Post-Concussion Syndrome Case Study: 17 Year Old Male Athlete: Difference between revisions
No edit summary |
Brianna Tam (talk | contribs) (citation) |
||
| Line 75: | Line 75: | ||
After 6 weeks of treatment, the patient has demonstrated significant improvements in response to the intervention. | After 6 weeks of treatment, the patient has demonstrated significant improvements in response to the intervention. | ||
* Increased cervical spine ROM: 80% flexion, 100% extension, L rotation and SF = 100%, R rotation and SF = 75% (no pain, just stiffness) | * Increased cervical spine ROM: 80% flexion, 100% extension, L rotation and SF = 100%, R rotation and SF = 75% (no pain, just stiffness) | ||
* PCSS: The patient’s score decreased from 64 to 52, which is greater than the meaningful change score of 6.8 points. He has reported a decrease in headaches, nausea, dizziness, and balance problems. | * PCSS: The patient’s score decreased from 64 to 52, which is greater than the meaningful change score of 6.8 points. <ref>McLeod TCV, Leach C. Psychometric properties of self-report concussion scales and checklists.(evidence-based practice)(Report). Journal of Athletic Training. 2012 Mar 1;47(2):221–3.</ref> He has reported a decrease in headaches, nausea, dizziness, and balance problems. | ||
* PHQ-9: The patient’s post-intervention score decreased to 9, indicating mild depression severity. As mentioned previously, diagnosing mental health disorders is not within the physiotherapy scope of practice. He was referred to a psychologist to be further assessed and adequately treated as his depressive symptoms have persisted throughout the treatment period. | * PHQ-9: The patient’s post-intervention score decreased to 9, indicating mild depression severity. As mentioned previously, diagnosing mental health disorders is not within the physiotherapy scope of practice. He was referred to a psychologist to be further assessed and adequately treated as his depressive symptoms have persisted throughout the treatment period. | ||
* Community Balance and Mobility Scale: MCID = 8. The patient’s score increased to 62/96, which is clinically significant. He showed improvements in tasks that were previously challenging such as lateral dodging and hopping forward. His score is still below the mean score for his age group, 88.71/96, indicating further progressions and improvements can be made. | * Community Balance and Mobility Scale: MCID = 8. The patient’s score increased to 62/96, which is clinically significant. He showed improvements in tasks that were previously challenging such as lateral dodging and hopping forward. His score is still below the mean score for his age group, 88.71/96, indicating further progressions and improvements can be made. | ||
Revision as of 17:01, 14 May 2020
Original Editor -
Top Contributors -
Abstract[edit | edit source]
This fictional case was created for educational purposes, and highlights some of the key clinical findings of a 17-year old male athlete who experienced a concussion, and subsequently post-concussion syndrome. This case study documents the initial physiotherapy assessment, as well as the follow-up treatments. It highlights the main challenges experienced by the patient, the short-term and long-term goals, the physiotherapy interventions, and the outcomes. The patient’s main concerns were balance difficulties and severe headaches, and he also developed some psychosocial issues, all of which were preventing him from returning to sport and completing school work. The initial assessment revealed decreased cervical range of motion, pain and increased tone on palpation of the musculature around the neck, decreased accessory movements of the cervical spine, and impaired balance and eye movements. Interventions were focused on patient education, increasing cervical range of motion, decreasing pain with movement, improving balance and eye movements, aerobic exercise and functional activities to promote return to sport. After 6 weeks of treatment, the patient made significant improvements in all measured outcomes including cervical range of motion, the Community Balance and Mobility Scale, and the Post-Concussion Symptoms Scale.
Introduction[edit | edit source]
This case study presents a 17-year old hockey player who sustained a concussion and has now been diagnosed with post-concussion syndrome. A concussion typically results in physical and cognitive symptoms that are relatively short-lived and tend to resolve spontaneously within 7-10 days. However, some people experience persistent concussion symptoms that last beyond the general time frame of recovery and can be diagnosed with post-concussion syndrome (PCS).[1] This persistence of symptoms can last for months and sometimes years. Studies have suggested that 21-59% of paediatric patients (under the age of 18) who experience a concussion, will develop the long-lasting symptoms of post-concussion syndrome.[2]
Persisting concussion symptoms can leave the athlete in a vulnerable state and increases the risk of a more debilitating injury if more trauma occurs before recovery is complete.[3] Physiotherapists should be familiar with post-concussion syndrome and should understand that is it important to ensure full recovery before considering a return to sport.
The purpose of this case study is to provide an example of how a patient may present with post-concussion syndrome, as well as possible interventions and outcome measures that may be used to track recovery progress. It is important to note that there are many symptoms and clinical presentations of post-concussion syndrome, therefore intervention strategies will vary among patients according to their functional impairments, activity limitations and participation restrictions.
