Posterior Knee Pain: Difference between revisions
No edit summary |
No edit summary |
||
| Line 14: | Line 14: | ||
<br> | <br> | ||
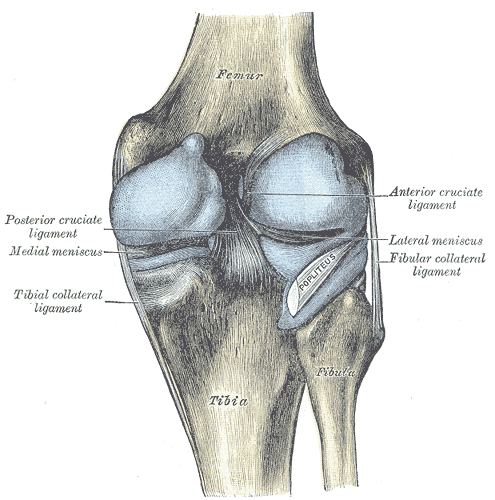
The anatomy of the [http://www.physio-pedia.com/Knee knee] is important when evaluating posterior knee pain.<ref name="p1" /> <ref name="p8">http://www.eorthopod.com/content/popliteal-cysts</ref> | The anatomy of the [http://www.physio-pedia.com/Knee knee] is important when evaluating posterior knee pain.<ref name="p1" /> <ref name="p8">http://www.eorthopod.com/content/popliteal-cysts</ref> There is a complicated network of muscles, ligaments, and other soft tissues around the knee that contributes to the structure and support of the joint. These include both passive and active stabilizers. Examples of passive stabilizers include the [[Medial Collateral Ligament of the Knee|medial collateral ligament]] (MCL), [[Lateral Collateral Ligament|lateral collateral ligament]] (LCL), [[Anterior Cruciate Ligament|anterior cruciate ligament]] (ACL), and [[Posterior Cruciate Ligament Injury|posterior cruciate ligament]] (PCL), while examples of active stabilizers consist of the [[hamstrings]], extensor mechanisms, and the [[Popliteus Muscle|popliteus]] muscle. | ||
[[Image:Posterior knee.png|posterior view of knee joint]]<br> | [[Image:Posterior knee.png|posterior view of knee joint]]<br> | ||
Revision as of 20:40, 3 October 2018
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! {8/10/19}
Description/ definition[edit | edit source]
Knee pain is more common in the anterior, medial, and lateral aspect of the knee than in the posterior aspect of the knee. The differential diagnoses for posterior knee pain include pathology to the bones, musculotendinous structures, ligaments, and/or to the bursas. Less common are neurologic and vascular injuries. Also tumours, such as a begin tumour that contains both bone and cartilage and usually occurs near the end of a long bone (osteochondroma) or bony tumours. Tenderness of palpation over the tendons or muscles in the back of the knee can indicate muscle or tendon injury. Pain or swelling in the popliteal area suggests an effusion or cyst.
A precise understanding of knee anatomy, the physical examination and of the differential diagnosis is needed to accurately evaluate and treat posterior knee pain.[1]
Clinically Relevant Anatomy[edit | edit source]
The anatomy of the knee is important when evaluating posterior knee pain.[1] [2] There is a complicated network of muscles, ligaments, and other soft tissues around the knee that contributes to the structure and support of the joint. These include both passive and active stabilizers. Examples of passive stabilizers include the medial collateral ligament (MCL), lateral collateral ligament (LCL), anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL), while examples of active stabilizers consist of the hamstrings, extensor mechanisms, and the popliteus muscle.
SM
The semimembranosus tendon is a part of the posteromedial joint capsule, which is important in controlling anteromedial rotatory instability. (Together with the pes anserinus tendons it gives medial and posteromedial reinforcement.)[3] There is a U-shaped bursa that surrounds the distal SM tendon, separating it from the medial tibial plateau, medial (tibial) collateral ligament (MCL), and semitendinosus tendon (surrounding structures).[1]
Fig.1A demonstrates the semimembranosus tendon, with its divisions: anterior arm (Ant), direct arm (Dir), inferior arm (Inf) and the oblique popliteal ligament (OPL).
