Osteoporotic Vertebral Fractures: Difference between revisions
No edit summary |
No edit summary |
||
| Line 29: | Line 29: | ||
[[Image:Vertebral Fracture.png|right|250x350px|Vertebral Fracture]] | [[Image:Vertebral Fracture.png|right|250x350px|Vertebral Fracture]] | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
Due to the osteoporosis that made the bone density low and made the bone weak (higher activity of osteoclasts and lower activity of osteoblasts), the vertebra can ‘collapse’. This is called a vertebral body fracture. The fracture can lead to hyperkyphosis or hyperlordosis depending on the vertebral level. People with osteoporosis break down bone faster than it can regenerate. Trabecular bone is more active and because of this, trabecular bone is more likely to be affected. When people stand up causing pressure on the spine, the weak trabecular bone of the spine body’s can start to collapse, leading to an osteoporotic vertebral fracture. <span style="line-height: 1.5em;">This fracture occur on the posterior part of the vertebra or the vertebral body. Because of the decrease of height of the vertebra, the ligamentum logitudinale anterius and posterius loses tension. This can cause vertebral instability.</span> | |||
[[Image:Afb_osteo_2.png|400x400px]][[Image:Afb_osteo_1.png|right]] | |||
== Epidemiology / Etiology == | == Epidemiology / Etiology == | ||
Revision as of 23:10, 14 June 2016
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Mathieu Vanderroost, Angeliki Chorti, Lucinda hampton, Jasper Vermeersch, Jon Room, Kim Jackson, Jelle Van Hemelryck, Khloud Shreif, Laura Ritchie, Lauren Lopez, Vidya Acharya, 127.0.0.1, Admin, Rachael Lowe, Kai A. Sigel, WikiSysop and Claire Knott
Search Strategy[edit | edit source]
Databases: Pubmed, Web of Science, Pedro.
As subject headings varied between the databases, various combinations of the key words were used. These were the most productive: Osteoporotic Vertebral Fractures, Osteoporotic Vertebrae Fractures, Insufficiency Fractures, Vertebral Compression Fractures, Osteoporosis AND physical therapy, Osteoporosis AND diagnosis, Osteoporotic Vertebral Fractures AND treatment.
Definition / Description[edit | edit source]
Osteoporotic (fragility) fractures are fractures that result from mechanical forces that would not ordinarily result in a fracture, known as low-level (or low-energy) trauma according to National Institute for Health and Care Excellence (NICE) clinical guidelines. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Osteoporosis is a disease that is characterised by low bone mass,[1] causing bones to be more fragile and likely to fracture.[2] The word osteoporosis literally means porous bone.[3] One of the significant consequences of osteoporosis is fractures. Common types of fracture include wrist fractures, hip fractures and vertebral fractures.[1][4]
Osteoporosis in older adults is caused by an imbalance of bone resorption in excess of bone formation. The dominant factor leading to bone loss in older adults appears to be gonadal sex steroid deficiency, with multiple genetic and biochemical factors, such as Vitamin D Deficiency or hyperparathyroidism, that may accelerate bone loss.
Conditions that adversely affect growth and development may limit development of peak bone mass and accelerate subsequent bone loss. Studies of bone microarchitecture have shown that trabecular bone loss begins in the third decade of life, before gonadal sex steroid deficiency develops, whereas cortical loss typically begins in the sixth decade, about the time of menopause in women and about the same age in men.
Antiresorptive agents for the treatment of osteoporosis act primarily by limiting osteoclast activity, whereas osteoanabolic agents, such as teriparatide, act primarily by stimulating osteoblastic bone formation. Clinical investigation of new compounds for the treatment of osteoporosis is mainly directed to those that stimulate bone formation or differentially decrease bone resorption more than bone formation. Therapies for osteoporosis are associated with adverse effects, but in patients at high risk of fracture, the benefits generally far outweigh the risks.