Client Characteristics[edit | edit source]
A 17-year old male suffered a traumatic brain injury during a hockey game when he collided with a player from the other team. The impact of the collision resulted in a direct blow to the front of his head and he immediately lost consciousness and fell to the ice. The loss of consciousness was brief and only lasted about 2 minutes. Once he regained consciousness, he reported feeling dizziness and confusion. He was taken by ambulance to the emergency department where he was assessed and diagnosed with a mild traumatic brain injury (a.k.a. concussion). The next day, he felt even more dizzy and also reported feeling very nauseous and having an intense headache.
Over the next few months he experienced relapses in his recovery. He reports losing his balance quite often and having constant headaches. He has also been experiencing depression and troubles concentrating. His mother has noted that he has become quite irritable and will often lash out on his family for no reason. He reported a previous concussion about 1 year ago, but with rest the symptoms resolved within a couple of weeks. It has now been 3 months since his injury and the onset of his concussion symptoms. He was reassessed by his family doctor and diagnosed with post-concussion syndrome (PCS). He was referred to physiotherapy to improve his concussion symptoms and help him return to his previous function.
Examination Findings[edit | edit source]
Subjective[edit | edit source]
During the assessment with the physiotherapist, the patient reported experiencing headaches that worsened with neck movement and bright lights (3/10 and dull at rest going up to 8/10 and sharp on the NPRS with movement/lights). Dizziness and issues with balance were also a reported concern. The MRI taken at the hospital immediately after the initial injury showed no significant lesions or other issues. The patient experienced no amnesia however, was now finding it more difficult to focus on school. Using a computer for more than ½ hour also caused a headache, dizziness and some nausea. He states that he takes Tylenol as needed for his headaches, which decreases his pain to 5/10. He reported that doing required readings for school was more difficult than pre-injury and took much longer. The patient noted that he was unmotivated and was not finding the activities he used to enjoy brought him as much happiness.
Previously the patient was a very active and athletic individual, practicing with his hockey team as well as doing resistance training 5 times a week. His family mentioned that recently he was spending most of his spare time just laying in bed and was more impatient than usual. The patient noted avoiding doing some activities as he was worried it would make the pain worse. Sleeping has not been affected. The chief concern of the patient is the headaches and dizziness and his main goal is to be able to complete his school year with minimal symptoms, as well as return to working out and playing sports as quickly as possible.
Objective[edit | edit source]
- Scan exam: normal
- Cranial nerve testing: normal
- Reflexes: normal (grade 2)
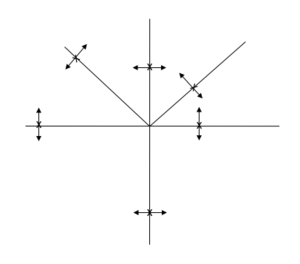
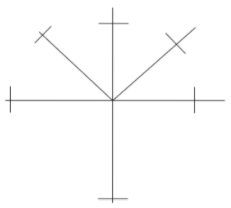
- Decreased cervical spine ROM:
- 50% flexion, 75% extension, L rotation and side flexion (SF) = 90%, R rotation and SF = 40%, all with pain bilaterally (worse with R rotation, SF and flexion)
- Palpation: Increased tone and tenderness of bilateral upper fibres of trapezius, sternocleidomastoid, and sub-occipitals. Tenderness on palpation over C3/C4 and C4/C5 facet joints
- PPIVMs: decreased rotation and side flexion at C3/C4 and C4/C5
- PAIVMS: decreased mobility and pain at C3/4 and C4/5 with IMP (inferior, medial, posterior) glide on the right
- Flexion-rotation test: normal (this indicates the rotation at C1/2 is fine)
- Cranio-cervical flexion test: able to perform craniocervical flexion at 24mm Hg for 2-3 seconds, but not at 26mmHg
- To test for benign paroxysmal positional vertigo the dix-hallpike test was completed: normal
- Visual tests: Smooth pursuit and saccadic eye movement was noticeably slower than normal
Outcome Measures[edit | edit source]
- Post-concussion Symptom Scale (PCSS) is a computerized program and another way to assess concussion symptoms. His score was 64 which is considered a high score and a risk factor for poor prognosis.
- PHQ-9 is a screening questionnaire used to indicate the severity of depression. His score was 11 which indicated moderate depression (Cut score = 10). Although diagnosing a mental illness is considered outside the scope of physiotherapy, it is important for the therapist to consider this as a yellow flag and to be aware of the potential impact on recovery. Communication with the family physician would be helpful to share these findings.
- Community balance and mobility scale is an outcome measure designed for patients with traumatic brain injuries that are higher functioning. The tasks include more difficult activities such as walking and multitasking, hopping and lateral dodging. His score was 45/96 (MCID=8) and can be used to track progress over time.
Clinical Impression[edit | edit source]
Patient is a previously active 17-year old who sustained a concussion 3 months ago. He presents with decreased and painful cervical mobility, dizziness, impaired balance and eye movements, and intense headaches which affect his ability to complete school work and participate in sports. Personal factors that may be contributing to pain are depression, fear of movement and high irritability.
