Ovarian Cancer
Original Editors - Trisha Counce & Brandy Hirsch from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Brandy Hirsch, Trisha Counce, Lucinda hampton, Aminat Abolade, Vidya Acharya, Elaine Lonnemann, WikiSysop, Kim Jackson, Rishika Babburu, 127.0.0.1 and Wendy Walker
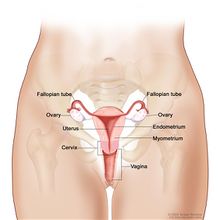
Definition/Description[edit | edit source]
Ovarian cancer (OC) is one of the most common gynecologic cancers that has the highest mortality rate.[1]
The term "ovarian cancer" encompasses several types of cancer that all arise from the cells of the ovaries in the female reproductive system.[2]
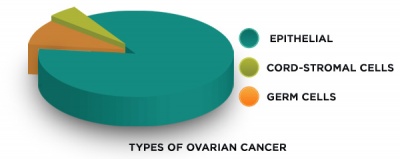
Ovarian cancer commonly manifests as three different types
- Epithelial - derived from the cells on the surface of the ovary or fallopian tube, accounts for about 70% of all ovarian cancers, making it the most common type.[2]
2. Germ cell - derived from the cells that produce eggs
3. Cord-stromal cell - derived from the connective tissue within the ovary[3]
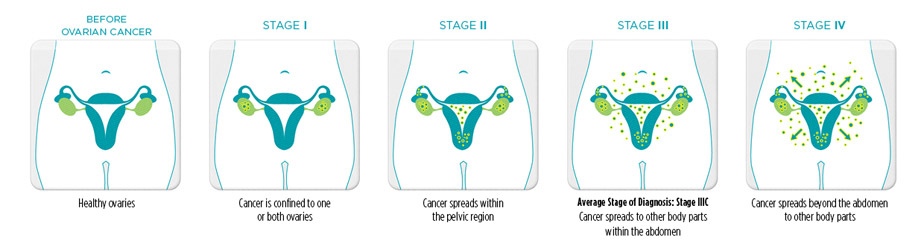
Stages [edit | edit source]
- Stage I - Growth of the cancer is limited to the ovary or ovaries.
- Stage II - Growth of the cancer involves one or both ovaries with pelvic extension.
- Stage III - Growth of the cancer involves one or both ovaries, and one or both of the following are present: (1) the cancer has spread beyond the pelvis to the lining of the abdomen; and (2) the cancer has spread to lymph nodes. The tumor is limited to the true pelvis but with histologically proven malignant extension to the small bowel or omentum.
- Stage IV - This is the most advanced stage of ovarian cancer. Growth of the cancer involves one or both ovaries and distant metastases (spread of the cancer to organs located outside of the peritoneal cavity) have occurred. Finding ovarian cancer cells in pleural fluid (from the cavity which surrounds the lungs) is also evidence of stage IV disease[3].
Risk of Recurrence:
- Patients diagnosed in stage I have a 10 percent chance of recurrence.
- Patients diagnosed in stage II have a 30 percent chance of recurrence.
- Patients diagnosed in stage III have a 70 to 90 percent chance of recurrence.
- Patients diagnosed in stage IV have a 90 to 95 percent chance of recurrence[4].
Prevalence and Incidence [edit | edit source]
Population growth, increased risk factors of cancer, decreased pregnancy and duration of lactation, as well as tube ligation have led to an upward trend in the incidence of OC around the world.
- It is the fifth most common cause of death from cancer in women, and is the most lethal of all gynecological cancers.
- The lifetime risk of a woman developing ovarian cancer is 1 in 71, and 1 in 200 women will develop ovarian cancer between their 50th and 70th birthday.
- Ninety percent of all deaths from ovarian cancer are due to high-grade serous cancer, and this cancer sub-type accounts for 75% of all cases[5].
- Worldwide, 295,414 cases of ovarian cancer have been identified in 2018, accounting for 3.4% of all cancer cases in women.
The incidence of epithelial ovarian cancers varies in different age and race groups.
- Higher among transitioned countries
- Approximately 30% of ovarian cancer cases occur in European countries
- In 2012, the highest rates of ovarian cancer occurred in China (14.60% of all cases), India (11.33% of all cases), and the US (81.8% of all cases).
- In 2012 that year, 22,240 cases of ovarian cancer were detected in the US alone.
