Posterior Knee Pain: Difference between revisions
Oyemi Sillo (talk | contribs) No edit summary |
Oyemi Sillo (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox">
'''Original Editor ''' - [[User:Joyce De Gelas|Joyce De Gelas]] | <div class="editorbox">
'''Original Editor ''' - [[User:Joyce De Gelas|Joyce De Gelas]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}
</div><div class="editorbox"></div> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}
</div> | |||
== Description/ definition == | == Description/ definition == | ||
Knee pain is more common in the anterior, medial, and lateral aspect of the knee than in the posterior aspect of the knee. The different diagnoses for posterior knee pain include pathology to the bones, musculotendinous structures, ligaments, and/or to the bursas. Less common are neurologic and vascular injuries. Also tumors, such as a begin tumor that contains both bone and cartilage and usually occurs near the end of a long bone (osteochondroma) or bony tumors. Tenderness of palpation over the tendons or muscles in the back of the knee can indicate muscle or tendon injury. Pain or swelling in the popliteal area suggests an effusion or cyst. <br>A precise understanding of knee anatomy, the physical examination and of the differential diagnosis is needed to accurately evaluate and treat posterior knee pain. | Knee pain is more common in the anterior, medial, and lateral aspect of the knee than in the posterior aspect of the knee. The different diagnoses for posterior knee pain include pathology to the bones, musculotendinous structures, ligaments, and/or to the bursas. Less common are neurologic and vascular injuries. Also tumors, such as a begin tumor that contains both bone and cartilage and usually occurs near the end of a long bone (osteochondroma) or bony tumors. Tenderness of palpation over the tendons or muscles in the back of the knee can indicate muscle or tendon injury. Pain or swelling in the popliteal area suggests an effusion or cyst. <br>A precise understanding of knee anatomy, the physical examination and of the differential diagnosis is needed to accurately evaluate and treat posterior knee pain.<ref name="1">S. English, D. Perret. Posterior knee pain, Internet, 12 June 2010, | ||
http://link.springer.com/article/10.1007/s12178-010-9057-4/fulltext.html, 29/11/2012, (evidence level 4).</ref> | |||
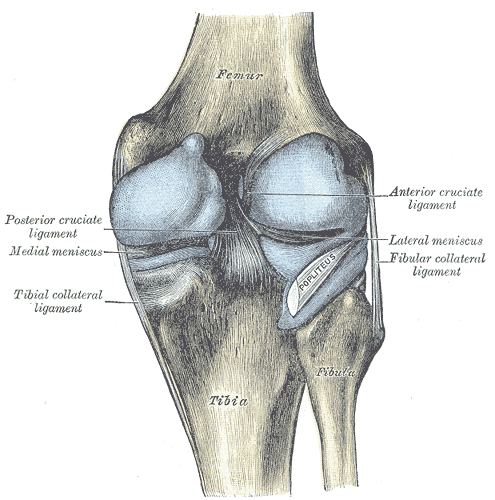
= Clinically Relevant Anatomy = | = Clinically Relevant Anatomy = | ||
<br> | |||
The anatomy of the | The anatomy of the [http://www.physio-pedia.com/Knee knee] and [[]] is important when evaluating posterior knee pain.<ref name="1" /> <ref name="8">http://www.eorthopod.com/content/popliteal-cysts</ref> | ||
<br> | [[Image:Posterior_knee.png|posterior view of knee joint]]<br> | ||
<br> | <br><br> | ||
SM<br>The semimembranosus tendon is a part of the posteromedial joint capsule, which is important in controlling anteromedial rotatory instability. (Together with the pes anserinus tendons it gives medial and posteromedial reinforcement.) | SM<br>The semimembranosus tendon is a part of the posteromedial joint capsule, which is important in controlling anteromedial rotatory instability. (Together with the pes anserinus tendons it gives medial and posteromedial reinforcement.)<ref name="12">Darlene Hertling, Randolph M. Kessler, “Management Of Common Musculoskeletal Disorders: Physical Therapy Principles and Methodes” (fourth edition), LippinCott Williams & Wilkins</ref> There is a U-shaped bursa that surrounds the distal SM tendon, separating it from the medial-tibial plateau, medial (tibial) collateral ligament (MCL), and semitendinosus tendon (surrounding structures).<ref name="1" /> <br>Fig.1A demonstrates the semimembranosus tendon, with its divisions: anterior arm (Ant), direct arm (Dir), inferior arm (Inf) and the oblique popliteal ligament (OPL). <br>Fig.1B: The capsular arm of the semimembranosus (Caps. Sm.) intertwines with the capsular bundle of the posterior oblique ligament (Caps. POL). [13]<br> <br> <br> | ||
= Mechanism of injury = | = Mechanism of injury = | ||
<br>The simple presence of the surrounding anatomical structures causes increased friction to the SM tendon (and irritation to the bursa) during repetitive knee flexion. | <br>The simple presence of the surrounding anatomical structures causes increased friction to the SM tendon (and irritation to the bursa) during repetitive knee flexion.<ref name="1" /> | ||
