Shoulder Special Tests: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Traditionally Orthopaedic Special tests were used to assist in the diagnostic process by implicating specific tissue structures that are either dysfunctional, pathological, or lack structural integrity, confirming the findings from the physical assessment and providing a tentative diagnosis.<ref name="Magee" /> Special testing is generally performed following a full examination of the [[shoulder]] that includes but is not limited to patient history, mechanism of injury, clinical observation, bony and soft tissue palpation, assessment of active and passive physiological movements, assessment of passive arthokinematic / accessory joint mobility, neurological assessment, [[Muscle Strength|manual muscle testing]], and functional assessments.<ref name="Biederwolf" /> Reproduction of pain, and weakness during these special test were considered clinically diagnostic. | |||
However, although Orthopaedic Special Tests are commonly used, findings from both narrative, systematic reviews, and research investigations have consistently questioned the value of these procedures as a method of implicating the structures associated with presenting symptoms and concluded that the capability of these tests to assess and implicate specific pathology as the source of symptoms cannot be achieved with the certainty and confidence required to meaningfully inform clinical decision making. <ref name="Biederwolf" /><ref name=":0" /> | |||
<blockquote>"It is not possible to make a definitive diagnosis with the clinical tests currently in use" <ref name=":1" /></blockquote> | |||
According to Magee <ref name="Magee" /> many of these special tests, in particular those involving the labrum, have not shown high sensitivity or specificity; and as a result combination of tests or test clusters, often referred to as clinical prediction rules are considered more useful, although even in these cases, the tests are not necessarily definitive.<ref name="Magee" /> While there has been a large amount of research on Orthopaedic Special Tests for the shoulder, according to Hegedus et al <ref name="Hegedus2015" /> much of it is of low to moderate quality <ref name="Hegedus2008" /><ref name="Hegedus2012" /> and where they are high quality they display limited solid diagnostic metrics, sensitivity or specificity or application to clinical practice and as such is likely to vary greatly in the hands of different clinicians and in varying clinical practice environments. | |||
<blockquote>"Currently, almost without exception, there is a lack of clarity with regard to whether common tests used in clinical examination are useful in differentially diagnosing pathologies of the shoulder" <ref name="Hegedus2008" /></blockquote> | |||
<blockquote>"The use of any single shoulder physical examination test to make a pathoanatomic diagnosis cannot be unequivocally recommeded" <ref name="Hegedus2012" /></blockquote> | |||
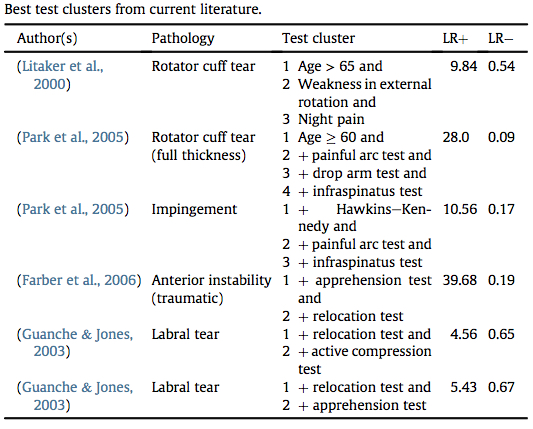
Similarly, while clustering Orthopaedic Special Tests together has been shown to improve diagnostic accuracy in both research and clinical practice, in many cases these clusters are being used incorrectly.<ref name="Hegedus2008" /><ref name="Hegedus2012" /><ref name="Hegedus2015" />Hegedus et al <ref name="Hegedus2015" /> identified just 6 best clusters, with best defined as those combinations of tests with the strongest likelihood ratios from research with the highest quality, judged through use of the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) document with a score of > 10. They suggest that any studies whose QUADAS is 10 or less have many design faults which make the likelihood ratios questionable and probably only applicable to those specific populations examined in the study, and not repeatable in outside of that group.<ref name="Hegedus2015" /> The following table summarises the current best clusters based on current evidence. | |||
[[File:OST Shoulder Clusters.jpg|thumb|900x900px|<ref name="Hegedus2015" />|none]] | |||
So what we do now know about Orthopaedic Special Tests of the Shoulder is that these tests generally cannot be utilised to make a definitive structural or pathoanatomic diagnosis, they may help us with symptom reproduction which can be used to test and retest following therapeutic interventions to assess for any change in symptoms. You can find the range of Individual Orthopaedic Special Tests for the Shoulder below. | |||