Important: Bone mass alone does not explain the risk of fractures in at least 50% of osteoporosis cases; bone quality also plays a role. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
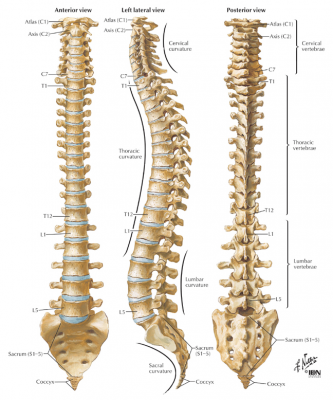
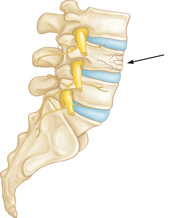
Clinically Relevant Anatomy[edit | edit source]
Due to the osteoporosis that made the bone density low and made the bone weak (higher activity of osteoclasts and lower activity of osteoblasts), the vertebra can ‘collapse’. This is called a vertebral body fracture. The fracture can lead to hyperkyphosis or hyperlordosis depending on the vertebral level. People with osteoporosis break down bone faster than it can regenerate. Trabecular bone is more active and because of this, trabecular bone is more likely to be affected. When people stand up causing pressure on the spine, the weak trabecular bone of the spine body’s can start to collapse, leading to an osteoporotic vertebral fracture. This fracture occur on the posterior part of the vertebra or the vertebral body. Because of the decrease of height of the vertebra, the ligamentum logitudinale anterius and posterius loses tension. This can cause vertebral instability.
Epidemiology / Etiology[edit | edit source]
Osteoporotic vertebral fractures are a significant problem. The number of vertebral fractures in the UK in 2010 was estimated to be 30,994, this number is expected to increase by 17.9% by 2020.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title In America 700,000 vertebral fractures occur within the population who have osteoporosis.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title In addition to this once a vertebral fracture has been sustained the risk of subsequent vertebral, hip or wrist fractures increase. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Osteoporosis affects up to 30% of women and 12% of men at some point in their lives. Two of the most important risk factors are increasing age and female gender, although other common and potentially modifiable risk factors include long-term corticosteroid therapy, chronic inflammatory disease, malabsorption and untreated premature menopause. [5]
There is a higher prevalence for osteoporotic vertebral fractures for elderly and females with equal frequency in both Caucasian and Asian women. One out of four postmenopausal women suffer osteoporotic vertebral fractures. Osteoporotic vertebral fractures are multiple in up to 20% of patients and affect more than 20% of those older than 50 years with slight female prevalence that markedly increases when they age above 80 years.[6]
Symptomatic osteoporotic vertebral fractures affect 1 in 6 women and 1 in 12 men during their lifetime. In Europe the annual incidence of osteoporotic vertebral fractures is 10.7 per thousand for women and 5.7 per thousand for men. Statistically, men got less osteoporotic fractures then women because men lose less bone density when they age. These figures may underestimate the actual size of the problem as most osteoporotic vertebral fractures go unreported and undiagnosed. With the prevalence of osteoporosis predicted to increase by 2021, a rise in associated fractures is also likely. The main causes and risk factors of fractures and vertebral fractures are a decay in bone density and previous fractures. [7][8]
Looking more closely to the specific regions of the spine and the prevalence of osteoporotic fractures, we can conclude that osteoporotic fractures in the toracic spine are mostly affected.
