Respiratory Assessment: Difference between revisions
(EDIT) |
No edit summary |
||
| (20 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
== | <div class=“noeditbox”> | ||
This article is currently under review and may not be up to date. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}}) | |||
</div> | |||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|Mandeepa Kumawat]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== Introduction == | |||
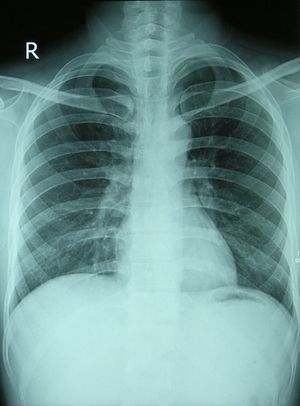
[[File:Chest X-ray 2346.jpg|thumb]]Respiratory conditions can affect breathing either through damage to the lungs or excess [[Sputum|secretions]]. To ensure that the correct treatment is implemented, a thorough respiratory assessment should include both a comprehensive subjective and objective component to get a complete understanding of the client's function and baseline.<ref>Mikelsons, C. (2008). The role of physiotherapy in the management of COPD. Respiratory Medicine: COPD Update, 4(1), 2–7 Available at https://www.semanticscholar.org/paper/The-role-of-physiotherapy-in-the-management-of-COPD-Mikelsons/e333d7621a7fddb06be0ff219e2336c352fe335c</ref><ref>Cross J, Harden B, Broad MA, Quint M, Paul Ritson MC, Thomas S. Respiratory physiotherapy: An on-call survival guide. Elsevier Health Sciences; 2008 Nov 25.</ref> | |||
== Subjective Assessment == | |||
The subjective assessment is an important part of the client experience. It allows the client to express their symptoms from their viewpoint and helps to guide the objective assessment and plan a treatment programme with the clients needs at the forefront. Each subjective assessment should include the following components.<ref name=":0">Hough A. Physiotherapy in respiratory care: a problem-solving approach to respiratory and cardiac management. Springer; 2013 Nov 11.</ref><ref name=":1">Main E, Denehy L. Cardiorespiratory Physiotherapy: Adults and Paediatrics 5th Edition. Elsevier; 2016 Jul 5.</ref> | |||
* Patient's main concerns. | |||
=== History of Present Illness === | |||
* Site, Intensity, Type, Aggravating factor and Relieving factor (SITAR) | |||
* Onset - sudden or gradual | |||
* Location - radiating | |||
* Duration - frequency or chronology (seasonal or daily variations) | |||
* Characteristics - quality or severity | |||
* Current situation - improving or deteriorating | |||
* Effect on activity of daily living (ADL) | |||
* Previous diagnosis of similar episodes | |||
* Previous treatment and efficacy | |||
=== Past Medical History === | |||
* Thoracic, nasal, pharyngeotracheal, trauma or surgery, hospitalisation for pulmonary disorders. | |||
* Use of ventilation - assisting devices | |||
* Respiratory disorders: Asthma, [[Bronchiectasis]], [[COPD (Chronic Obstructive Pulmonary Disease)|COPD]]- TB, [[bronchitis]], [[emphysema]], | |||
* Other chronic disorders - cardiac, cancer, blood clotting disorders | |||
* Allergies | |||
* Immunisation (pneumococcal, influenza) | |||
* Diabetes Mellitus/ [[Tuberculosis]]/ Blood pressure/ [[asthma]] | |||
=== Surgical History === | |||
* Endoscopy, tracheostomy, lobectomy | |||
=== Personal and social history === | |||
* Sleep | |||
* Appetite, weight loss | |||
* Bowel and bladder | |||
* Smoking | |||
* Exercise tolerance | |||
* Home environment | |||
* Economic condition - poor / fair / good | |||
* Exercise tolerance | |||
== Cardinal Signs and Symptoms == | |||
=== Cough === | |||
* Onset: sudden or gradual<ref>Raj, A. A., & Birring, S. S. (2007). Clinical assessment of chronic cough severity. Pulmonary Pharmacology & Therapeutics, 20(4), 334–337.</ref> | |||
* Duration: | |||