* [[Painful Arc]] | |||
* [[Hawkins / Kennedy Impingement Test of the Shoulder]] | |||
* [[Neers Test|Neer's Test]] | |||
* [[Codman's Test]] | |||
* [[Speeds Test|Speed's Test]] | |||
* [[Yergasons Test]] | |||
* [[O'Briens Test]] | |||
* | |||
== Sub Heading 2 == | == Sub Heading 2 == | ||
| Line 25: | Line 50: | ||
Traditionally Orthopaedic Special tests were used to assist in the diagnostic process by implicating specific tissue structures that are either dysfunctional, pathological, or lack structural integrity, confirming the findings from the physical assessment and providing a tentative diagnosis.<ref name="Magee">Magee, D. Shoulder. Chapter 5 In: Orthopedic Physical Assessment. Elsevier, 2014</ref> Special testing is generally performed following a full examination of the shoulder that includes but is not limited to patient history, mechanism of injury, clinical observation, bony and soft tissue palpation, assessment of active and passive physiological movements, assessment of passive arthokinematic / accessory joint mobility, neurological assessment, manual muscle testing, and functional assessments.<ref name="Biederwolf">Biederwolf NE. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3812837/ A proposed evidence-based shoulder special testing examination algorithm: clinical utility based on a systematic review of the literature.] International Journal of Sports Physical Therapy. 2013 Aug;8(4):427.</ref> Reproduction of pain, and weakness during these special test were considered clinically diagnostic. | Traditionally Orthopaedic Special tests were used to assist in the diagnostic process by implicating specific tissue structures that are either dysfunctional, pathological, or lack structural integrity, confirming the findings from the physical assessment and providing a tentative diagnosis.<ref name="Magee">Magee, D. Shoulder. Chapter 5 In: Orthopedic Physical Assessment. Elsevier, 2014</ref> Special testing is generally performed following a full examination of the shoulder that includes but is not limited to patient history, mechanism of injury, clinical observation, bony and soft tissue palpation, assessment of active and passive physiological movements, assessment of passive arthokinematic / accessory joint mobility, neurological assessment, manual muscle testing, and functional assessments.<ref name="Biederwolf">Biederwolf NE. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3812837/ A proposed evidence-based shoulder special testing examination algorithm: clinical utility based on a systematic review of the literature.] International Journal of Sports Physical Therapy. 2013 Aug;8(4):427.</ref> Reproduction of pain, and weakness during these special test were considered clinically diagnostic. | ||
However, although Orthopaedic Special Tests are commonly used, findings from both narrative, systematic reviews and research investigations have consistently questioned the value of these procedures as a method of implicating the structures associated with presenting symptoms and concluded that the capability of these tests to assess and implicate specific pathology as the source of symptoms cannot be achieved with the certainty and confidence required to meaningfully inform clinical decision making. <ref name="Biederwolf" /><ref>Lewis J, McCreesh K, Roy JS, Ginn K. Rotator cuff tendinopathy: navigating the diagnosis-management conundrum. journal of orthopaedic & sports physical therapy. 2015 Nov;45(11):923-37.</ref> | However, although Orthopaedic Special Tests are commonly used, findings from both narrative, systematic reviews and research investigations have consistently questioned the value of these procedures as a method of implicating the structures associated with presenting symptoms and concluded that the capability of these tests to assess and implicate specific pathology as the source of symptoms cannot be achieved with the certainty and confidence required to meaningfully inform clinical decision making. <ref name="Biederwolf" /><ref name=":0">Lewis J, McCreesh K, Roy JS, Ginn K. Rotator cuff tendinopathy: navigating the diagnosis-management conundrum. journal of orthopaedic & sports physical therapy. 2015 Nov;45(11):923-37.</ref> | ||