= Clinical presentation/Characteristics = | = Clinical presentation/Characteristics = | ||
Semimembranosus tendinopathy (SMT)<br>This is an uncommon cause of chronic posteromedial knee pain that more often occurs with older patients. It may be underdiagnosed or inadequately treated because of a lack of understanding of the condition. But timely diagnosis can lead to effective treatments. <br>Although tendinopathy may occur in any of the hamstrings tendons, the semimembranosus tendon is the most commonly affected. It may occur as a primary phenomenon in endurance athletes or as a secondary, overuse, compensatory condition from a primary knee abnormality, such as patellofemoral disorders. | Semimembranosus tendinopathy (SMT)<br>This is an uncommon cause of chronic posteromedial knee pain that more often occurs with older patients. It may be underdiagnosed or inadequately treated because of a lack of understanding of the condition. But timely diagnosis can lead to effective treatments. <br>Although tendinopathy may occur in any of the hamstrings tendons, the semimembranosus tendon is the most commonly affected. It may occur as a primary phenomenon in endurance athletes or as a secondary, overuse, compensatory condition from a primary knee abnormality, such as patellofemoral disorders.<ref name="11">Nicola Maffulli, Per Renstrom, Wayne B. Leadbetter, “Tendon Injuries: Basic Science and Clinical Medicine”, Uitgeverij: Springer</ref> <br>SMT usually presents as an aching pain localized to the posteromedial knee with tenderness on palpation inferior to the joint.<ref name="1" /> The pain is severe in its acute form, but symptoms increase with activities that involve significant hamstring activation: running, cycling, walking down stairs, climbing, or sudden deep knee flexion.<ref name="2">William E. Bylund, Kevin de Weber. Semimembranosus tendinopathy, Pubmed, 2010 September, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445062/ , 29/11/2012, (evidence of level 4).</ref><ref name="10">Proper shoe fit: http://walking.about.com/od/prshoe/tp/shoemotion.htm</ref> <br>• Hamstring Strain (HSS)<br>Characteristics of hamstring strain.<br>Main symptoms are, a sudden sharp pain during sport activities, it can also be described as a tearing impression, and tightness, weakness and impaired range of motion. <br> | ||
= <br>Diagnostic Procedures = | = <br>Diagnostic Procedures = | ||
| Line 32: | Line 31: | ||
= <br>Management / interventions = | = <br>Management / interventions = | ||
Medical therapy management <br>SMT<br>- Injection(s) of 3 mL of 2% lidocaine and 10 mg triamcinolone at the insertion site can be effective in relieving the symptoms. | Medical therapy management <br>SMT<br>- Injection(s) of 3 mL of 2% lidocaine and 10 mg triamcinolone at the insertion site can be effective in relieving the symptoms.<ref name="2" /> <br>- Surgery to reroute and reattach the tendon is rarely needed but may be effective.<ref name="2" /> | ||
Physical therapy management<br>- ¬SMT | |||
'''Physical therapy management'''<br>- ¬SMT<ref name="2" /><br>In more than 90% of the cases, this condition will heal without further intervention. | |||
1. Initial conservative treatment includes relative rest, ice, pain-relieving modalities, a short course of NSAIDs, and physical therapy that includes hamstring strengthening and stretching exercises. | 1. Initial conservative treatment includes relative rest, ice, pain-relieving modalities, a short course of NSAIDs, and physical therapy that includes hamstring strengthening and stretching exercises. | ||
2. SMT may benefit from proper shoe fit to prevent overpronation or a medial heel lift in patients with genu valgum. Proper shoe fits are stable running shoes and shoes with motion control technology, they provide extra support preventing your ankle from rolling inwards extremely. Wearing these shoes is even more important when you are | 2. SMT may benefit from proper shoe fit to prevent overpronation or a medial heel lift in patients with genu valgum. Proper shoe fits are stable running shoes and shoes with motion control technology, they provide extra support preventing your ankle from rolling inwards extremely. Wearing these shoes is even more important when you are overweight. The main stability features are the medial post, the engineered heel and the plastic shank under the arch.<ref name="9">Proper shoe fit: http://www.runningshoesguru.com/2012/02/5-best-stability-running-shoes/</ref><ref name="10" /> | ||
E.g. : Nike Zoom Structure Triax 15 | E.g. : Nike Zoom Structure Triax 15 | ||