** Acute < 3 weeks | |||
** Persistent >3 weeks<ref>NHS Cough Available at:https://www.nhs.uk/conditions/cough/ (Accessed 22nd November 2020)</ref> | |||
** Chronic > 8 weeks<ref>Mayo Clinic. Chronic Cough. Available at<nowiki/>https://www.mayoclinic.org/diseases-conditions/chronic-cough/symptoms-causes/syc-20351575 (Accessed 22nd November 2020)</ref> | |||
* Nature: Dry irritation; Wet signs of infection | |||
* Type: Mucoid; Mucopurulent TB; Frothy [[Pulmonary Oedema|pulmonary oedema]]; Rusty (blood) TB , lobar [[pneumonia]] | |||
* Odour: foul infection | |||
* Productive of sputum | |||
* Are they regularly clearing their throat. | |||
=== Sputum === | |||
* Amount | |||
* Normal - 100 ml of tracheobronchial secretions are produced daily and cleared subconsciously | |||
=== Colour === | |||
{| class="wikitable" | |||
!'''Colour''' | |||
!Potential cause | |||
|- | |||
|Blood Streaked | |||
|inflammation of throat (larynx, trachea) or bronchi, lung cancer, ulcers | |||
|- | |||
|Pink | |||
|blood formed from alveoli and small peripheral bronchi | |||
|- | |||
|Copious amounts of blood | |||
|cavitary TB , lung abscess ,bronchiectasis , lung infarction , pulmonary embolism | |||
|- | |||
|Green or greenish | |||
|possible infection | |||
|- | |||
|Rust | |||
== | |pneumococcal bacteria , [[Tuberculosis|pulmonary TB]] | ||
|- | |||
|Brownish | |||
|[[Bronchitis|chronic bronchitis]] (greenish / yellowish / brown), chronic pneumonia (whitish - brown) | |||
|- | |||
|Yellowish purulen | |||
|pus - haemophilus | |||
|- | |||
|Yellowish/green (mucopurulent) | |||
|bronchiectasis, [[Cystic Fibrosis|cystic fibrosis]], [[pneumonia]] | |||
|- | |||
|Whitish grey | |||
|chronic allergic bronchitis | |||
|- | |||
|White, milky or opaque (mucoid) | |||
|viral infection or allergy (asthma) | |||
|- | |||
|Foamy white | |||
|earlier phase - [[Pulmonary Oedema|pulmonary oedema]] | |||
|- | |||
|Frothy pink | |||
|severe pulmonary oedema | |||
|- | |||
|Black/ black specks | |||
|smoke inhalation (fires, tobacco, heroin), coal dust | |||
|} | |||
Yellowish | |||
=== Breathlessness === | |||
The physiotherapist should always relate breathlessness to the level of function that the patient can achieve | The physiotherapist should always relate breathlessness to the level of function that the patient can achieve | ||
* Exercise tolerance ( | * Exercise tolerance (e.g. number of stairs client can climb or can walk) | ||
* Shortness of breath at rest | * Shortness of breath at rest | ||
| Line 102: | Line 115: | ||
* Associated swelling of ankles or recent weight gain | * Associated swelling of ankles or recent weight gain | ||
* Activities : Sudden ( pneumothorax , pulmonary embolism , DVT ) | * Activities : Sudden ([[pneumothorax]], [[Pulmonary Embolism|pulmonary embolism]], [[Deep Vein Thrombosis|DVT]]) | ||
* Constant breathlessness (fibrosis, fluid) | |||
==== Grading Breathlessness ==== | |||
=== | * New York Heart Association (NYHA) | ||
*# Grade 1 - no symptoms and limitation in ordinary physical activity | |||
== | *# Grade 2 - mild symptoms , angina and slight limitation in ordinary activities | ||
*# Grade 3 - marked limitation in activity due to symptom , even during less than ordinary activity . | |||
Grade 1 - no symptoms and limitation in ordinary physical activity | *# Grade 4 - severe limitation , experience symptoms even at rest mostly bed bound patient | ||
* Modified Medical Research Council (MMRC) | |||
Grade 2 - mild symptoms , angina and slight limitation in ordinary activities | ** Grade 0 - no dyspnea except with strenuous exercise | ||
** Grade 1- dyspnea when walking up on the hill or hurrying on the level | |||
Grade 3 - marked limitation in activity due to symptom , even during less than ordinary activity . | ** Grade 2 - walks slower than most on the level or stops after 15 minutes of walking on the level. | ||