<blockquote>"It is not possible to make a definitive diagnosis with the clinical tests currently in use" <ref>Lewis JS, Tennent TD. How Effective are our Diagnostic Tests for Rotator Cuff Pathology. Evidence Based Sports Medicine. 2nd Edition. BMJ Books. Blackwell Publishing. 2007.</ref></blockquote> | <blockquote>"It is not possible to make a definitive diagnosis with the clinical tests currently in use" <ref name=":1">Lewis JS, Tennent TD. How Effective are our Diagnostic Tests for Rotator Cuff Pathology. Evidence Based Sports Medicine. 2nd Edition. BMJ Books. Blackwell Publishing. 2007.</ref></blockquote> | ||
According to Magee <ref name="Magee" /> many of these special tests, in particular those involving the labrum, have not shown high sensitivity or specificity; and as a result combination of tests or test clusters, often referred to as clinical prediction rules are considered more useful, although even in these cases, the tests are not necessarily definitive.<ref name="Magee" /> While there has been a large amount of research on Orthopaedic Special Tests for the shoulder, according to Hegedus et al <ref name="Hegedus2015">Hegedus EJ, Cook C, Lewis J, Wright A, Park JY. Combining orthopedic special tests to improve diagnosis of shoulder pathology. Physical Therapy in Sport. 2015 May 31;16(2):87-92.</ref> much of it is of low to moderate quality <ref name="Hegedus2008">Hegedus, E. J., Goode, A., Campbell, S., Morin, A., Tamaddoni, M., Moorman, C. T., 3rd, et al. (2008). Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. British Journal of Sports Medicine, 42, 80e92. discussion 92.</ref><ref name="Hegedus2012">Hegedus, E. J., Goode, A. P., Cook, C. E., Michener, L., Myer, C. A., Myer, D. M., et al. (2012). Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta- analysis of individual tests. British Journal of Sports Medicine, 46, 964e978.</ref> and where they are high quality they display limited solid diagnostic metrics, sensitivity or specificity or application to clinical practice and as such is likely to vary greatly in the hands of different clinicians and in varying clinical practice environments. | According to Magee <ref name="Magee" /> many of these special tests, in particular those involving the labrum, have not shown high sensitivity or specificity; and as a result combination of tests or test clusters, often referred to as clinical prediction rules are considered more useful, although even in these cases, the tests are not necessarily definitive.<ref name="Magee" /> While there has been a large amount of research on Orthopaedic Special Tests for the shoulder, according to Hegedus et al <ref name="Hegedus2015">Hegedus EJ, Cook C, Lewis J, Wright A, Park JY. Combining orthopedic special tests to improve diagnosis of shoulder pathology. Physical Therapy in Sport. 2015 May 31;16(2):87-92.</ref> much of it is of low to moderate quality <ref name="Hegedus2008">Hegedus, E. J., Goode, A., Campbell, S., Morin, A., Tamaddoni, M., Moorman, C. T., 3rd, et al. (2008). Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. British Journal of Sports Medicine, 42, 80e92. discussion 92.</ref><ref name="Hegedus2012">Hegedus, E. J., Goode, A. P., Cook, C. E., Michener, L., Myer, C. A., Myer, D. M., et al. (2012). Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta- analysis of individual tests. British Journal of Sports Medicine, 46, 964e978.</ref> and where they are high quality they display limited solid diagnostic metrics, sensitivity or specificity or application to clinical practice and as such is likely to vary greatly in the hands of different clinicians and in varying clinical practice environments. | ||
Revision as of 11:40, 2 April 2021
Original Editor - Naomi O'Reilly
Top Contributors - Kim Jackson, Manisha Shrestha, Shoko Otsuka, Naomi O'Reilly, Rucha Gadgil, Tarina van der Stockt and Lucinda hampton
Introduction[edit | edit source]
Traditionally Orthopaedic Special tests were used to assist in the diagnostic process by implicating specific tissue structures that are either dysfunctional, pathological, or lack structural integrity, confirming the findings from the physical assessment and providing a tentative diagnosis.[1] Special testing is generally performed following a full examination of the shoulder that includes but is not limited to patient history, mechanism of injury, clinical observation, bony and soft tissue palpation, assessment of active and passive physiological movements, assessment of passive arthokinematic / accessory joint mobility, neurological assessment, manual muscle testing, and functional assessments.[2] Reproduction of pain, and weakness during these special test were considered clinically diagnostic.