There is a prevalence of 2,4/1000 (age 35-44), 5,1/1000 (age 44-75), 29/1000 (age > 75) in the thoracic spine. (Corresponding figures for men: 5,2/1000, 15/1000, 28/1000)[9]
Characteristics / Clinical Presentation[edit | edit source]
Symptoms of vertebral fracture can include pain, curvature of the spine, height loss, difficulties with ADLs, loss of self-esteem related to changes in body shape, and in cases of severe kyphosis respiratory and gastrointestinal problems,Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title in addition to vertebral fractures being linked to mortality.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Differential Diagnosis[edit | edit source]
Diagnostic Procedures[edit | edit source]
Outcome Measures[edit | edit source]
Examination[edit | edit source]
Medical Management[edit | edit source]
Good quality evidence supports that several medications (e.g. bisphosphonates) for bone density reduce fracture risk. Never the less side effects vary among drugs. (Crandall CJ, 2014: LoE 1A) Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
At first, conservative treatment still is the method of choice. In case of resulting deformity, sintering and persistent pain vertebral cement augmentation techniques today are widely used.Treatment after vertebral fracture should include appropriate pain management and possibly bracing.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Forms of conservative treatment commonly used in these patients include bed rest, analgesic medication, physiotherapy and bracing. Vertebral fractures can also be treated surgically using vertebroplasty and kyphoplasty.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Percutaneous vertebroplasty (VP) began as a simple, low-cost procedure that aimed to provide pain relief for patients with vertebral compression fractures (VCF). Balloon kyphoplasty (KP) was introduced later, and was presented not only as a ‘‘pain killer,’’ but also as a deformity correction procedure. (Itshayek E et al., 2012. LoE 2A)Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Treatment after vertebral fracture should include appropriate pain management and possibly bracing.[10]
Vertebral fractures can also be treated surgically using vertebroplasty and kyphoplasty.[11][12]
In a vertebroplasty bone cement, usually polymethylmethacrylate (PMMA), is injected into the vertebral bone. In a kyphoplasty a balloon is inserted into the vertebral body, the balloon is inflated to attempt to re-establish normal height and posture, the balloon is remove and cement injected.
Physical Therapy Management[edit | edit source]
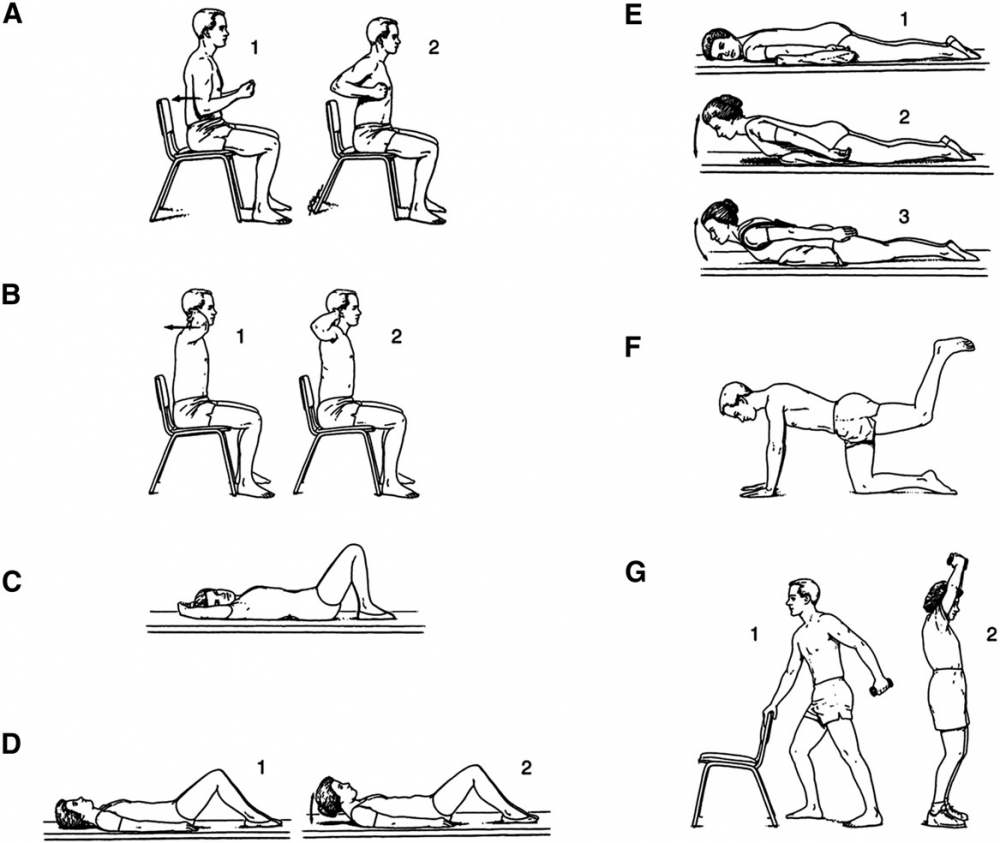
After a short period of bed rest patients should begin mobilisation with a rehabilitation and exercise program. The goals of rehabilitation are the prevention of falls, reduction of the kyphosis, enhancing axial muscle strength and providing correct spine alignment. (Yoo JH et al., 2015, LoE: 2B)[13]
Regarding Physiotherapy management, there are a number of treatment approaches, including strengthening exercise, stabilisation exercise, balance training, stretching, relaxation techniques, manual therapy and taping.[14][15] Currently a large RCT is comparing exercise based and ‘hands on’ manual therapy based physiotherapy against a control.[15]
Zehnacker and Bemis‐Dougherty conducted a systematic review to study the effect of weighted exercises on bone mineral density in post menopausal women. (2007, LoE: 1A)[16] Exercises such as walking has been shown to maintain or improve bone density in an osteoporotic population. Strengthening exercises, using weights or resistance bands, has also been shown to maintain or improve bone density at the location of the targeted muscle attachments. Maintaining bone health is extremely important, especially in the elderly as there typically is a decline in bone mass with age.
