as well.[1]
If melanoma has metastasized to distant organs, it may be impossible to excise all of the cancerous cells during surgery. In this case, chemotherapy may be used to treat the cancer. Chemotherapy is typically not as effective in curing melanoma as it is in other cancer types; however, it may reduce symptoms or decrease mortality. Recent research suggests that combining chemotherapy with immunotherapy drugs, such as interferons or interleukins, may be more effective than chemotherapy alone. This combination is known as biochemotherapy or chemoimmunotherapy.[12] Other combinations, such as chemotherapy with bone marrow transplantation, have also been studied. Research has shown that initial response to this treatment is positive, but generally lasts for less than six months.[13]
Physical Therapy Management (current best evidence)[edit | edit source]
Physical Therapists should be aware of potential signs of skin cancer when evaluating patients. Therapists should look for abnormal spots, particularly areas that are exposed to the sun, or any of the ABCDE warning signs. If any abnormal findings are observed, the patient should be referred to their primary care physician for further testing. [7]
Physical Therapists can play an integral role in treating or managing side effects of melanoma treatments. This can include minimizing lymphedema, wound management, and pain control. Therapists may also work with these patients to address symptoms from conventional cancer treatments such as fatigue, muscle weakness, and atrophy. [7]
Physical Therapists should also be aware of contraindications to aerobic exercise for chemotherapy patients. Therapists should monitor vital signs and RPE during exercise. Observation for signs of infection, thrombocytopenia, DVT, dehydration, and electrolyte balance is also recommended. [6]
| Platelet count | <50,000/mm3 |
| Hemoglobin | <10 g/dL |
| WBC count | <3,000/mm3 |
| Absolute granulocytes | <2,500/mm3 |
Differential Diagnosis[edit | edit source]
The following differential diagnoses should be considered[14]
- Basal Cell Carcinoma
- Squamous Cell Carcinoma
- Mycosis Fungoides
- Benign Melanocytic Lesions
- Dysplastic Nevus Syndrome
- Sebaceous Carcinoma
- Pigmented Actinic Keratosis
Case Reports/ Case Studies[edit | edit source]
A Case Report of Primary Recurrent Malignant Melanoma of the Urinary Bladder
In situ malignant melanoma on nevus spilus in an elderly patient
Primary malignant melanoma of the esophagus: A case report
Resources
[edit | edit source]
National Cancer Institute: Melanoma: www.cancer.gov/cancertopics/types/melanoma
American Cancer Society: Melanoma Skin Cancer: www.cancer.org/%20cancer/skincancer-melanoma/index
Skin Cancer Foundation: Melanoma: www.skincancer.org/skin-cancer-information/melanoma
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1fGBqCW25OtBvPIBGxBnWFIuy00YvVL5_Jd_jNdAB93qeBDMV8|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 Melanoma Skin Cancer. American Cancer Society. Available at http://www.cancer.org/cancer/skincancer-melanoma/index. Accessed March 17, 2014.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Melanoma. Skin Cancer Foundation. Available at www.skincancer.org/skin-cancer-information/melanoma. Accessed March 17, 2014.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedSeer - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedSEER - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedGoodman - ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 Goodman CC, Snyder TE. Screening for Cancer. In: Differential Diagnosis for Physical Therapists, Screening for Referral. W B Saunders Company; 2012: 487-543.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Goodman CC, Fuller KS. The Integumentary System. In: Pathology Implications for the Physical Therapist. 3rd ed. St. Louis, MO: Saunders Elsevier; 2009: 392-452.
- ↑ Alappattu M, Coronado R, Lee D, Bour B, George S. Clinical characteristics of patients with cancer referred for outpatient physical therapy. Physical Therapy [serial on the Internet]. (2015, Apr), [cited April 5, 2017]; 95(4): 526-538. Available from: MEDLINE.
- ↑ A F Grann, T Frøslev, A B Olesen, H Schmidt, T L Lash. The impact of comorbidity and stage on prognosis of Danish melanoma patients, 1987–2009: a registry-based cohort study [Internet]. British Journal of Cancer. 2013. p. 265–71. Available from: http://www.nature.com/bjc/journal/v109/n1/full/bjc2013246a.html
- ↑ 10.0 10.1 FDA Approved Drugs for Melanoma [Internet]. AIM at Melanoma. [cited 2017Apr3]. Available from: https://www.aimatmelanoma.org/melanoma-treatment-options/fda-approved-drugs-for-melanoma/
- ↑ Secondary CNS Melanomas. Medscape. Available at: http://emedicine.medscape.com/article/1158059-overview. Accessed on: March 19, 2014.
- ↑ Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364(26):2517-26.
- ↑ Ho, R. C. S. (1995), Medical management of stage IV malignant melanoma. Medical issues. Cancer, 75: 735–741. doi: 10.1002/1097-0142(19950115)75:2+&amp;amp;amp;amp;amp;lt;735::AID-CNCR2820751418&amp;amp;amp;amp;amp;gt;3.0.CO;2-Q
- ↑ Malignant Melanoma Differential Diagnosis. Medscape. Available at http://emedicine.medscape.com/article/280245-differential. Accessed March 18, 2014.