Somatosensation: Difference between revisions
Amanda Ager (talk | contribs) No edit summary |
Amanda Ager (talk | contribs) No edit summary |
||
| Line 24: | Line 24: | ||
== Receptors == | == Receptors == | ||
Somatosensory receptors are distributed throughout the entire body, rather than being concentrated at specialized locations. Different parts of the body will also have different concentrations of each type of receptor. The various types of receptors are able to sense various kinds of stimuli such as pressure against the skin, limb position, distention of the bladder, and body temperature. If a stimulus becomes so strong that it may be harmful, the somatosensory system is also responsible for feeling pain (nociception)<ref name=":1" />. | |||
Sensory receptors are classified into five categories: | Sensory receptors are classified into five categories: | ||
| Line 36: | Line 38: | ||
5. '''Chemoreceptors:''' Detects changes and is responsive to chemical stimuli. | 5. '''Chemoreceptors:''' Detects changes and is responsive to chemical stimuli. | ||
A single stimulus usually activates many receptors, and each receptor is capable of encoding stimulus features such as intensity, duration and direction. It is the central nervous system (CNS) which interprets the activity of the different receptors involved in the sensation and uses these interpretations to generate coherent perceptions<ref>Martín-Alguacil N., de Gaspar I., Schober J.M., Pfaff D.W. (2013) Somatosensation: End Organs for Tactile Sensation. In: Pfaff D.W. (eds) Neuroscience in the 21st Century. Springer, New York, NY. <nowiki>https://doi.org/10.1007/978-1-4614-1997-6_27</nowiki>.</ref>. | A single stimulus usually activates many receptors, and each receptor is capable of encoding stimulus features such as intensity, duration and direction. It is the central nervous system (CNS) which interprets the activity of the different receptors involved in the sensation and uses these interpretations to generate coherent perceptions<ref name=":1">Martín-Alguacil N., de Gaspar I., Schober J.M., Pfaff D.W. (2013) Somatosensation: End Organs for Tactile Sensation. In: Pfaff D.W. (eds) Neuroscience in the 21st Century. Springer, New York, NY. <nowiki>https://doi.org/10.1007/978-1-4614-1997-6_27</nowiki>.</ref>. | ||
== Methods for Measuring Somatosensation == | |||
As a clinician, it is important to note that there is no direct way of measuring somatosensation. Even though some of the tests mentioned below target a specific aspect of somatosensation, it is not practical to measure one sense in isolation. Often times various types of receptors are active to varying degrees with different stimuli. The follow are the most common categorizations for quantifying aspects of somatosensation. | |||
Proprioception mainly comprises of kinesthesia and joint position sense. It can also include the sense of muscle tension, joint pressure, sense of force and sense of velocity. | |||
Kinesthesia: Sense of movement. | |||
Brief Kinesthesia Test | |||
Joint position sense: Sense of joint or limb positioning, it can be active or passive. | |||
Joint repositioning test (active or passive) | |||
Tactile discrimination: Tactile discrimination (such as two-point discrimination) can affect stereognosis, the ability to identify objects based on touch alone. Discriminative touch is also subdivided into touch, pressure, flutter and vibration. | |||
Discriminator | |||
Tactile Discrimination Test | |||
Sense of temperature | |||
Self-reported pain | |||
== Clinical Implications == | |||
== Resources == | == Resources == | ||
Revision as of 14:51, 31 August 2020
Original Editor - User Name
Top Contributors - Amanda Ager, Kim Jackson, Manisha Shrestha, Lucinda hampton, Tolulope Adeniji, Aminat Abolade and Carina Therese Magtibay
Introduction[edit | edit source]
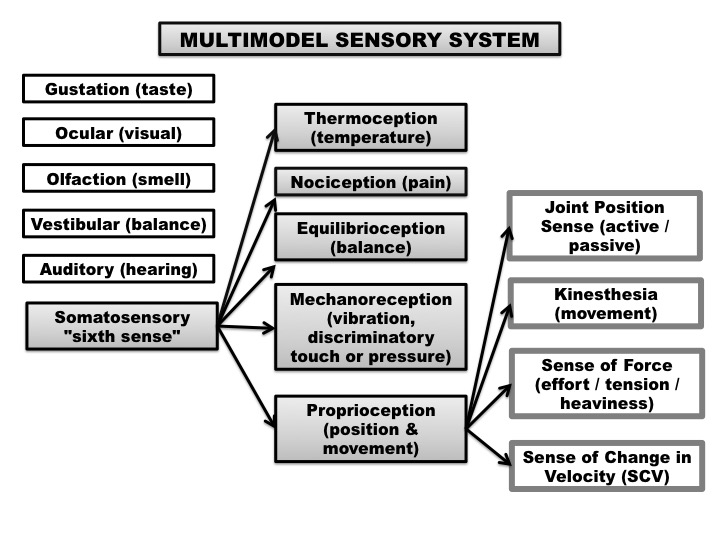
The body functions and interacts with its surrounding environment through the simultaneous inputs of our five senses; gustation (taste), ocular (vision), olfaction (smell), vestibular (balance) and auditory (hearing), respectively. However, it is often forgotten that we also have a "sixth sense", understood to be our sense of somatosensation. Somatosensation is an overarching sense which includes the sub-modalities of:
- Thermoception (temperature);
- Nociception (pain);
- Equilibrioception (balance);
- Mechanoreception (vibration, discriminatory touch and pressure);
- Proprioception (positioning and movement).