** Grade 3 - stops after few minutes of walking on the level. | |||
Grade 4 - severe limitation , experience symptoms even at rest mostly bed bound patient | ** Grade 4- dyspnea with minimal activity such as getting dressed or too dyspneic to leave the house. | ||
Grade 0 - no dyspnea except with | |||
Grade 1- dyspnea when walking up on the hill or hurrying on the level | |||
Grade 2 - walks slower than most on the level or stops after 15 minutes of | |||
Grade 3 - stops after few minutes of walking on the level. | |||
Grade 4- dyspnea with minimal activity such as getting dressed or too dyspneic to leave the house. | |||
2. | * American Thoracic Society (ATS) | ||
** Grade 0- none - no trouble of dyspnea on level / uphill | |||
** Grade 1 - mild - dyspnea on at level / uphill. | |||
** Grade 2 - moderate - walks slower than person of same age | |||
** Grade 3 - severe - stops after 100 yards | |||
** Grade 4 - very severe - breathlessness | |||
* [[Borg Rating Of Perceived Exertion|Modified BORG Dyspnoea Scal]]<nowiki/>e - Patients are asked "How much difficulty is your breathing causing you right now?” 0 Nothing at all, 0.5 Very, very slight (just noticeable), 1 Very slight, 2 Slight, 3 Moderate, 4 Somewhat severe, 5 Severe, 7 Very severe, 9 Very, very severe (almost maximal), 10 Maximal. <ref>Heart Online. Rating of perceived exertion: Borg scales. Available at: https://www.sralab.org/sites/default/files/2018-04/Rating_of_perceived_exertion_-_Borg_scale.pdf (Accessed 22nd November 2020)</ref> | |||
=== Chest Pain === | |||
Chest pain in respiratory patients usually originate from musculoskeletal , pleural or tracheal inflammation as lung parenchyma and small airways contain no pain fibres. Pain relief can be achieved by heat, splinting or pain medication. Typical examples of the causes of chest pain include: | |||
* Pleuritic chest pain | |||
* Tracheitis | |||
* Musculoskeletal (chest wall) pain | |||
* Angina pectoris | |||
* Pericarditis | |||
=== Incontinence === | |||
Coughing and huffing increases intra - abdominal pressure which may precipitate urinary leakage | |||
=== Other Symptoms === | |||
* Fever (pyrexia) | |||
* Headache - morning headache - nocturnal CO2 retention | |||
* Peripheral oedema - right heart failure | |||
* Shivering | |||
* Weight loss | |||
* Palpitations | |||
* Vomiting and nausea | |||
* Gastro intestinal reflex | |||
== Objective Assessment == | |||
Once the subjective assessment has been completed there will indicators on what to look for during the objective assessment. A thorough and detailed objective assessment will assist with the planning and management of an individualised treatment programme that focuses on the presentation and needs of the client.<ref name=":0" /><ref name=":1" /> | |||
=== General Examination === | |||
==== Vital signs ==== | |||
* Temperature | |||
* Pulse | |||
* Respiratory rate | |||
* Blood pressure | |||
* Oxygen saturation (SpO2) | |||
==== General Appearance ==== | |||
* Body weight - BMI and weight in kg | |||
* Height | |||
* Nails - clubbing | |||
* Eyes - pallor (anaemia); Plethora (high haemoglobin); Jaundice (yellow color due to liver or blood disturbance) | |||
* Tongue and mouth - Cyanosis - [[Hypoxaemia|hypoxemia]] | |||
* Jugular venous pressure - increased in right heart failure , chronic lung disease , dehydrated patient | |||
* Peripheral oedema - seen in decreased albumin level , impaired venous or lymphatic function , increased steroids | |||
* Pressure sores (in bedbound patients) | |||
==== Observation of Chest ==== | |||
* Tranverse diameter > AP Diameter | |||
* Kyphosis | |||
* Kyphoscoliosis - restrictive lung defect | |||
* Pectus carinatum - pigeon chest | |||
* Hyperinflation or barrel chest - AP = transverse - ribs horizontal | |||
==== Breathing Pattern ==== | |||
* Typical rate - 12 to 16 breath per minute | |||