- Among the Asian countries, Singapore, Kazakhstan, and Brunei have the highest standardized incidence rate of ovarian cancer
Considering the heavy burden of ovarian cancer on women's health, preventive measures as well as health education and early detection in high risk groups of women are highly recommended. Although some risk factors cannot be changed, a focus on preventable risk factors may reduce the risk of ovarian cancer.[1]
Mortality[edit | edit source]
In 2018, 184,799 deaths occurred due to ovarian cancer, accounting for 4.4% of the entire cancer-related mortality among women.
- The incidence of cancer is higher among high Human Development Index (HDI) countries however the trend of mortality rate tends to be the reverse
- The highest mortality rate in Asia is seen in India, and the mortality rate has decreased in Europe and North America in recent years, especially among young people.
- The mortality-to-incidence ratio is high among African women, indicating their lack of access to suitable treatment.
- Two-thirds of ovarian cancer mortality is attributable to high-grade serous carcinoma[1].
Etiology/Risk Factors[edit | edit source]
General risk factors include
- nulliparity
- Middle-aged (50) or older [6]
- early menopause
- gonadal dysgenesis
- family history: contributes to 24% of cases of epithelial ovarian cancer
- BRCA1/BRCA2 mutations: particularly for serous types
- Lynch syndrome-associated ovarian cancers most often have an endometrioid or serous type histology
- smoking: especially for mucinous adenocarcinoma
- previous history of breast, endometrial or colon cancer
- certain ethnic groups
Protective factors
- oral contraceptives
- breastfeeding (this is controversial)[7]
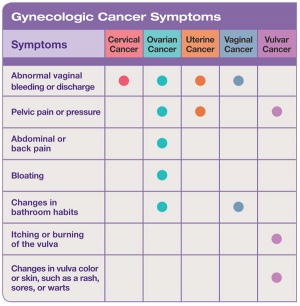
Characteristics/Clinical Presentation[edit | edit source]
Epithelial ovarian cancer presents with a wide variety of vague and nonspecific symptoms.[8] Ovarian cancer may cause one or more of these signs and symptoms--
- Bloating, which is when the area below your stomach swells or feels full [8][6][9]
- Vaginal bleeding or discharge (not normal for individual) [6][8]
- Pain in the pelvic or abdominal area, abdominal distension or discomfort, abdominal mass [6][8]
- Back pain [6][9]
- Feeling full quickly while eating [6][8][9]
- Painful urinination or frequent urges, constipation, or diarrhea [6][9]
- Indigestion and acid reflux [8]
- Shortness of breath (SOB) [8]
- Weight Loss
- Persistent lack of energy [9]
Medications[edit | edit source]
Common Drugs & Drug Combinations Used in Chemotherapy [2]
- Carboplatin & Paclitaxel
- Cisplatin & Paclitaxel
- Bevacizumab
- Paclitaxel & Bevacizumab
If it is not the first time a patient has received chemotherapy, the type of drugs used are determined by how long it has been since the last time they took a drug containing platinum.[3] If it has been less than 6 months, the patient is termed platinum resistant. If it has been more than 6 months since the last day of platinum-based chemotherapy, then often a platinum-containing drug will be used again.[4]
In patients who are platinum resistant, a single drug is often used. Some of these include:[3][2]
Pegylated liposomal doxoruicin, Docetaxel, Paclitaxel, Topotecan, Gemcitabine, Etoposide, or Bevacizumab
Other Drugs Approved for Ovarian Cancer [2][3][4]
Adriamycin PFS
Adriamycin RDF
Carboplatin
Clafen
Cisplatin
Cyclophosphamide
Cytoxan
Doxorubic in Hydrochloride
Dox-SL
DOXIL
Doxorubicin Hydrochloride Liposome
Evacet
Gemcitabine Hydrochloride
Gemzar
Hycamtin
LipoDox
Neosar
Paclitaxel
Paraplat
Paraplatin
Platinol
Platinol-AQ
Taxol
Topotecan Hydrochloride
Diagnostic Tests[edit | edit source]
There are currently no reliable screening tools available to diagnose ovarian cancer.
- One goal of all cancer therapy is to provide early screening and pre-emptive intervention to avoid the challenges presented by highly metastatic cancers. The stages of cancer have a huge influence on the outcome. Early diagnosis of cancer will fundamentally affect the management of these tumors.[5]
- The current recommendations include an annual pelvic exam, transvaginal ultrasound, and CA-125 blood test.[10]
- These are the best options for screening but even in combination, results have been found to be unreliable.