| Line 46: | Line 47: | ||
<br> | <br> | ||
Hamstring strain | Hamstring strain<ref name="3">SANDRA J. SHULTZ, PEGGY A. HOUGLUM EN DAVID H. PERRIN. Examination of musculoskeletal injuries, third edition, Human Kinetics, 2010, 696 pages.</ref><ref name="4">OHN C. GRIFFIN, Client-centered exercise prescription, Human Kinetics, 1998, 263 pages.</ref><ref name="5">STEVEN J. FLECK, WILLIAM J. KRAEMER, Designing resistance-training programs, second edition, Human Kinetics, 1997, 275 pages.</ref><ref name="6">DANIEL LORENZ, MICHAEL REIMAN, The role and implementation of eccentric training in athletic rehabilitation: tendinopathy, hamstring strains and ACL reconstruction, pubmed, march 2011, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3105370/, 27/11/2012, (evidence level 5).</ref><ref name="7">BRANDON SCHMITT, TYLER TIM AND MALACHY MCHUGH, Hamstring injury rehabilitation and prevention of reinjury using lengthened state eccentric training: a new concept, pubmed, June 2012, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3362981/, 27/11/2012, (evidence level 5).</ref> - RICE-method: rest, ice, compression and elevation to speed the recovery. After the acute stages, heat can be used such as hot packs, whirlpool or heating before the stretching exercises. All the activities should be followed by ice-treatment to decrease inflammation and discomfort. | ||
-The first phase | -The first phase<ref name="7" />: the athlete begins pain free submaximal isometric strengthening at multiple angles. | ||
-Exercise: The athlete completes a set of isometric contractions at 30°, 60°, and 90° of knee flexion by placing the injured limb on top of the contralateral limb and contracting the strained hamstring. The hamstring should not be stretched into a painful range at this time but available hip and knee ROM should be maintained. Motion is also good for aligning fibers and increasing the strength of the lateral adhesion of fibers, which protects the injured fibers from stump separation. The goals of this stage are to normalize gait and to obtain knee flexion strength at greater than 50% of uninjured length upon manual muscle testing at 90 degrees of knee flexion. | -Exercise: The athlete completes a set of isometric contractions at 30°, 60°, and 90° of knee flexion by placing the injured limb on top of the contralateral limb and contracting the strained hamstring. The hamstring should not be stretched into a painful range at this time but available hip and knee ROM should be maintained. Motion is also good for aligning fibers and increasing the strength of the lateral adhesion of fibers, which protects the injured fibers from stump separation. The goals of this stage are to normalize gait and to obtain knee flexion strength at greater than 50% of uninjured length upon manual muscle testing at 90 degrees of knee flexion. | ||
| Line 56: | Line 57: | ||
<br> | <br> | ||
<br>- The second phase<ref name="6" /><ref name="7" />:The athlete progressively regains strength throughout the ROM and improves neuromuscular control of the hips and pelvis in preparation for sports specific movements. End range lengthening should be avoided if painful in this stage. | |||
<br>- The second phase | |||
Exercises: Eccentric training can be achieved using an isokinetic dynamometer if available and performing exercises such as straight leg deadlift, single leg windmills and the Nordic hamstring exercise. | Exercises: Eccentric training can be achieved using an isokinetic dynamometer if available and performing exercises such as straight leg deadlift, single leg windmills and the Nordic hamstring exercise. | ||
| Line 76: | Line 75: | ||
<br>At the completion of this phase the athlete should have full strength upon manual muscle testing (5/5) or be within 20% of the uninjured leg in the zero to 90° range when measured with a hand held or isokinetic dynamometer in order to progress to the next phase. The athlete should also be able to jog both forward and backward without pain at a moderate speed at this point. | <br>At the completion of this phase the athlete should have full strength upon manual muscle testing (5/5) or be within 20% of the uninjured leg in the zero to 90° range when measured with a hand held or isokinetic dynamometer in order to progress to the next phase. The athlete should also be able to jog both forward and backward without pain at a moderate speed at this point. | ||