* Typical Inspiratory : expiratory ratio = 1:1.5 to 1:2 | |||
* Check for bradypnea, tachypnea, hyperventilation | |||
* Prolonged expiration - 1:3 to 1:4 | |||
* Pursed lip breathing | |||
* Apnoea | |||
* Hypopnea | |||
* Kaussamaul ‘s respiration - metabolic acidosis | |||
* Cheyne strokes respiration - drugs ( narcotics) , heart failure , neurological disturbances | |||
* Ataxic breathing - cerebellar disease | |||
* Apneutic breathing - brain damage | |||
* Thoracoabdominal - female ; abdominothoracic | |||
==== ICU Patients ==== | |||
* Mode of ventilation - supplemental oxygen; intermitent positive pressure ventilation | |||
* Route of ventilation - face mask, nasal cannula, endotracheal tube, tracheostomy | |||
* Level of consciousness - measured with Glasgow coma scale | |||
* Central venous pressure (CVP) and pulmonary artery pressure (PAP) | |||
==== Palpation ==== | |||
* [[Trachea and Larynx|Trachea]] - tracheal deviation indicates underlying mediasternal shift . trachea may be pulled towards in collapsed or fibrosed upper lobe or pushed away from [[pneumothorax]] or large pleural effusion. | |||
* Measuring Chest Expansion (using a tape measure) Technique at residual volume, the examiner ‘s hands are placed spanning the posterolateral segment of both bases, with the thumbs touching in the midline posteriorly, both the sides should move equally with 3 - 5cm being the normal displacement. | |||
** Supramammary - 1.5cm | |||
** Mammary - 1.5cm | |||
** Inframammary - 1cm | |||
* Hoover’s sign - Paradoxical movement of the lower chest can occur in patients with severe chronic airflow limitation who are extremely hyperinflated. As the dome of the diaphragm cannot descend any further diaphragm contraction during inspiration pulls the lower ribs inwards. | |||
* Vocal Fremitus It is the measure of speech vibrations transmitted through the chest wall to the examiner’ s hands. It is the measure by asking the patient to repeatedly say ‘ggg’ or 111 whilst the examiner`s hands are placed flat on both sides of the chest | |||
** Increase in patient whose lung underneath is relatively solid (consolidated) | |||
** Decrease in patient - pneumothorax or pleural effusion | |||
* [[Percussion]] It is performed by placing the left hand firmly on the chest wall so that the finger have good contact with the skin . the middle finger of the left hand is struck over the DIP joint with the middle finger of the right hand . for all the positions , percuss at 4 to 5 cm intervals over the intercostal spaces , moving systematically from superior to inferior and medial to lateral | |||
* Resonance - the expected sound can usually be heard over all areas of the lungs. | |||
** Hyper resonance - associated with hyperinflation may indicate emphysema , pneumothorax or asthma. | |||
** Dullness or flatness - pneumonia , atelactasis , pleural effusion , pneumothorax or asthma. | |||
** Tympany - sound usually associated with percussion over the abdomen | |||
* [[Auscultation]] with the stethoscope provides important information to the condition of the lungs and pleura. All sounds can be characterised in the same manner as the percussion notes, intensity, pitch, quality and duration. | |||
** Normal breath sounds bronchial, vesicular | |||
** Abnormal breath sounds - crackles, rhonchi, wheeze, pleural friction rub | |||
** Vocal resonance - Decrease in resonance - emphysema , pneumothorax , pleural thickening or pleural effusion. | |||
** Heart sounds | |||
*** 1st - closure of mitral and tricuspid valve. | |||
*** 2nd - closure of pulmonary and aortic valves. | |||
*** 3rd - cardiac failure | |||
*** 4th - heart failure , hypertension , aortic valve disease | |||
== Diagnostics == | |||
There are many different tests that can assist in diagnosing respiratory conditions and help implement and guide the best treatment options. | |||