Systemic Involvement[edit | edit source]
Ovarian cancer can effect several different systems including the gastrointestinal, urogenital, cardiovascular, pulmonary, and musculoskeletal. Systemic issues that can occur with ovarian cancer consist of abdominal bloating, discomfort, pain, distension, indigestion, and acid reflux. Pelvic pain or discomfort, back pain, painful urination, constipation, and/or diarrhea are additional symptoms that may acovarian cancer. A sensation of shortness of breath can also occur which can be confused with a cardiopulmonary dysfunction. [6][9][8] In addition, it has been found that patients with ovarian cancer demonstrate an altered lipid metabolism. This condition may lead to a future epidemiological finding. [11]
Medical Management[edit | edit source]
There are three main treatment types for ovarian cancer:[3]
1) Surgery - Surgery to remove the cancerous growth is the most common method of diagnosis and therapy for ovarian cancer. It is best performed by a qualified gynecologic oncologist.
2) Chemotherapy - Chemotherapy is the treatment of cancer using chemicals (medications) that travel through the bloodstream to destroy cancer cells or stop them from growing both in and outside the ovaries. Chemotherapy is used in the majority of cases as a follow-up therapy to surgery.
- Intraperitoneal - medicine is placed directly into the peritoneal area through a surgically implanted port and catheter. New advances have combined it with intravenous (IV) therapy, using chemotherapy agents that work best for treating ovarian cancer. The National Cancer Institute recommends that, for select ovarian cancer patients, chemotherapy be given by both IV and IP. This combination has been found to increase survival for women with advanced stage ovarian cancer.[10]
- Neoadjuvant - a patient may receive chemotherapy before having surgery to remove their tumor.[10]
3) Radiation Therapy - Radiation therapy uses high-energy X-rays to kill cancer cells and shrink tumors (only rarely used in the treatment of ovarian cancer in the United States).
Side effects of Chemotherapy:[10]
- Hair loss
- Nausea & Vomiting
- Fatigue
- Diarrhea & Constipation
- Nerve Problems
- Mouth Issues
- Sexual & Intimacy Issues
- "Chemobrain"
Physical Therapy Management (current best evidence)[edit | edit source]
Although there are no specific physical therapy protocols for ovarian cancer, evidence supports the benefits of physical therapy in improving daily function, quality of life, and health in patients with cancer. As part of your cancer treatment, physical therapists can help you design an individualized exercise program. There are many reasons for being physically active during cancer treatment, but each person’s exercise program should be based on what is safe and what works best for them. It should also be something you like doing. Your exercise plan should take into account any exercise program you already follow, what you can do now, and any physical problems or limits you have. [12] These therapeutic exercises aim to reduce fatigue and optimize physical function, safety and well-being. [13]
An exercises regimen could include:
- Range-of-motion training with [14]
- Light resistance exercises [14]
- Cardiovascular activity [15]
- Flexibility exercises [15]
- Strength training [15]
Exercise, even minimal physical exertion, increases heart rate and muscle flexion while boosting your body’s tolerance to chemotherapy and radiation treatments. Participating in daily exercise programs will enable you to gain a sense of physical control over your condition, and will provide an outlet for stress and anxiety. In addition, exercise will instill you with the motivation and the drive for optimal wellness. [14]
Physical therapy also provides:
- Massage Therapy, which recent studies show can decrease stress, anxiety, depression, and pain, and increase alertness [15]
- Lymphedema Therapy
- Self-Care Managment to improve an individuals ability to return to their home
The American Cancer Society outlines the following for physical activity after cancer treatment. [16]
When you are recovering from cancer treatment
- Many side effects get better within a few weeks after cancer treatment ends, but some can last much longer or even emerge later. Most people are able to slowly increase exercise time and intensity.
- What may be a low- or moderate-intensity activity for a healthy person may seem like a high-intensity activity for some cancer survivors.
When you are living disease-free or with stable disease
- During this phase, physical activity is important to your overall health and quality of life. It may even help some people live longer. There’s some evidence that getting to and staying at a healthy weight, eating right, and being physically active may help reduce risk of second cancer as well as other serious chronic diseases. More research is needed to be sure about these possible benefits.