Strengthening and flexability exercises improve overall physical function and postural control. Improving postural control is important to reduce risk for falls. Falls often result in fractures in an osteoporotic population. Balance exercises are also important to further reduce the risk of falls. (Burke TN et al, 2012, LoE: 1B)[17]
Studies from De Kam et al. (2009, LoE:1A), Karinkanta et al. (2007, LoE:1B) and Hourigan SR et al. (2008, LoE:1B) all found that a combined balance and progressive strength training programme produced the best results in terms of maintaining leg strength, balance, bone mineral density and physical function compared to balance or strength training alone.[18][19][20]
Sinaki et al (2002, LoE: 3B) demonstrated that a spinal extensor strengthening programme and a dynamic proprioceptive programme increased bone density and reduced the risk of VCFs. Moreover the incidence of new fractures associated with back extension exercises is lower than the incidence related to abdominal flexion exercises (16% versus 89%).[21]
Exercise and exercise technique that focuses on spinal extension play an important role in reducing the risk of osteoporosis-related fractures. In addition, reports have shown that strenuous spinal flexion exercise, whether therapeutic, recreational, or job related, may induce compression fracture if beyond the biomechanical competence of the vertebral bodies. In other words, extreme flexion is contra-indicated. (LoE: 3A)[22]
Back extensor exercises improve muscle strength, providing a better dynamic-static posture and reduction of the kyphotic deformity. Correction of the kyphosis also results in pain relief, increased mobility and an improvement in the quality of life. (LoE: 3B)[23]
It has been previously hypothesized that horizontal nonloading back extension exercises from a prone position can decrease the incidence of vertebral fractures (LoE: 5).[24] Back extension exercises performed from the prone position load vertebral horizontal trabeculae without the risk of vertebral compression fracture that can occur with vertical loading. (LoE: 3A)[22]
Chen BL and colleagues studied the effectiveness of systematic back muscle exercises after vertebroplasty for spinal osteoporotic compression fractures. (2012, LoE: 1B) They found that systematic back muscle exercises resulted in a significant better outcome on the Oswestry Disability Index and pain level (VAS) compared to the control group. Control group only received general postoperation therapy without systematic back exercises.[25]
Wendlova J. (2011, LoE: 4) concludes after a biomechanical analysis that carrying a backpack on the back is recommended to patients with osteoporotic vertebral fractures. This is based upon removing the muscular dysbalance of the trunk muscles and upon increasing the bone strength by compressive force acting upon the vertebrae. Compressive forces activate osteoblasts to enhance osteoformation.The backpack load is differentiated: patients with vertebral fractures put a weight up to 1 kg into their backpacks, patients without vertebral fractures but diagnosed with osteoporosis increase the load up to 2kg. Further research is needed. [26]
To prevent falls and fractures, an exercise program should include balance and lower extremity strength training combined with a coordinated approach.(2012, LoE: 3A)[22]
Postural taping can help in maintaining postural alignment. Tape is applied to the skin to provide increased proprioceptive feedback about postural alignment, improve thoracic extension, reduce pain and facilitate postural muscle activity and balance. (Bautmans, 2012, LoE: 3B)[27]
Key Research[edit | edit source]
The following articles are key evidence pieces for physical therapy interventions:
- Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial. Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Positive effects of exercise on falls and fracture risk in osteopenic women.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study
- Identifying osteoporotic vertebral fracture. Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Position Statement of the Korean Society for Bone and Mineral Research.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Resources[edit | edit source]
www.nhs.uk/conditions/Osteoporosis/Pages/Introduction.aspx
www.nos.org.uk/about-osteoporosis
Clinical Bottom Line[edit | edit source]
Osteoporotic vertebral fractures are fractures of one ore more of the vertebrae due to osteoporosis. Osteoporosis causes the bones to be more fragile and more likely to fracture. Osteoporotic vertebral fractures classically occur during normal day-to-day activities such as bending, walking or lifting relatively light objects.