=== [[Spirometry]] === | |||
This is a simple respiratory test that measures the forced expiratory volume in 1 second (FEV) , the forced vital capacity ( FVC ) and peak expiratory flow rate (PEFR) are important measures of ventilatory function.<ref>Miller MR, Hankinson J, Brusasco V et al (2005) Standardisation of spirometry. Eur Respir J 26(2):319–338</ref> | |||
=== [[Arterial Blood Gases]] === | |||
ABG provide an accurate measure of O2 uptake and CO2 removal by the respiratory system as a whole. Typical values are listed below: | |||
* pH : 7.35 TO 7.45 | |||
* PaO2: 10.7 to 13.3 kPa (80 - 100 mmHg) | |||
* PaCO2: 4.7 TO 6.0 KPa (35 to 45 mm hg) | |||
* HCO3: 22 - 26 MMOL / L | |||
* Base excess : -2 to +2 | |||
=== [[Chest X-Rays|Chest X-ray]] === | |||
Chest x-rays are often taken early if a respiratory disorder is suspected. As well as revealing the condition of the lungs they can also diagnose: | |||
* Pneumonia | |||
* Emphysema | |||
* Mass or nodule in the lung | |||
* Pleural effusion (fluid around the lung) | |||
* Rib fracture | |||
* Tuberculosis | |||
* Congestive heart failure | |||
* Enlarged heart | |||
== References == | |||
<references /> | |||
[[Category:Cardiopulmonary]] | |||
[[Category:Respiratory System - Assessment and Examination]] | |||
[[Category:Respiratory]] | |||
[[Category:Respiratory Disease]] | |||
Latest revision as of 05:51, 17 November 2021
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (17/11/2021)
Introduction[edit | edit source]
Respiratory conditions can affect breathing either through damage to the lungs or excess secretions. To ensure that the correct treatment is implemented, a thorough respiratory assessment should include both a comprehensive subjective and objective component to get a complete understanding of the client's function and baseline.[1][2]
Subjective Assessment[edit | edit source]
The subjective assessment is an important part of the client experience. It allows the client to express their symptoms from their viewpoint and helps to guide the objective assessment and plan a treatment programme with the clients needs at the forefront. Each subjective assessment should include the following components.[3][4]
- Patient's main concerns.
History of Present Illness[edit | edit source]
- Site, Intensity, Type, Aggravating factor and Relieving factor (SITAR)
- Onset - sudden or gradual
- Location - radiating
- Duration - frequency or chronology (seasonal or daily variations)
- Characteristics - quality or severity
- Current situation - improving or deteriorating
- Effect on activity of daily living (ADL)
- Previous diagnosis of similar episodes
- Previous treatment and efficacy
Past Medical History[edit | edit source]
- Thoracic, nasal, pharyngeotracheal, trauma or surgery, hospitalisation for pulmonary disorders.
- Use of ventilation - assisting devices
- Respiratory disorders: Asthma, Bronchiectasis, COPD- TB, bronchitis, emphysema,
- Other chronic disorders - cardiac, cancer, blood clotting disorders
- Allergies
- Immunisation (pneumococcal, influenza)
- Diabetes Mellitus/ Tuberculosis/ Blood pressure/ asthma
Surgical History[edit | edit source]
- Endoscopy, tracheostomy, lobectomy
Personal and social history[edit | edit source]
- Sleep
- Appetite, weight loss
- Bowel and bladder
- Smoking
- Exercise tolerance
- Home environment
- Economic condition - poor / fair / good
- Exercise tolerance
Cardinal Signs and Symptoms[edit | edit source]
Cough[edit | edit source]
- Onset: sudden or gradual[5]
- Duration:
- Nature: Dry irritation; Wet signs of infection
- Type: Mucoid; Mucopurulent TB; Frothy pulmonary oedema; Rusty (blood) TB , lobar pneumonia
- Odour: foul infection
- Productive of sputum
- Are they regularly clearing their throat.