Fig.1B: The capsular arm of the semimembranosus (Caps. Sm.) intertwines with the capsular bundle of the posterior oblique ligament (Caps. POL). [13]
Mechanism of injury[edit | edit source]
The simple presence of the surrounding anatomical structures causes increased friction to the SM tendon (and irritation to the bursa) during repetitive knee flexion.[1]
Aetiology[edit | edit source]
Potential Causes of Posterior Knee Pain
| Tendinopathy, muscle strain, or trigger point (TrP) | |||
|---|---|---|---|
| Hamstrings
Gastrocnemius Popliteus |
|||
| Nerve injury (palsy) | |||
| Common peroneal nervee | |||
| Ligamentous injury (sprain or rupture |
Clinical presentation/Characteristics [edit | edit source]
Semimembranosus tendinopathy (SMT)
This is an uncommon cause of chronic posteromedial knee pain that more often occurs with older patients. It may be underdiagnosed or inadequately treated because of a lack of understanding of the condition. But timely diagnosis can lead to effective treatments.
Although tendinopathy may occur in any of the hamstrings tendons, the semimembranosus tendon is the most commonly affected. It may occur as a primary phenomenon in endurance athletes or as a secondary, overuse, compensatory condition from a primary knee abnormality, such as patellofemoral disorders.[1]
SMT usually presents as an aching pain localized to the posteromedial knee with tenderness on palpation inferior to the joint.[1] The pain is severe in its acute form, but symptoms increase with activities that involve significant hamstring activation: running, cycling, walking down stairs, climbing, or sudden deep knee flexion.[3][4]
• Hamstring Strain (HSS)
Characteristics of the hamstring strain.
Main symptoms are, a sudden sharp pain during sports activities, it can also be described as a tearing impression, and tightness, weakness and impaired range of motion.
Diagnostic Procedures[edit | edit source]
Outcomes Measures[edit | edit source]
Management / interventions[edit | edit source]
Medical therapy management
SMT
- Injection(s) of 3 mL of 2% lidocaine and 10 mg triamcinolone at the insertion site can be effective in relieving the symptoms.[3]
- Surgery to reroute and reattach the tendon is rarely needed but may be effective.[3]
Physical therapy management[edit | edit source]
- ¬SMT[3] (Evidence level: 5)
In more than 90% of the cases, this condition will heal without further intervention.
1. Initial conservative treatment includes relative rest, ice, pain-relieving modalities, a short course of NSAIDs, and physical therapy that includes hamstring strengthening and stretching exercises.
2. SMT may benefit from proper shoe fit to prevent overpronation or a medial heel lift in patients with genu valgum. Proper shoe fits are stable running shoes and shoes with motion control technology, they provide extra support preventing your ankle from rolling inwards extremely. Wearing these shoes is even more important when you are overweight. The main stability features are the medial post, the engineered heel and the plastic shank under the arch.[5][4] (Evidence level:5)
E.g. : Nike Zoom Structure Triax 15
Hamstring strain[6][7][8][9][10] - RICE-method: rest, ice, compression and elevation to speed the recovery. After the acute stages, heat can be used such as hot packs, whirlpool or heating before the stretching exercises. All the activities should be followed by ice-treatment to decrease inflammation and discomfort.
-The first phase[10] (level of evidence:5): the athlete begins pain-free submaximal isometric strengthening at multiple angles.
-Exercise: The athlete completes a set of isometric contractions at 30°, 60°, and 90° of knee flexion by placing the injured limb on top of the contralateral limb and contracting the strained hamstring. The hamstring should not be stretched into a painful range at this time but available hip and knee ROM should be maintained. Motion is also good for aligning fibres and increasing the strength of the lateral adhesion of fibres, which protects the injured fibres from stump separation. The goals of this stage are to normalize gait and to obtain knee flexion strength at greater than 50% of uninjured length upon manual muscle testing at 90 degrees of knee flexion.
-Isometric knee flexion in the seated position. Note that this would be performed at multiple angles.
- The second phase[9][10] (level of evidence:5): The athlete progressively regains strength throughout the ROM and improves neuromuscular control of the hips and pelvis in preparation for sports specific movements. End range lengthening should be avoided if painful in this stage.
Exercises: Eccentric training can be achieved using an isokinetic dynamometer if available and performing exercises such as straight leg deadlift, single leg windmills and the Nordic hamstring exercise.
(Eccentric) Single leg windmills
The patient stands with the uninjured leg on a chair or fixed surface and reaches down in a diagonal plane while keeping stance leg straight and maintaining lumbar lordosis.
It can be performed without (early) weights and progressed by using hand-held weights or kettlebells, as shown.