- The third phase | - The third phase<ref name="7" />: Focus is on functional movements and eccentric strengthening in the lengthened state. Plyometric and sports specific training may be initiated as well as advanced balance exercise. Alternative lengthened state eccentric training may also be achieved without a dynamometer by keeping the involved thigh on the subject's chest while resisting an outside force with an elastic resistance like a thera-Band, cable column, or manual resistance. | ||
<br> | <br> | ||
| Line 86: | Line 85: | ||
<br> | <br> | ||
<br>Lengthened state eccentric training on cable column. | <br>Lengthened state eccentric training on cable column.<br> | ||
This exercise may be performed by having the patient lay supine pulling knee snugly into chest while hooked up to cable column or elastic resistance. The patient then uses his or her arms to pull the knee into flexion and then slowly eccentrically resists the cable or elastic band as it pulls the knee into extension. At the completion of this stage the athlete should have full strength throughout the range of motion and should be able to confidently perform all sport related tasks without limitation. | |||
This exercise may be performed by having the patient lay supine pulling knee snugly into chest while hooked up to cable column or elastic resistance | |||
<br> | <br> | ||
| Line 102: | Line 95: | ||
Posterior knee pain can be caused by a number of conditions: | Posterior knee pain can be caused by a number of conditions: | ||
*Semimembranosis tendinopathy | *[[Semimembranosus_Tendinopathy|Semimembranosis tendinopathy]] | ||
*Biceps femoris tendinopathy | *[[Biceps_Tendonitis|Biceps femoris tendinopathy]] | ||
*Hamstrings strain | *[[Hamstring_Strain|Hamstrings strain]] | ||
*Calf strain | *[[Calf_Strain|Calf strain]] | ||
*M. popliteus strain | *[[Popliteus_strain|M. popliteus strain]] | ||
*M. popliteus tendinitis | *[[Popliteus_Tendinitis|M. popliteus tendinitis]] | ||
* | *[[Posterior_Cruciate_Ligament_Injury|Posterior cruciate ligament injury ]]<br> | ||
*[[Knee_Rotary_Instability|PLC: Posterolateral corner/ posterior complex]] | |||
* | *[[Knee_Bursitis|Knee Bursitis]] | ||
*Common peroneal nerve injury | *Common peroneal nerve injury | ||
* | *[[Baker's_Cyst|Bak]][[Knee_Bursitis|ee Bursitis]] | ||
*popliteal artery entrapment syndrome, aneurysms | *popliteal artery entrapment syndrome, aneurysms | ||
*Deep venous thrombosis (DVT) | *[[Deep_Vein_Thrombosis|Deep venous thrombosis ]](DVT) | ||
<br>Posterior knee pain can also be referred pain, such as from intra-articular hip pathology, lumbar facet arthropathy, sacroiliac join dysfunction, and sacral radiculopathy. Or it can be caused by peripheral neurological injury and entrapment of nerves in the popliteal fossa. | <br>Posterior knee pain can also be referred pain, such as from intra-articular hip pathology, lumbar facet arthropathy, sacroiliac join dysfunction, and sacral radiculopathy. Or it can be caused by peripheral neurological injury and entrapment of nerves in the popliteal fossa.<ref name="1" /> | ||
= <br>Key Evidence = | = <br>Key Evidence = | ||
| Line 123: | Line 116: | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
<div class="researchbox">
<rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=14ipX3fGPZTPtIuv3-jTCwmSpmERsaO2_10I1g_6E6rcCzQEHA|charset=UTF8|short|max=10</rss>
</div> | <div class="researchbox">
<rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=14ipX3fGPZTPtIuv3-jTCwmSpmERsaO2_10I1g_6E6rcCzQEHA|charset=UTF8|short|max=10</rss>
</div> | ||
= References = | = References = | ||
<references /><br> | |||
<br> | <br> | ||
[[Category:Condition]] [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] [[Category:Knee]] [[Category:Pain]] | [[Category:Condition]] [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] [[Category:Knee]] [[Category:Pain]] | ||
Revision as of 22:19, 12 October 2014
Description/ definition[edit | edit source]
Knee pain is more common in the anterior, medial, and lateral aspect of the knee than in the posterior aspect of the knee. The different diagnoses for posterior knee pain include pathology to the bones, musculotendinous structures, ligaments, and/or to the bursas. Less common are neurologic and vascular injuries. Also tumors, such as a begin tumor that contains both bone and cartilage and usually occurs near the end of a long bone (osteochondroma) or bony tumors. Tenderness of palpation over the tendons or muscles in the back of the knee can indicate muscle or tendon injury. Pain or swelling in the popliteal area suggests an effusion or cyst.