Sputum[edit | edit source]
- Amount
- Normal - 100 ml of tracheobronchial secretions are produced daily and cleared subconsciously
Colour[edit | edit source]
| Colour | Potential cause |
|---|---|
| Blood Streaked | inflammation of throat (larynx, trachea) or bronchi, lung cancer, ulcers |
| Pink | blood formed from alveoli and small peripheral bronchi |
| Copious amounts of blood | cavitary TB , lung abscess ,bronchiectasis , lung infarction , pulmonary embolism |
| Green or greenish | possible infection |
| Rust | pneumococcal bacteria , pulmonary TB |
| Brownish | chronic bronchitis (greenish / yellowish / brown), chronic pneumonia (whitish - brown) |
| Yellowish purulen | pus - haemophilus |
| Yellowish/green (mucopurulent) | bronchiectasis, cystic fibrosis, pneumonia |
| Whitish grey | chronic allergic bronchitis |
| White, milky or opaque (mucoid) | viral infection or allergy (asthma) |
| Foamy white | earlier phase - pulmonary oedema |
| Frothy pink | severe pulmonary oedema |
| Black/ black specks | smoke inhalation (fires, tobacco, heroin), coal dust |
Breathlessness[edit | edit source]
The physiotherapist should always relate breathlessness to the level of function that the patient can achieve
- Exercise tolerance (e.g. number of stairs client can climb or can walk)
- Shortness of breath at rest
- Association of paraoxysmal nocturnal dyspnea (PND)
- Associated swelling of ankles or recent weight gain
- Activities : Sudden (pneumothorax, pulmonary embolism, DVT)
- Constant breathlessness (fibrosis, fluid)
Grading Breathlessness[edit | edit source]
- New York Heart Association (NYHA)
- Grade 1 - no symptoms and limitation in ordinary physical activity
- Grade 2 - mild symptoms , angina and slight limitation in ordinary activities
- Grade 3 - marked limitation in activity due to symptom , even during less than ordinary activity .
- Grade 4 - severe limitation , experience symptoms even at rest mostly bed bound patient
- Modified Medical Research Council (MMRC)
- Grade 0 - no dyspnea except with strenuous exercise
- Grade 1- dyspnea when walking up on the hill or hurrying on the level
- Grade 2 - walks slower than most on the level or stops after 15 minutes of walking on the level.
- Grade 3 - stops after few minutes of walking on the level.
- Grade 4- dyspnea with minimal activity such as getting dressed or too dyspneic to leave the house.
- American Thoracic Society (ATS)
- Grade 0- none - no trouble of dyspnea on level / uphill
- Grade 1 - mild - dyspnea on at level / uphill.
