Personal Protective Equipment (PPE)
Introduction[edit | edit source]
Protecting ourselves so that we can continue to help others, is a priority for health care providers around the world. This includes being conscious and up to date with infection prevention, control measures and the appropriate implementation of personal protective equipment (PPE), hand hygiene and waste management of potentially harmful materials.
According to the World Health Organization (WHO), personal protective equipment "...consists of garments placed to protect the health care workers or any other persons to get infected"[1]
Medical PPE typically includes: face protection, goggles and mask or faceshield, gloves, gown or coverall, head cover, and rubber boots.
The following page addresses specifically medical PPE, for the protection against possible external infectious pathogens or substances.
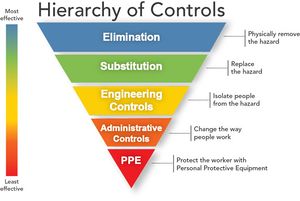
Hierarchy of Safety and Health Controls[edit | edit source]
According to the Occupational Safety and Health Administration (OSHA) the protection of healthcare workers from infectious disease exposures in the workplace requires a combination of controls:
- Training and administrative controls: By providing appropriate safety and infection control training to healthcare professionals, and administrative controls such as establishing and applying isolation policies and procedures, also procedures to identify patients with communicable diseases before the exposure to healthcare worker.
- Engineering controls: such as negative pressure rooms for patients with airborne diseases such as TB,
- Work practice control: for example, not recapping needles.
- Personal Protective Equipment (PPE): Although PPE is at the end of the hierarchy of prevention, it is very important for protecting healthcare workers from disease transmission.
Types of PPE[edit | edit source]
- Gloves: Protects your hands from microbes and minimizes the possible spreading of microbes.
- Masks: Cover your mouth and nasal area. Some masks have a see-through plastic piece, which also covers your eyes (shield). A special respiratory mask (respirator) forms a tight seal around your nose and mouth. It can be useful to minimize the inhalation of smaller microbes, such as tuberculosis bacteria. Click here for a comprehensive guide on selecting the appropriate face mask.
- Eye protection: This includes face shields as well as goggles. They can protect the mucous membranes of your eyes from bodily fluids. If the fluids make contact with the eyes, microbes within the fluid can enter the body through the mucous membranes.
- Clothing: Includes gowns, aprons, head covering, and shoe covers.
Selection of Appropriate PPE[edit | edit source]
It is important to consider the following factors influencing the selection of PPE:
- Type of anticipated exposure: Such as from touch or surfaces, splashes or sprays, or large volumes bodily fluids, which may seep through the clothing. PPE selection (and combinations of PPE), is determined by the category of isolation of the patient being treated (see the link below from the CDC).
- Durability and appropriateness of the PPE for the task. This will affect, for example, whether a gown or apron is selected. If a gown is required, the type of gown is also important. Does it need to be fluid resistant, fluid proof, both or neither?
- Fitting. PPE must fit the individual user (form a proper seal). For example; if a glove is too large / too small than the person's hand, it will compromise the level of protection while also affecting the dexterity of the health care provider.
Click here for a full list of recommendations for the application of standard precautions for the care of all patients in all healthcare settings, according to the Centre of Disease Control and Prevention (CDC - US).
There are also some limiting factors to consider when wearing PPE in a healthcare environment. It is important to have a full understanding of the different types of PPE, when making your selection based on the purpose and goal of the protection.
Using a head or full body ventilated PPE suit equipped with powered-air-purifying-respirators was found to cause reduced dexterity due to multiple glove layering. Back pain related to the respirator of the fully ventilated suit and impaired visibility by a flexible face shield may also be an issue. The temperature of the work environment may also have an impact on healthcare workers, as working at a temperature of 28°C wearing a full body ventilated PPE may cause heat stress and dehydration. Whereas a temperature of 22°C had no negative impact on the same physical parameters[2].
Different Types of Personal Protective Equipment[edit | edit source]
Gloves[edit | edit source]
Gloves are the most common type of PPE used in a healthcare setting. There are different types of glove material such as: vinyl, latex, latex-free or nitrile. Gloves can also be sterile or non-sterile, single use or reusable. Most patient care activities require the use of a single pair of nonsterile gloves made of either latex, nitrile, or vinyl. However, because of allergy concerns, some facilities have eliminated or limited latex products, including gloves, and now use gloves made of nitrile or other material.
Do’s and Don’ts of glove use:[edit | edit source]
The way you use the gloves influences the risk of infections and disease transmission in healthcare sittings. These are the most important do’s and don’ts of glove use:
- Work from clean to dirty: In this instance it refers to touching clean body sites or surfaces before you touch dirty or heavily contaminated areas.
- Limit opportunities for “touch contamination” - protect yourself, others and environmental surfaces. Example of touch contamination, adjusting glasses, rubbing nose or scratching face with glove that has been in contact with a patient. Furthermore, avoid unnecessarily touching environmental surfaces with contaminated gloves. Surfaces such as light switches, door and cabinet knobs can become contaminated if touched by soiled gloves.
- Change gloves as needed. Always change gloves after use on each patient, and discard them in the nearest appropriate receptacle.