A precise understanding of knee anatomy, the physical examination and of the differential diagnosis is needed to accurately evaluate and treat posterior knee pain.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Clinically Relevant Anatomy[edit | edit source]
The anatomy of the knee and [[]] is important when evaluating posterior knee pain.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
SM
The semimembranosus tendon is a part of the posteromedial joint capsule, which is important in controlling anteromedial rotatory instability. (Together with the pes anserinus tendons it gives medial and posteromedial reinforcement.)Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title There is a U-shaped bursa that surrounds the distal SM tendon, separating it from the medial-tibial plateau, medial (tibial) collateral ligament (MCL), and semitendinosus tendon (surrounding structures).Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Fig.1A demonstrates the semimembranosus tendon, with its divisions: anterior arm (Ant), direct arm (Dir), inferior arm (Inf) and the oblique popliteal ligament (OPL).
Fig.1B: The capsular arm of the semimembranosus (Caps. Sm.) intertwines with the capsular bundle of the posterior oblique ligament (Caps. POL). [13]
Mechanism of injury[edit | edit source]
The simple presence of the surrounding anatomical structures causes increased friction to the SM tendon (and irritation to the bursa) during repetitive knee flexion.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Clinical presentation/Characteristics [edit | edit source]
Semimembranosus tendinopathy (SMT)
This is an uncommon cause of chronic posteromedial knee pain that more often occurs with older patients. It may be underdiagnosed or inadequately treated because of a lack of understanding of the condition. But timely diagnosis can lead to effective treatments.
Although tendinopathy may occur in any of the hamstrings tendons, the semimembranosus tendon is the most commonly affected. It may occur as a primary phenomenon in endurance athletes or as a secondary, overuse, compensatory condition from a primary knee abnormality, such as patellofemoral disorders.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
SMT usually presents as an aching pain localized to the posteromedial knee with tenderness on palpation inferior to the joint.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title The pain is severe in its acute form, but symptoms increase with activities that involve significant hamstring activation: running, cycling, walking down stairs, climbing, or sudden deep knee flexion.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
• Hamstring Strain (HSS)
Characteristics of hamstring strain.
Main symptoms are, a sudden sharp pain during sport activities, it can also be described as a tearing impression, and tightness, weakness and impaired range of motion.
Diagnostic Procedures[edit | edit source]
Outcomes Measures[edit | edit source]
Management / interventions[edit | edit source]
Medical therapy management
SMT
- Injection(s) of 3 mL of 2% lidocaine and 10 mg triamcinolone at the insertion site can be effective in relieving the symptoms.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Surgery to reroute and reattach the tendon is rarely needed but may be effective.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Physical therapy management
- ¬SMTCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
In more than 90% of the cases, this condition will heal without further intervention.
1. Initial conservative treatment includes relative rest, ice, pain-relieving modalities, a short course of NSAIDs, and physical therapy that includes hamstring strengthening and stretching exercises.
2. SMT may benefit from proper shoe fit to prevent overpronation or a medial heel lift in patients with genu valgum. Proper shoe fits are stable running shoes and shoes with motion control technology, they provide extra support preventing your ankle from rolling inwards extremely. Wearing these shoes is even more important when you are overweight. The main stability features are the medial post, the engineered heel and the plastic shank under the arch.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
E.g. : Nike Zoom Structure Triax 15
Hamstring strainCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title - RICE-method: rest, ice, compression and elevation to speed the recovery. After the acute stages, heat can be used such as hot packs, whirlpool or heating before the stretching exercises. All the activities should be followed by ice-treatment to decrease inflammation and discomfort.