The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture. Chronic pain may also occur in patients with multiple compression fractures, height loss and low bone density. Although this is probably due to structural changes or osteoarthritis.
Vertebral fractures doesn’t only occur due to osteoporosis. Also a trauma or metastasis can cause a vertebral fracture. The diagnosis of osteoporosis can be confirmed by Dual Energy X-ray Absorptiometry (DXA).
Often used outcome measures to evaluate the progression of a patiënt are: Visual analogue scale for overall pain and pain during day and night (VAS), a Quality of Life questionnaire and a Physical functioning questionaire ( modified 23-item version of the Roland–Morris Disability Questionnaire).
Conservative treatment (bed rest, analgesic medication, physiotherapy and bracing) still is the method of choice as medical treatment. Vertebral fractures can also be treated surgically using vertebroplasty and kyphoplasty.
As physical therapy management there are a number of treatment approaches, including strengthening exercise, stabilisation exercise, balance training, stretching, relaxation techniques, manual therapy and taping.
Recent Related Research[edit | edit source]
- Rzewuska M. The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: a systematic review with meta-analysis.Eur Spine J. 2015 Apr;24(4):702-14. Level of Evidence: 1A.
- Buchbinder R, Golmohammadi K, Johnston RV, Owen RJ, Homik J, Jones A, Dhillon SS, Kallmes DF, Lambert RG.Percutaneous vertebroplasty for osteoporotic vertebral compression fracture.Cochrane Database Syst Rev. 2015 Apr 30;4:CD006349. Level of Evidence: 1A.
References[edit | edit source]
- ↑ 1.0 1.1 NICE. Osteoporosis: assessing the risk of fragility fracture: NICE Guidelines CG146. Manchester: National Institute for Health and Care Excellence, 2012.
- ↑ NOS. What is Osteoporosis? National Osteoporosis Society. https://www.nos.org.uk/about-osteoporosis (accessed 03/02/15)
- ↑ Ström O, Borgström F, Kanis JA, Compston J, Cooper C, McCloskey EV, Jönsson B. Osteoporosis: burden, health care provision and opportunities in the EU: A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 2011 6:59–155 DOI 10.1007/s11657-011-0060-1
- ↑ NHS. Osteoporosis. National Health Service. http://www.nhs.uk/conditions/Osteoporosis/Pages/Introduction.aspx (accessed 03/02/15)
- ↑ Ralston SH, Fraser J.Diagnosis and management of osteoporosis.Practitioner. 2015 Dec;259(1788):15-9, 2. (Level of Evidence: 3A)
- ↑ El-Fiki M. Vertebroplasty, Kyphoplasty, Lordoplasty, expandable devices and current treatment of painful osteoporoticvertebral fractures.World Neurosurg. 2016 Apr 9
- ↑ Steven R. Cummings et al. Epidemiology and outcomes of osteoporotic fractures. The Lancet. 2002
- ↑ Goodwin VA et al. Orthotics and taping in the management of vertebral fractures in people with osteoporosis: a systematic review. British Medical Journal.2016 (Level of Evidence 2A)
- ↑ Seppo Santavirta', Yrjo T. Konttinen*, Markku Heliovaara3, Paul Knekt3, Peter Luthje4 and Arpo Aromaa. Determinants of osteoporotic thoracic vertebral fracture, Acta Oflhop Scand 1992; 63 (2): 198-202 (LoE 2B)
- ↑ Gerdhem P. Osteoporosis and fragility fractures: Vertebral fractures. Best Practice &amp;amp;amp;amp;amp;amp;amp; Research Clinical Rheumatology 2013 27: 743–755
- ↑ Dionyssiotis Y. Management of osteoporotic vertebral fractures. Int J Gen Med. 2010 3: 167–171.