Gowns or Aprons?[edit | edit source]
There are 3 factors influencing the selection of a gown or apron:
- The purpose of use: Isolation gowns are generally the preferred PPE for clothing but aprons occasionally are used where limited contamination is anticipated. If contamination of the arms can be anticipated, a gown should be selected. Gowns should fully cover the torso, fit comfortably over the body, and have long sleeves that fit snuggly at the wrist.
- The material properties of the gown: Isolation gowns are made either of cotton or a spun synthetic material that dictate whether they can be laundered and reused or must be disposed. Cotton and spun synthetic isolation gowns vary in their degree of fluid resistance, another factor that must be considered in the selection of this garb. If fluid penetration is likely, a fluid resistant gown should be used.
- Patient risks and whether a clean, rather than sterile gown, can be used. Clean gowns are generally used for isolation. Sterile gowns are only necessary for performing invasive procedures, such as inserting a central line. In this case, a sterile gown would serve purposes of patient and healthcare worker protection.
Face Protection[edit | edit source]
Masks should fully cover the nose and mouth and prevent fluid penetration. Masks should fit snuggly over the nose and mouth. For this reason, masks that have a flexible nose piece and can be secured to the head with string ties or elastic are preferable.
Goggles provide barrier protection for the eyes. They should fit snuggly over and around the eyes. Goggles with anti-fog features will help maintain clarity of vision.
When skin protection, in addition to mouth, nose, and eye protection, is needed or desired, for example, when irrigating a wound or suctioning copious secretions, a face shield can be used as a substitute to wearing a mask or goggles. The face shield should cover the forehead, extend below the chin, and wrap around the side of the face.
Respiratory Protection[edit | edit source]
Respirators that filter the air before it is inhaled should be used for respiratory protection to protect healthcare workers from hazardous or infectious aerosols, such as Mycobacterium tuberculosis. The most commonly used respirators in healthcare settings are the N95, N99, or N100 particulate respirators.
Like other PPE, the selection of a respirator type must consider the nature of the exposure and risk involved. For example, N95 particulate respirators might be worn by personnel entering the room of a patient with infectious tuberculosis. However, if a bronchoscopy is performed on the patient, the healthcare provider might wear a higher level of respiratory protection, such as a powered air-purifying respirator or PAPR.
Prior the use of a respirator, it is important to undergo a medical evaluation determining the safety of wearing a respirator, fit testing to determine the appropriate size and type, training on how and when to use a respirator and finally fit checking before using it to ensure a proper seal.
Sequence for Donning PPE[edit | edit source]
- Gown or apron.
- Mask or respirator.
- Goggles or face shields.
- Gloves.
However, the combination of PPE used, and therefore the sequence for donning, will be determined by the precautions that need to be taken.
Sequence for Removing PPE[edit | edit source]
- Gloves
- Face shield or goggles
- Gown
- Mask or respirator
The sequence for removing PPE is intended to limit opportunities for self-contamination. The gloves are considered the most contaminated pieces of PPE and are therefore removed first[3]. Below is a video that demonstrates donning and removing PPE.
The Location for Removing PPE[edit | edit source]
This depends on the amount and type of PPE worn and the category of isolation a patient is on, if applicable. If only gloves are worn as PPE, it is safe to remove and discard them in the patient room. When a gown or full PPE is worn, PPE should be removed at the doorway or in an anteroom. Respirators should always be removed outside the patient room, after the door is closed. Hand hygiene should be performed after all PPE is removed.
There is a risk of contamination of skin and clothes during removal of contaminated gloves or gowns. It is important to pay attention on the method of removing PPE to avoid contamination and disease transmission. Educating healthcare workers with the correct way of removing PPE by practice in removal of contaminated PPE with providing immediate visual feedback can reduce the risk of contamination of skin and clothes during removal of PPE[4].
Hand Hygiene[edit | edit source]
Hand hygiene is the cornerstone of preventing infection transmission. You should perform hand hygiene immediately after removing PPE. If your hands become visibly contaminated during PPE removal, wash hands before continuing to remove PPE. Wash your hands thoroughly with soap and warm water or, if hands are not visibly contaminated, use an alcohol-based hand rub. Below is a video that demonstrates the steps of hand hygiene.
Level of Isolation
Helpful Resources[edit | edit source]
- World Health Organization - PPE
- Health & Safety Executive (UK)
- The University of Western Australia - What is PPE?
- Center for Disease Control and Prevention - Isolation Precautions
References[edit | edit source]
- ↑ Protective Personal Equipment. World Health Organization.https://www.who.int/medical_devices/meddev_ppe/en/. Retrieved on: 13 March 2020.
- ↑ Loibner M, Hagauer S, Schwantzer G, Berghold A, Zatloukal K. Limiting factors for wearing personal protective equipment (PPE) in a health care environment evaluated in a randomised study. PloS one. 2019 Jan 22;14(1):e0210775.
- ↑ Cdcgov. Cdcgov. [Online]. Available from: https://www.cdc.gov/niosh/ppe/default.html [Accessed 21 April 2019].
- ↑ Tomas ME, Kundrapu S, Thota P, Sunkesula VC, Cadnum JL, Mana TS, Jencson A, O’donnell M, Zabarsky TF, Hecker MT, Ray AJ. Contamination of health care personnel during removal of personal protective equipment. JAMA internal medicine. 2015 Dec 1;175(12):1904-10.