The American Cancer Society recommends that cancer survivors take these actions
- Take part in regular physical activity.
- Avoid inactivity and return to normal daily activities as soon as possible after diagnosis.
- Aim to exercise at least 150 minutes per week.
- Include strength training exercises at least 2 days per week.
A growing number of studies have looked at the impact of physical activity on cancer recurrence and long-term survival. Exercise has been shown to improve cardiovascular fitness, muscle strength, body composition, fatigue, anxiety, depression, self-esteem, happiness, and several quality of life factors in cancer survivors. At least 20 studies of people with breast, colorectal, prostate, and ovarian cancer have suggested that physically active cancer survivors have a lower risk of cancer recurrence and improved survival compared with those who are inactive. Randomized clinical trials are still needed to better define the impact of exercise on such outcomes.
Those who are overweight or obese after treatment should limit high-calorie foods and drinks, and increase physical activity to promote weight loss. Those who have been treated for digestive or lung cancers may be underweight. They may need to increase their body weight to a healthier range, but exercise and nutrition are still important. Both groups should emphasize vegetables, fruits, and whole grains. It’s well known that obesity is linked with a higher risk of developing some cancers. It’s also linked with breast cancer recurrence, and it might be related to the recurrence of other types of cancer, too. Exercise can help you get to and stay at a healthy weight.
Living with advanced cancer
- Some level of physical activity can improve quality of life for people with certain types of cancer, even if the disease is advanced (has spread to many places and/or is no longer responding to treatment). But this varies by cancer type, physical ability, health problems related to the cancer or cancer treatment, and other illnesses. The situation can also change quickly for a person with advanced cancer, and physical activity should be based on the person’s goals, abilities, and preferences.
Differential Diagnosis[edit | edit source]
Ovarian cancer presents with few diagnostic dilemmas yet it is commonly misdiagnosed as Extraovarian Primary Peritoneal Carcinoma (EOPPC) and adnexal masses (ovarian cysts). The differential diagnosis for these two diagnosis are extensive, with most masses representing benign processes. [17][8] EOPPC is an abdominal cancer without ovarian involvement. It mimics the signs and symptoms of ovarian cancer as well as the microscopic appearance and pattern of spread. Ovarian cysts are difficult to differentiate without histopathologic tissue diagnosis, a definitive diagnosis is generally precluded. Physicians must evaluate the likelihood of a pathologic process using clinical and radiologic information and balance the risk of surgical intervention for a benign versus malignant process. [8]
In addition, ovarian carcinoma will sometimes present first with a paraneoplastic syndrome such as polyarthritis syndrome, carpal tunnel, myopathy, plantar fasciitis, or palmar fasciitis (swelling, digital stiffness or contractures, palmar erythema). The condition may be misdiagnosed as chronic regional pain syndrome (CRPS), Dupuytren’s contracture, or a rheumatologic disorder. Hand and upper extremity manifestations often appear before the tumor is clinically evident. [17]
Additional Differential Diagnosis: [8]
Malignant gastric tumors
Anovulation
Appendiceal tumors
Appendicitis, Acute
Ascites
Benign lesions of the uterine corpus
Bladder distention/urinary retention
Borderline Ovarian Cancer
Cervicitis
Colon cancer
Embryologic remnants
Endometriosis
Gastric Cancer
Irritable Bowel Syndrome
Low-lying cecum
Metastatic gastrointestinal carcinoma
Ovarian torsion
Pancreatic Cancer
Pelvic abscess
Pelvic Inflammatory Disease
Pelvic kidney
Peritoneal Cancer
Peritoneal cyst
Rectal Cancer
Retroperitoneal mass
Urachal cyst
Urinary Tract Obstruction
Uterine Cancer
Uterine fibroids
Case Reports/ Case Studies[edit | edit source]
Physical Activity and Ovarian Cancer
Early Symptoms of Ovarian Cancer In Young Patients
Recreational Activity and Ovarian Cancer
Fertility Drugs and Ovarian Cancer
Resources[edit | edit source]
Stages of Ovarian Cancer Video
National Ovarian Cancer Coalition Clinical Trials
Womens Health Website--Ovarian Cancer Fact Sheet
Social Media Support Group Healthheo
Ovarian Cancer National Alliance
Gilda Radner Familial Ovarian Cancer Registry
Daily Rx Website--Ovarian Cancer
More information about complementary and alternative treatments can be found in the Ovarian Cancer Guide to Quality of Life Issues and can be ordered by calling 1-888-OVARIAN (1-888-682-7426).