- Grade 2 - moderate - walks slower than person of same age
- Grade 3 - severe - stops after 100 yards
- Grade 4 - very severe - breathlessness
- Modified BORG Dyspnoea Scale - Patients are asked "How much difficulty is your breathing causing you right now?” 0 Nothing at all, 0.5 Very, very slight (just noticeable), 1 Very slight, 2 Slight, 3 Moderate, 4 Somewhat severe, 5 Severe, 7 Very severe, 9 Very, very severe (almost maximal), 10 Maximal. [8]
Chest Pain[edit | edit source]
Chest pain in respiratory patients usually originate from musculoskeletal , pleural or tracheal inflammation as lung parenchyma and small airways contain no pain fibres. Pain relief can be achieved by heat, splinting or pain medication. Typical examples of the causes of chest pain include:
- Pleuritic chest pain
- Tracheitis
- Musculoskeletal (chest wall) pain
- Angina pectoris
- Pericarditis
Incontinence[edit | edit source]
Coughing and huffing increases intra - abdominal pressure which may precipitate urinary leakage
Other Symptoms[edit | edit source]
- Fever (pyrexia)
- Headache - morning headache - nocturnal CO2 retention
- Peripheral oedema - right heart failure
- Shivering
- Weight loss
- Palpitations
- Vomiting and nausea
- Gastro intestinal reflex
Objective Assessment[edit | edit source]
Once the subjective assessment has been completed there will indicators on what to look for during the objective assessment. A thorough and detailed objective assessment will assist with the planning and management of an individualised treatment programme that focuses on the presentation and needs of the client.[3][4]
General Examination[edit | edit source]
Vital signs[edit | edit source]
- Temperature
- Pulse
- Respiratory rate
- Blood pressure
- Oxygen saturation (SpO2)
General Appearance[edit | edit source]
- Body weight - BMI and weight in kg
- Height
- Nails - clubbing
- Eyes - pallor (anaemia); Plethora (high haemoglobin); Jaundice (yellow color due to liver or blood disturbance)
- Tongue and mouth - Cyanosis - hypoxemia
- Jugular venous pressure - increased in right heart failure , chronic lung disease , dehydrated patient
- Peripheral oedema - seen in decreased albumin level , impaired venous or lymphatic function , increased steroids
- Pressure sores (in bedbound patients)
Observation of Chest[edit | edit source]
- Tranverse diameter > AP Diameter
- Kyphosis
- Kyphoscoliosis - restrictive lung defect
- Pectus carinatum - pigeon chest
- Hyperinflation or barrel chest - AP = transverse - ribs horizontal
Breathing Pattern[edit | edit source]
- Typical rate - 12 to 16 breath per minute
- Typical Inspiratory : expiratory ratio = 1:1.5 to 1:2
- Check for bradypnea, tachypnea, hyperventilation
- Prolonged expiration - 1:3 to 1:4
- Pursed lip breathing
- Apnoea
- Hypopnea
- Kaussamaul ‘s respiration - metabolic acidosis
- Cheyne strokes respiration - drugs ( narcotics) , heart failure , neurological disturbances
- Ataxic breathing - cerebellar disease
- Apneutic breathing - brain damage
- Thoracoabdominal - female ; abdominothoracic
ICU Patients[edit | edit source]
- Mode of ventilation - supplemental oxygen; intermitent positive pressure ventilation
- Route of ventilation - face mask, nasal cannula, endotracheal tube, tracheostomy
- Level of consciousness - measured with Glasgow coma scale
- Central venous pressure (CVP) and pulmonary artery pressure (PAP)
Palpation[edit | edit source]
- Trachea - tracheal deviation indicates underlying mediasternal shift . trachea may be pulled towards in collapsed or fibrosed upper lobe or pushed away from pneumothorax or large pleural effusion.
- Measuring Chest Expansion (using a tape measure) Technique at residual volume, the examiner ‘s hands are placed spanning the posterolateral segment of both bases, with the thumbs touching in the midline posteriorly, both the sides should move equally with 3 - 5cm being the normal displacement.
- Supramammary - 1.5cm
- Mammary - 1.5cm
- Inframammary - 1cm
- Hoover’s sign - Paradoxical movement of the lower chest can occur in patients with severe chronic airflow limitation who are extremely hyperinflated. As the dome of the diaphragm cannot descend any further diaphragm contraction during inspiration pulls the lower ribs inwards.
- Vocal Fremitus It is the measure of speech vibrations transmitted through the chest wall to the examiner’ s hands. It is the measure by asking the patient to repeatedly say ‘ggg’ or 111 whilst the examiner`s hands are placed flat on both sides of the chest
- Increase in patient whose lung underneath is relatively solid (consolidated)
- Decrease in patient - pneumothorax or pleural effusion
- Percussion It is performed by placing the left hand firmly on the chest wall so that the finger have good contact with the skin . the middle finger of the left hand is struck over the DIP joint with the middle finger of the right hand . for all the positions , percuss at 4 to 5 cm intervals over the intercostal spaces , moving systematically from superior to inferior and medial to lateral
- Resonance - the expected sound can usually be heard over all areas of the lungs.