Nordic hamstring exercise
Having the clinician holds the patient’s feet, while in tall kneeling, performs the Nordic hamstring exercise. The patient slowly falls forward while maintaining neutral hip posture until he or she can't control descent any longer and then pushes back into starting position with upper extremities.
You can do the Nordic hamstrings exercise with elastic assistance, which means that you can replace the helper/clinician into elastic assistance attached to the wall.”
At the completion of this phase, the athlete should have full strength upon manual muscle testing (5/5) or be within 20% of the uninjured leg in the zero to 90° range when measured with a hand-held or isokinetic dynamometer in order to progress to the next phase. The athlete should also be able to jog both forward and backward without pain at a moderate speed at this point.
- The third phase[10] (Evidence level:5): Focus is on functional movements and eccentric strengthening in the lengthened state. Plyometric and sports specific training may be initiated as well as advanced balance exercise. Alternative lengthened state eccentric training may also be achieved without a dynamometer by keeping the involved thigh on the subject's chest while resisting an outside force with an elastic resistance like a thera-Band, cable column, or manual resistance.
Lengthened state eccentric training on the Biodex.
Using a setup, the Biodex may be modified so that the patient is in hip flexion and then passively extends and flexes the knee into the end range of motion. The patient resists the passive motion as the knee is extended.
Lengthened state eccentric training on cable column.
This exercise may be performed by having the patient lay supine pulling knee snugly into chest while hooked up to cable column or elastic resistance. The patient then uses his or her arms to pull the knee into flexion and then slowly eccentrically resists the cable or elastic band as it pulls the knee into extension. At the completion of this stage, the athlete should have full strength throughout the range of motion and should be able to confidently perform all sport-related tasks without limitation.
Differential Diagnosis[edit | edit source]
Posterior knee pain can be caused by a number of conditions:
- Semimembranosus tendinopathy
- Biceps femoris tendinopathy
- Hamstrings strain
- Calf strain
- M. popliteus strain
- M. popliteus tendinitis
- Posterior cruciate ligament injury
- PLC: Posterolateral corner/ posterior complex
- Knee Bursitis
- Common peroneal nerve injury
- Baker Bursitis
- popliteal artery entrapment syndrome, aneurysms
- Deep venous thrombosis (DVT)
Posterior knee pain can also be referred pain, such as from ☃☃intra-articular hip pathology, lumbar facet arthropathy, sacroiliajointin dysfunction, and sacral radiculopathy. Or it can be caused by peripheral neurological injury and entrapment of nerves in the popliteal fossa.[1]
Key Evidence[edit | edit source]
Resources[edit | edit source]
References [edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 English S, Perret D. Posterior knee pain. Current reviews in musculoskeletal medicine. 2010 Oct 1;3(1-4):3-10.
- ↑ http://www.eorthopod.com/content/popliteal-cysts
- ↑ 3.0 3.1 3.2 3.3 3.4 Darlene Hertling, Randolph M. Kessler, “Management Of Common Musculoskeletal Disorders: Physical Therapy Principles and Methodes” (fourth edition), LippinCott Williams & Wilkins
- ↑ 4.0 4.1 Proper shoe fit: http://walking.about.com/od/prshoe/tp/shoemotion.htm
- ↑ Proper shoe fit: http://www.runningshoesguru.com/2012/02/5-best-stability-running-shoes/
- ↑ SANDRA J. SHULTZ, PEGGY A. HOUGLUM EN DAVID H. PERRIN. Examination of musculoskeletal injuries, third edition, Human Kinetics, 2010, 696 pages.
- ↑ OHN C. GRIFFIN, Client-centered exercise prescription, Human Kinetics, 1998, 263 pages.
- ↑ STEVEN J. FLECK, WILLIAM J. KRAEMER, Designing resistance-training programs, second edition, Human Kinetics, 1997, 275 pages.
- ↑ 9.0 9.1 DANIEL LORENZ, MICHAEL REIMAN, The role and implementation of eccentric training in athletic rehabilitation: tendinopathy, hamstring strains and ACL reconstruction, pubmed, march 2011, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3105370/, 27/11/2012, (evidence level 5).
- ↑ 10.0 10.1 10.2 10.3 BRANDON SCHMITT, TYLER TIM AND MALACHY MCHUGH, Hamstring injury rehabilitation and prevention of reinjury using lengthened state eccentric training: a new concept, pubmed, June 2012, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3362981/, 27/11/2012, (evidence level 5).