However, although Orthopaedic Special Tests are commonly used, findings from both narrative, systematic reviews, and research investigations have consistently questioned the value of these procedures as a method of implicating the structures associated with presenting symptoms and concluded that the capability of these tests to assess and implicate specific pathology as the source of symptoms cannot be achieved with the certainty and confidence required to meaningfully inform clinical decision making. [2][3]
"It is not possible to make a definitive diagnosis with the clinical tests currently in use" [4]
According to Magee [1] many of these special tests, in particular those involving the labrum, have not shown high sensitivity or specificity; and as a result combination of tests or test clusters, often referred to as clinical prediction rules are considered more useful, although even in these cases, the tests are not necessarily definitive.[1] While there has been a large amount of research on Orthopaedic Special Tests for the shoulder, according to Hegedus et al [5] much of it is of low to moderate quality [6][7] and where they are high quality they display limited solid diagnostic metrics, sensitivity or specificity or application to clinical practice and as such is likely to vary greatly in the hands of different clinicians and in varying clinical practice environments.
"Currently, almost without exception, there is a lack of clarity with regard to whether common tests used in clinical examination are useful in differentially diagnosing pathologies of the shoulder" [6]
"The use of any single shoulder physical examination test to make a pathoanatomic diagnosis cannot be unequivocally recommeded" [7]
Similarly, while clustering Orthopaedic Special Tests together has been shown to improve diagnostic accuracy in both research and clinical practice, in many cases these clusters are being used incorrectly.[6][7][5]Hegedus et al [5] identified just 6 best clusters, with best defined as those combinations of tests with the strongest likelihood ratios from research with the highest quality, judged through use of the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) document with a score of > 10. They suggest that any studies whose QUADAS is 10 or less have many design faults which make the likelihood ratios questionable and probably only applicable to those specific populations examined in the study, and not repeatable in outside of that group.[5] The following table summarises the current best clusters based on current evidence.
So what we do now know about Orthopaedic Special Tests of the Shoulder is that these tests generally cannot be utilised to make a definitive structural or pathoanatomic diagnosis, they may help us with symptom reproduction which can be used to test and retest following therapeutic interventions to assess for any change in symptoms. You can find the range of Individual Orthopaedic Special Tests for the Shoulder below.
- Painful Arc
- Hawkins / Kennedy Impingement Test of the Shoulder
- Neer's Test
- Codman's Test
- Speed's Test
- Yergasons Test
- O'Briens Test
Sub Heading 2[edit | edit source]
Sub Heading 3[edit | edit source]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedMagee - ↑ 2.0 2.1 Cite error: Invalid
<ref>tag; no text was provided for refs namedBiederwolf - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs named:0 - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs named:1 - ↑ 5.0 5.1 5.2 5.3 5.4 Cite error: Invalid
<ref>tag; no text was provided for refs namedHegedus2015 - ↑ 6.0 6.1 6.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedHegedus2008 - ↑ 7.0 7.1 7.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedHegedus2012
Introduction[edit | edit source]
Traditionally Orthopaedic Special tests were used to assist in the diagnostic process by implicating specific tissue structures that are either dysfunctional, pathological, or lack structural integrity, confirming the findings from the physical assessment and providing a tentative diagnosis.[1] Special testing is generally performed following a full examination of the shoulder that includes but is not limited to patient history, mechanism of injury, clinical observation, bony and soft tissue palpation, assessment of active and passive physiological movements, assessment of passive arthokinematic / accessory joint mobility, neurological assessment, manual muscle testing, and functional assessments.[2] Reproduction of pain, and weakness during these special test were considered clinically diagnostic.