- Hyper resonance - associated with hyperinflation may indicate emphysema , pneumothorax or asthma.
- Dullness or flatness - pneumonia , atelactasis , pleural effusion , pneumothorax or asthma.
- Tympany - sound usually associated with percussion over the abdomen
- Auscultation with the stethoscope provides important information to the condition of the lungs and pleura. All sounds can be characterised in the same manner as the percussion notes, intensity, pitch, quality and duration.
- Normal breath sounds bronchial, vesicular
- Abnormal breath sounds - crackles, rhonchi, wheeze, pleural friction rub
- Vocal resonance - Decrease in resonance - emphysema , pneumothorax , pleural thickening or pleural effusion.
- Heart sounds
- 1st - closure of mitral and tricuspid valve.
- 2nd - closure of pulmonary and aortic valves.
- 3rd - cardiac failure
- 4th - heart failure , hypertension , aortic valve disease
Diagnostics[edit | edit source]
There are many different tests that can assist in diagnosing respiratory conditions and help implement and guide the best treatment options.
Spirometry[edit | edit source]
This is a simple respiratory test that measures the forced expiratory volume in 1 second (FEV) , the forced vital capacity ( FVC ) and peak expiratory flow rate (PEFR) are important measures of ventilatory function.[9]
Arterial Blood Gases[edit | edit source]
ABG provide an accurate measure of O2 uptake and CO2 removal by the respiratory system as a whole. Typical values are listed below:
- pH : 7.35 TO 7.45
- PaO2: 10.7 to 13.3 kPa (80 - 100 mmHg)
- PaCO2: 4.7 TO 6.0 KPa (35 to 45 mm hg)
- HCO3: 22 - 26 MMOL / L
- Base excess : -2 to +2
Chest X-ray[edit | edit source]
Chest x-rays are often taken early if a respiratory disorder is suspected. As well as revealing the condition of the lungs they can also diagnose:
- Pneumonia
- Emphysema
- Mass or nodule in the lung
- Pleural effusion (fluid around the lung)
- Rib fracture
- Tuberculosis
- Congestive heart failure
- Enlarged heart
References[edit | edit source]
- ↑ Mikelsons, C. (2008). The role of physiotherapy in the management of COPD. Respiratory Medicine: COPD Update, 4(1), 2–7 Available at https://www.semanticscholar.org/paper/The-role-of-physiotherapy-in-the-management-of-COPD-Mikelsons/e333d7621a7fddb06be0ff219e2336c352fe335c
- ↑ Cross J, Harden B, Broad MA, Quint M, Paul Ritson MC, Thomas S. Respiratory physiotherapy: An on-call survival guide. Elsevier Health Sciences; 2008 Nov 25.
- ↑ 3.0 3.1 Hough A. Physiotherapy in respiratory care: a problem-solving approach to respiratory and cardiac management. Springer; 2013 Nov 11.
- ↑ 4.0 4.1 Main E, Denehy L. Cardiorespiratory Physiotherapy: Adults and Paediatrics 5th Edition. Elsevier; 2016 Jul 5.
- ↑ Raj, A. A., & Birring, S. S. (2007). Clinical assessment of chronic cough severity. Pulmonary Pharmacology & Therapeutics, 20(4), 334–337.
- ↑ NHS Cough Available at:https://www.nhs.uk/conditions/cough/ (Accessed 22nd November 2020)
- ↑ Mayo Clinic. Chronic Cough. Available athttps://www.mayoclinic.org/diseases-conditions/chronic-cough/symptoms-causes/syc-20351575 (Accessed 22nd November 2020)
- ↑ Heart Online. Rating of perceived exertion: Borg scales. Available at: https://www.sralab.org/sites/default/files/2018-04/Rating_of_perceived_exertion_-_Borg_scale.pdf (Accessed 22nd November 2020)
- ↑ Miller MR, Hankinson J, Brusasco V et al (2005) Standardisation of spirometry. Eur Respir J 26(2):319–338