Pudendal Nerve
Original Editor - name here
Top Contributors - Manisha Shrestha, Lucinda hampton, Kim Jackson, Wendy Snyders and Cindy John-Chu
Description[edit | edit source]
The term 'Pudendal' comes from ( Latin pudenda, meaning “external genitals”, derived from pudendum, meaning "parts to be ashamed of[1]
The pudendal nerve is the main nerve of perineum, pelvic floor muscles and the external genitalia.[2]Benjamin Alcock first described it in 1836 while researching the internal pudendal artery's path.
The pudendal nerve is a mixed nerve having sensory, motor, and autonomic functions. It is one of the primary nerve originating from sacral plexus following sciatic nerve. The nerve is paired, meaning that it is found bilaterally, one on the left and one on the right side of the body.[3]
Course[edit | edit source]
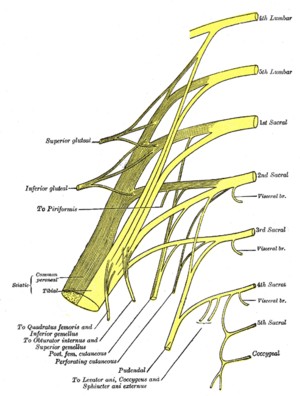
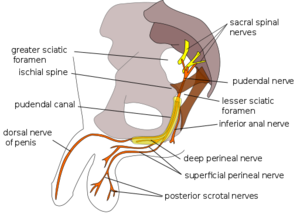
- The pudendal nerve receives input from the primary ventral roots of S2–S4 in the sacral plexus, which converge to form the nerve adjacent to the lateral wall of the pelvic cavity. It then forms 1, 2 or three trunks before its final branching; variable contributions from S1 and/or S5.
- Throughout most of its path, the nerve is closely associated with the branches of the internal pudendal artery and vein.
- exits the pelvis via the greater sciatic foramen inferior to the piriformis muscle and bends around the posterior aspect of the sacrospinous ligament.
- It courses for a very short distance within the gluteal region where it bends around the sacrospinous ligament to enter the perineum through the lesser sciatic foramen.
- While in the gluteal region the pudendal nerve is proximal to the ischial spine where it is the target of a pudendal nerve block.[3]
- Compressive nerve diseases are usually identified at the interligamentous section of its journey, which is when it is dorsal to the sacrospinous ligament and ventral to the sacrotuberous ligament.[2]
- After exiting the lesser sciatic foramen and entering the perineum, the nerve passes through a sheath of connective tissue on the medial wall of the obturator internus muscle called the pudendal (Alcock’s) canal.
- It continues to course through the pudendal canal, giving off three consecutive branches on its path towards the pubic symphysis.
- The pudendal nerve gives rise to the inferior anal nerve as soon as it enters the canal (also called the inferior rectal nerve).
- When it reaches the distal portion of the canal, the nerve bifurcates and gives rise to two more branches: the perineal nerve and the dorsal nerve of the penis/clitoris.
Root[edit | edit source]
S2,S3,S4
Branches[edit | edit source]
There are three main branches of the pudendal nerve. They are:
- Inferior rectal branch
- Perineal branch: which is divided into superficial and deep perineal nerve, which further divides into medial and posterolateral scrotal/labial nerve.
- Dorsal branch of penis/clitoris
Function[edit | edit source]
Motor[edit | edit source]
Sensory[edit | edit source]
Clinical relevance[edit | edit source]
- Pudendal Neuralgia
- Pudental Nerve Entrapment Syndrome
- Pudental Nerve Injury
Assessment[edit | edit source]
History[edit | edit source]
Common causes for pudendal nerve injury include:
- Prolonged sitting (e.g., seamstress, computer operators, judges, concert pianists, locomotive engineers)
- Repetitive hip flexion (sports activities, exercising, jogging, cycling)
- Direct trauma includes falls, motor vehicle accidents, vaginal delivery and pelvic surgeries, especially when using mesh (eg: surgeries for urinary incontinences, total abdominal hysterectomy)
- Radiation therapy especially in males treated for prostate cancer and patients treated for rectal and gynecological cancers[5]
Pain Assessment[edit | edit source]
- Patient with pelvic pain (especially perineal and genital) with or without concurrent sexual, bladder, or bowel symptoms
- Gradual onset of pain except for acute trauma
- Pain is less in morning and progress with progression of the day
- Type of pain is usually burning pain , but may also experience tingling, aching, stabbing, and shock-like pain
- Pain aggravates while sitting and relieves when standing, lying down, or seated on a toilet.
- Pain distribution may be limited or extensive and may include the vulva, vagina, clitoris, perineum, and rectum in females; glans penis, scrotum, perineum, and rectum in males
- Other symptoms associated with PN include urinary frequency, urgency, symptoms mimicking interstitial cystitis, painful ejaculation, dyspareunia, painful nocturnal orgasms, and persistent sexual arousal.
- Foreign body sensation[6]
Physical Examination
- Sensory
- Motor
- Autonomic
Treatment[edit | edit source]
Resources[edit | edit source]
References[edit | edit source]
- ↑ Harper, Douglas. "Pudendum". Online Etymology Dictionary.
- ↑ 2.0 2.1 Rojas-Gómez MF, Blanco-Dávila R, Tobar-Roa V, Gómez-González AM, Ortiz-Zableh AM, Ortiz-Azuero A. https://www.researchgate.net/publication/318085947_Regional_anesthesia_guided_by_ultrasound_in_the_pudendal_nerve_territory Colombian Journal of Anestesiology. 2017 Sep;45(3):200-9.
- ↑ 3.0 3.1 Kinter KJ, Newton BW. Anatomy, abdomen and pelvis, pudendal nerve. InStatPearls [Internet] 2021 Sep 13. StatPearls Publishing.
- ↑ Causes of Pudendal Neuralgia. Available from: https://www.youtube.com/watch?v=mLvwV_Tfas4 lasted accessed: 27th June 2022
- ↑ Soon-Sutton TL, Feloney MP, Antolak S. Pudendal neuralgia. InStatPearls [Internet] 2021 Jul 31. StatPearls Publishing.
- ↑ Kaur J, Singh P. Pudendal nerve entrapment syndrome.