- ↑ NICE. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for treating osteoporotic vertebral compression fractures: NICE technology appraisal guidance TA279. Manchester: National Institute for Health and Care Excellence, 2013
- ↑ Yoo JH, Moon SH, Ha YC, Lee DY, Gong HS, Park SY, Yang KH.Osteoporotic Fracture: 2015 Position Statement of the Korean Society for Bone and Mineral Research.J Bone Metab. 2015 Nov;22(4):175-81. 30. (Level of Evidence: 2B)
- ↑ Pratelli E, Cinotti I, Pasquetti P. Rehabilitation in osteoporotic vertebral fractures. Clin Cases Miner Bone Metab. 2010 7(1): 45–47.
- ↑ 15.0 15.1 Barker K, Javaid MK, Newman M, Minns Lowe C, Stallard N, Campbell H, Gandhi V, Lamb S. Physiotherapy Rehabilitation for Osteoporotic Vertebral Fracture (PROVE): study protocol for a randomised controlled trial. Trials 2014 15:22
- ↑ Zehnacker CH, Bemis‐Dougherty A. Effect of Weighted Exercises on Bone Mineral Density in Post Menopausal Women A Systematic Review. Journal of Geriatric Physical Therapy. 2007; 30(2):79-88. (Level of Evidence: 1A)
- ↑ Burke TN, Franca FJR, Ferreira de Meneses SR, Pereira RMR, Marques AP. Postural control in elderly women with osteoporosis: comparison of balance, strengthening and stretching exercises. A randomized controlled trial. Clinical Rehabilitation; 26 (11): 1021-1031. 2012. (Level of Evidence: 1B)
- ↑ De Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BCM. Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Osteoporos Int. 2009;20:2111–2125 (Level of evidence: 1A)
- ↑ Karinkanta S, Heinonen A, Sievänen H, Uusi-Rasi K, Pasanen M, Ojala K. A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial. Osteoporos Int. 2007;18:453–462. (Level of evidence: 1B)
- ↑ Hourigan SR, Nitz JC, Brauer SG, O'Neill S, Wong J, Richardson CA. Positive effects of exercise on falls and fracture risk in osteopenic women. Osteoporos Int. 2008;19:1077–1086. (Level of evidence: 1B)
- ↑ Sinaki M, Lynn SG. Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study.Am J Phys Med Rehabil. 2002 Apr;81(4):241-6. (Level of Evidence: 3B)
- ↑ 22.0 22.1 22.2 Sinaki M. Exercise for patients with osteoporosis: management of vertebral compression fractures and trunk strengthening for fall prevention.PM R. 2012 Nov;4(11):882-8. (Level of Evidence: 3A)
- ↑ Itoi E, Sinaki M.Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age.Mayo Clin Proc. 1994 Nov;69(11):1054-9. (Level of Evidence: 3B)
- ↑ Sinaki M.The role of physical activity in bone health: a new hypothesis to reduce risk of vertebral fracture.Phys Med Rehabil Clin N Am. 2007 Aug;18(3):593-608, xi-xii. (Level of Evidence: 5)
- ↑ Chen BL, Zhong Y, Huang YL, Zeng LW, Li YQ, Yang XX, Jiang Q, Wang CH. Systematic back muscle exercise after percutaneous vertebroplasty for spinal osteoporotic compression fracture patients: a randomized controlled trial.Clin Rehabil. 2012 Jun;26(6):483-92. (Level of Evidence: 1B)
- ↑ Wendlova J. The importance of carrying a backpack in the rehabilitation of osteoporotic patients (biomechanical analysis).Bratisl Lek Listy. 2011;112(1):41-3. (Level of Evidence: 4)
- ↑ Bautmans I, Van Arken J, Van Mackelenberg M, Mets T. Rehabilitation using manual mobilization for thoraic kyphosis in elderly postmenopauzal patients with osteoporosis. J Rehabil Med 2010, 42: 129-135. (Level of Evidence: 3B)