-The first phaseCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title: the athlete begins pain free submaximal isometric strengthening at multiple angles.
-Exercise: The athlete completes a set of isometric contractions at 30°, 60°, and 90° of knee flexion by placing the injured limb on top of the contralateral limb and contracting the strained hamstring. The hamstring should not be stretched into a painful range at this time but available hip and knee ROM should be maintained. Motion is also good for aligning fibers and increasing the strength of the lateral adhesion of fibers, which protects the injured fibers from stump separation. The goals of this stage are to normalize gait and to obtain knee flexion strength at greater than 50% of uninjured length upon manual muscle testing at 90 degrees of knee flexion.
-Isometric knee flexion in the seated position. Note that this would be performed at multiple angles.
- The second phaseCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title:The athlete progressively regains strength throughout the ROM and improves neuromuscular control of the hips and pelvis in preparation for sports specific movements. End range lengthening should be avoided if painful in this stage.
Exercises: Eccentric training can be achieved using an isokinetic dynamometer if available and performing exercises such as straight leg deadlift, single leg windmills and the Nordic hamstring exercise.
(Eccentric) Single leg windmills
The patient stands with the uninjured leg on a chair or fixed surface and reaches down in a diagonal plane while keeping stance leg straight and maintaining lumbar lordosis.
It can be performed without (early) weights and progressed by using hand-held weights or kettlebells, as shown.
Nordic hamstring exercise
Having the clinician hold the patient’s feet, while in tall kneeling, performs the Nordic hamstring exercise. The patient slowly falls forward while maintaining neutral hip posture until he or she can't control descent any longer and then pushes back into starting position with upper extremities.
You can do the Nordic hamstrings exercise with elastic assistance, which means that you can replace the helper/clinician in to elastic assistance attached to the wall.”
At the completion of this phase the athlete should have full strength upon manual muscle testing (5/5) or be within 20% of the uninjured leg in the zero to 90° range when measured with a hand held or isokinetic dynamometer in order to progress to the next phase. The athlete should also be able to jog both forward and backward without pain at a moderate speed at this point.
- The third phaseCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title: Focus is on functional movements and eccentric strengthening in the lengthened state. Plyometric and sports specific training may be initiated as well as advanced balance exercise. Alternative lengthened state eccentric training may also be achieved without a dynamometer by keeping the involved thigh on the subject's chest while resisting an outside force with an elastic resistance like a thera-Band, cable column, or manual resistance.
Lengthened state eccentric training on the Biodex.
Using a setup, the Biodex may be modified so that the patient is in hip flexion and then passively extends and flexes the knee into the end range of motion. The patient resists the passive motion as the knee is extended.
Lengthened state eccentric training on cable column.
This exercise may be performed by having the patient lay supine pulling knee snugly into chest while hooked up to cable column or elastic resistance. The patient then uses his or her arms to pull the knee into flexion and then slowly eccentrically resists the cable or elastic band as it pulls the knee into extension. At the completion of this stage the athlete should have full strength throughout the range of motion and should be able to confidently perform all sport related tasks without limitation.
Differential Diagnosis[edit | edit source]
Posterior knee pain can be caused by a number of conditions:
- Semimembranosis tendinopathy
- Biceps femoris tendinopathy
- Hamstrings strain
- Calf strain
- M. popliteus strain
- M. popliteus tendinitis
- Posterior cruciate ligament injury
- PLC: Posterolateral corner/ posterior complex
- Knee Bursitis
- Common peroneal nerve injury
- Bakee Bursitis
- popliteal artery entrapment syndrome, aneurysms
- Deep venous thrombosis (DVT)
Posterior knee pain can also be referred pain, such as from intra-articular hip pathology, lumbar facet arthropathy, sacroiliac join dysfunction, and sacral radiculopathy. Or it can be caused by peripheral neurological injury and entrapment of nerves in the popliteal fossa.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Key Evidence[edit | edit source]
Resources[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
References [edit | edit source]