However, although Orthopaedic Special Tests are commonly used, findings from both narrative, systematic reviews and research investigations have consistently questioned the value of these procedures as a method of implicating the structures associated with presenting symptoms and concluded that the capability of these tests to assess and implicate specific pathology as the source of symptoms cannot be achieved with the certainty and confidence required to meaningfully inform clinical decision making. [2][3]
"It is not possible to make a definitive diagnosis with the clinical tests currently in use" [4]
According to Magee [1] many of these special tests, in particular those involving the labrum, have not shown high sensitivity or specificity; and as a result combination of tests or test clusters, often referred to as clinical prediction rules are considered more useful, although even in these cases, the tests are not necessarily definitive.[1] While there has been a large amount of research on Orthopaedic Special Tests for the shoulder, according to Hegedus et al [5] much of it is of low to moderate quality [6][7] and where they are high quality they display limited solid diagnostic metrics, sensitivity or specificity or application to clinical practice and as such is likely to vary greatly in the hands of different clinicians and in varying clinical practice environments.
"Currently, almost without exception, there is a lack of clarity with regard to whether common tests used in clinical examination are useful in differentially diagnosing pathologies of the shoulder" [6]
"The use of any single shoulder physical examination test to make a pathoanatomic diagnosis cannot be unequivocally recommeded" [7]
Similarly, while clustering Orthopaedic Special Tests together has been shown to improve diagnostic accuracy in both research and clinical practice, in many cases these clusters are being used incorrectly.[6][7][5]Hegedus et al [5] identified just 6 best clusters, with best defined as those combinations of tests with the strongest likelihood ratios from research with the highest quality, judged through use of the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) document with a score of > 10. They suggest that any studies whose QUADAS is 10 or less have many design faults which make the likelihood ratios questionable and probably only applicable to those specific populations examined in the study, and not repeatable in outside of that group.[5] The following table summarises the current best clusters based on current evidence.
So what we do now know about Orthopaedic Special Tests of the Shoulder is that these tests generally cannot be utilised to make a definitive structural or pathoanatomic diagnosis, they may help us with symptom reproduction which can be used to test and retest following therapeutic interventions to assess for any change in symptoms. You can find the range of Individual Orthopaedic Special Tests for the Shoulder below.
- Painful Arc
- Hawkins / Kennedy Impingement Test of the Shoulder
- Neer's Test
- Codman's Test
- Speed's Test
- Yergasons Test
- O'Briens Test
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Magee, D. Shoulder. Chapter 5 In: Orthopedic Physical Assessment. Elsevier, 2014
- ↑ 2.0 2.1 Biederwolf NE. A proposed evidence-based shoulder special testing examination algorithm: clinical utility based on a systematic review of the literature. International Journal of Sports Physical Therapy. 2013 Aug;8(4):427.
- ↑ Lewis J, McCreesh K, Roy JS, Ginn K. Rotator cuff tendinopathy: navigating the diagnosis-management conundrum. journal of orthopaedic & sports physical therapy. 2015 Nov;45(11):923-37.
- ↑ Lewis JS, Tennent TD. How Effective are our Diagnostic Tests for Rotator Cuff Pathology. Evidence Based Sports Medicine. 2nd Edition. BMJ Books. Blackwell Publishing. 2007.
- ↑ 5.0 5.1 5.2 5.3 5.4 Hegedus EJ, Cook C, Lewis J, Wright A, Park JY. Combining orthopedic special tests to improve diagnosis of shoulder pathology. Physical Therapy in Sport. 2015 May 31;16(2):87-92.
- ↑ 6.0 6.1 6.2 Hegedus, E. J., Goode, A., Campbell, S., Morin, A., Tamaddoni, M., Moorman, C. T., 3rd, et al. (2008). Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. British Journal of Sports Medicine, 42, 80e92. discussion 92.
- ↑ 7.0 7.1 7.2 Hegedus, E. J., Goode, A. P., Cook, C. E., Michener, L., Myer, C. A., Myer, D. M., et al. (2012). Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta- analysis of individual tests. British Journal of Sports Medicine, 46, 964e978.