Collectively, these senses allow us to participate in our activities of daily living (ADLs) by guiding our movements, all the while minimizing the possibility of sustaining an injury.
What is Somatosensation?[edit | edit source]
Somatosensation is a mixed sensory category, and is mediated, in part, by the somatosensory and posterior parietal cortices. They underlie the ability to identify tactile characteristics of our surroundings, create meaning about sensations, and formulate body actions related to the sensations[1]. These various sensations contribute to the somatic aspects of the body scheme as a basis for interacting with our environments[2].
Body representations are reliant on multi-sensory cortical and sub‐cortical areas, including particularly premotor cortex, posterior parietal cortex and the putamen[3].
It is also important to note that the experience of sensing often involves a more complex integration of somatosensory inputs, and may be influenced by emotional and social contexts as well[2].
Word origin: somato– from soma (body) + sensation.
Receptors[edit | edit source]
Somatosensory receptors are distributed throughout the entire body, rather than being concentrated at specialized locations. Different parts of the body will also have different concentrations of each type of receptor. The various types of receptors are able to sense various kinds of stimuli such as pressure against the skin, limb position, distention of the bladder, and body temperature. If a stimulus becomes so strong that it may be harmful, the somatosensory system is also responsible for feeling pain (nociception)[4].
Sensory receptors are classified into five categories:
1. Mechanoreceptors: Detects mechanical changes or deformations in tissues.
2. Thermoreceptors: Detects changes in temperature.
3. Proprioceptors: Detects changes to limb position (joint position sense), movement detection (kinesthesia).
4. Pain receptors (nociceptors): Neural processing of injurious stimuli in response to tissue damage.
5. Chemoreceptors: Detects changes and is responsive to chemical stimuli.
A single stimulus usually activates many receptors, and each receptor is capable of encoding stimulus features such as intensity, duration and direction. It is the central nervous system (CNS) which interprets the activity of the different receptors involved in the sensation and uses these interpretations to generate coherent perceptions[4].
Methods for Measuring Somatosensation[edit | edit source]
As a clinician, it is important to note that there is no direct way of measuring somatosensation. Even though some of the tests mentioned below target a specific aspect of somatosensation, it is not practical to measure one sense in isolation. Often times various types of receptors are active to varying degrees with different stimuli. The follow are the most common categorizations for quantifying aspects of somatosensation.
Proprioception mainly comprises of kinesthesia and joint position sense. It can also include the sense of muscle tension, joint pressure, sense of force and sense of velocity.
Kinesthesia: Sense of movement.
Brief Kinesthesia Test
Joint position sense: Sense of joint or limb positioning, it can be active or passive.
Joint repositioning test (active or passive)
Tactile discrimination: Tactile discrimination (such as two-point discrimination) can affect stereognosis, the ability to identify objects based on touch alone. Discriminative touch is also subdivided into touch, pressure, flutter and vibration.
Discriminator
Tactile Discrimination Test
Sense of temperature
Self-reported pain
Clinical Implications[edit | edit source]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ Romo R, Hernández A, Salinas E, et al. From sensation to action. Behav Brain Res 2002;135:105–118.
- ↑ 2.0 2.1 Dunn W. Implementing neuroscience principles to support habilitation and recovery. In: Christiansen C, Baum CM, editors. Occupational Therapy: Enabling Function and Well-being. Thorofare, NJ: SLACK; 1997:182–223.
- ↑ Holmes NP, Spence C. The body schema and multisensory representation(s) of peripersonal space. Cogn Process 2004; 5: 94–105.
- ↑ 4.0 4.1 Martín-Alguacil N., de Gaspar I., Schober J.M., Pfaff D.W. (2013) Somatosensation: End Organs for Tactile Sensation. In: Pfaff D.W. (eds) Neuroscience in the 21st Century. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-1997-6_27.