The patient’s previous functional level and supportive home environment are factors indicating a high likelihood of a full recovery and return to sport. The patient is an excellent candidate for physiotherapy activities aimed at restoring pain-free cervical range of motion, and improving balance and functional mobility suitable for his return to sport and school.
Problem List[edit | edit source]
- Headaches and nausea (caused by neck movement and using screens ex computer, phone)
- Eye movement slower than normal and affecting ability to complete school work
- Balance and dizziness issues affecting ability to be physically active
- Fear of movement also affecting physical activity
- Depressive symptoms including lack of motivation
- Personality changes including impatience and quick to anger
Intervention[edit | edit source]
Short-term Goals[edit | edit source]
- The patient will be able to complete school work for 50 minutes using a computer (or other screen) without developing a headache within 4 weeks.
- The patient will increase cervical ROM by 10% in all movements with no pain or headache within 3 weeks.
Long-term Goals[edit | edit source]
- The patient will be able to return to playing with his hockey team with no headaches or dizziness by the beginning of his next hockey season in 8 months.
- The patient will be able to sit and study/complete school work on his computer for 2 hours with no headaches, nausea, or dizziness within 6 months.
Management Program[edit | edit source]
Outcome[edit | edit source]
After 6 weeks of treatment, the patient has demonstrated significant improvements in response to the intervention.
- Increased cervical spine ROM: 80% flexion, 100% extension, L rotation and SF = 100%, R rotation and SF = 75% (no pain, just stiffness)
- PCSS: The patient’s score decreased from 64 to 52, which is greater than the meaningful change score of 6.8 points. [4] He has reported a decrease in headaches, nausea, dizziness, and balance problems.
- PHQ-9: The patient’s post-intervention score decreased to 9, indicating mild depression severity. As mentioned previously, diagnosing mental health disorders is not within the physiotherapy scope of practice. He was referred to a psychologist to be further assessed and adequately treated as his depressive symptoms have persisted throughout the treatment period.
- Community Balance and Mobility Scale: MCID = 8. The patient’s score increased to 62/96, which is clinically significant. He showed improvements in tasks that were previously challenging such as lateral dodging and hopping forward. His score is still below the mean score for his age group, 88.71/96, indicating further progressions and improvements can be made.
- FMA: After the intervention, the patient scored 35/68, indicating an improvement in his fear-avoidance behaviours. He is below the cut-score of 48, which previously indicated a high level of fear-avoidance behaviours.
Discussion[edit | edit source]
This case study illustrates a detailed case of Post-Concussion Syndrome. This patient presented with a variety of physical and behavioural symptoms that are commonly seen in someone with PCS. His depressive symptoms and personality changes were beyond the scope of the physiotherapist and he was appropriately referred to a psychologist to be further assessed and treated. He was a suitable candidate for physiotherapy as he had a number of impairments that needed to be addressed prior to returning to school and participating in sports. The intervention approach included a wide variety of techniques including cervical ROM, endurance training, balance training, eye movement exercises, and aerobic exercise. The treatment method, alongside patient education, significantly improved this patient’s symptoms and functional activity level.
The significant improvements seen in this patient’s outcome measures post-intervention can help inform other physiotherapists, as well as other healthcare providers, when assessing and treating individuals with PCS. However, it is important to note that this is one particular patient and each person will present differently. Each individual with PCS should be assessed and treated with a patient-centered approach given their impairments and goals. This case may help inform clinicians when faced with patients presenting in a similar manner.
Self-Study Questions[edit | edit source]
- Physical and cognitive concussion symptoms typically resolve within:
- 50-55 days
- 7-10 days
- 30-35 days
- 1-2 days
- Which of the following would be considered a yellow flag from this case study?
- Impaired balance
- Depressive symptoms
- Headaches
- Dizziness
References[edit | edit source]
- ↑ Fowler Kennedy Sport Medicine. Post-Concussion Syndrome Management Guidelines. Available from: https://www.fowlerkennedy.com/wp-content/uploads/2017/02/Post-Concussion-Treatment-Guidelines.pdf (Accessed 12 May 2020).
- ↑ Ellis MJ, Cordingley D, Vis S, Reimer K, Leiter J, Russell K, et al. Vestibulo-ocular dysfunction in pediatric sports-related concussion. Journal of neurosurgery Pediatrics [Internet]. 2015 Sep;16(3):248–55. Available from: http://search.proquest.com/docview/1708903933/
- ↑ Leddy JJ, Sandhu H, Sodhi V, Baker JG, Willer B. Rehabilitation of Concussion and Post-concussion Syndrome. Sports Health: A Multidisciplinary Approach. 2012 Mar;4(2):147–54.
- ↑ McLeod TCV, Leach C. Psychometric properties of self-report concussion scales and checklists.(evidence-based practice)(Report). Journal of Athletic Training. 2012 Mar 1;47(2):221–3.