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Momenimovahed Z, Tiznobaik A, Taheri S, Salehiniya H. Ovarian cancer in the world: epidemiology and risk factors. International journal of women's health. 2019;11:287.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6500433/ (last accessed 2.9.2020)
- ↑ 2.0 2.1 2.2 2.3 2.4 Green A. Ovarian Cancer (Cancer of the Ovaries). MedicineNet.com. http://www.medicinenet.com/ovarian_cancer/article.htm. Updated September 24, 2013. Accessed March 12, 2014.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Medical Information. National Ovarian Cancer Coalition. http://ovarian.org/what_is_ovarian_cancer.php. Accessed March 12, 2014.
- ↑ 4.0 4.1 4.2 Ovarian Cancer. National Cancer Institute. http://www.cancer.gov/cancertopics/types/ovarian. Accessed March 12, 2014.
- ↑ 5.0 5.1 Xian W, George S. Meeting report from the 2018 12th Biennial Ovarian Cancer Research Symposium detection and prevention of ovarian cancer. International Journal of Gynecologic Cancer. 2019 Aug 1;29(Suppl 2):s2-6.Available from:https://ijgc.bmj.com/content/29/Suppl_2/s2.long (last accessed 2.9.2020)
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 Ovarian Cancer. Center for Disease Control and Prevention. http://www.cdc.gov/cancer/ovarian/index.htm. Updated June 17, 2013. Accessed March 12, 2014.</ref>
- ↑ Radiopedia OC Available from:https://radiopaedia.org/articles/ovarian-tumours (last accessed 2.9.2020)
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 Green A. Ovarian Cancer. Medscape. http://emedicine.medscape.com/article/255771-overview#a0101. Published 1994-2014. Updated March 10, 2014. Accessed March 12, 2014.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Mayo Clinic Staff. Diseases and Conditions Ovarian Cancer. http://www.mayoclinic.org/diseases-conditions/ovarian-cancer/basics/definition/con-20028096. Published 1998-2014. Updated November 10, 2012. Accessed March 12, 2014.
- ↑ 10.0 10.1 10.2 10.3 Ovarian Cancer Institute. http://ovariancancerinstitute.org. Published 2014. Accessed March 12, 2014.
- ↑ Gercel-Taylor C, Doering D, Kraemer F, Taylor D. Aberrations in normal systemic lipid metabolism in ovarian cancer patients.Gynecologic Oncology. January 1996;60(1):35-41. Available from: MEDLINE, Ipswich, MA. Accessed March 12, 2014.
- ↑ Physical Activity and the Cancer Patient. American Cancer Society. http://www.cancer.org/treatment/survivorshipduringandaftertreatment/stayingactive/physical-activity-and-the-cancer-patient. Published 2014. Updated February 6, 2013. Accessed March 12, 2014.
- ↑ Oncology Rehabilitation for Ovarian Cancer. Cancer Treatment Centers of America. http://www.cancercenter.com/ovarian-cancer/oncology-rehabilitation/. Published 2014. Accessed March 12, 2014.
- ↑ 14.0 14.1 14.2 Oncology Rehabilitation for Ovarian Cancer. Cancer Treatment Centers of America. http://www.cancercenter.com/ovarian-cancer/oncology-rehabilitation/. Published 2014. Accessed March 12, 2014.
- ↑ 15.0 15.1 15.2 15.3 Physical Therapy. Cancer Compass. http://www.cancercompass.com/cancer-treatment/physical-therapy.htm. Published 2014. Accessed March 12, 2014.
- ↑ Ovarian Cancer Overview. American Cancer Society. http://www.cancer.org/acs/groups/cid/documents/webcontent/003070-pdf.pdf. Published 2013. Updated February 6, 2014. Accessed March 12, 2014.fckLRfckLRfckLRfckLR<span>Additional co-morbidities associated with ovarian cancer: <ref>Chia V, O'Malley C, Griffiths R, et al. Prevalence and incidence of comorbidities in elderly women with ovarian cancer. Gynecologic Oncology [serial online]. May 2013;129(2):346-352. Available from: MEDLINE, Ipswich, MA. Accessed March 12, 2014.
- ↑ 17.0 17.1 1. Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. Saunders; 2012.