Spondylolisthesis: Difference between revisions
m (Text replace - ''''Lead Editors'''' to ''''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}') |
No edit summary |
||
| Line 2: | Line 2: | ||
'''Original Editors ''' - [[User:Margo De Mesmaeker|Margo De Mesmaeker]] | '''Original Editors ''' - [[User:Margo De Mesmaeker|Margo De Mesmaeker]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition / Description == | == Definition / Description == | ||
| Line 8: | Line 8: | ||
Spondylolisthesis is a deviation of the spine when a shift of the vertebra occurs compared to the one just below. It is frequently situated at the fourth and fifth lumbar vertebra<ref name="N.J. Rosenberg">N.J. Rosenberg. Degenerative spondylolisthesis. Predisposing factors. The journal of Bone and Joint Surgery (1975) 57:467-474. (1C)</ref>. This shift is forward orientated, sometimes backwards, but this is rather uncommon. <br>A forward shift is called an anterolysthesis and a backward shift is called retrolysthesis. The degree of spondylolisthesis is generally mild, with a mean of 14%. Because of the shift it is possible that a nerve can be compressed or that the spinal canal is narrowed. <br> | Spondylolisthesis is a deviation of the spine when a shift of the vertebra occurs compared to the one just below. It is frequently situated at the fourth and fifth lumbar vertebra<ref name="N.J. Rosenberg">N.J. Rosenberg. Degenerative spondylolisthesis. Predisposing factors. The journal of Bone and Joint Surgery (1975) 57:467-474. (1C)</ref>. This shift is forward orientated, sometimes backwards, but this is rather uncommon. <br>A forward shift is called an anterolysthesis and a backward shift is called retrolysthesis. The degree of spondylolisthesis is generally mild, with a mean of 14%. Because of the shift it is possible that a nerve can be compressed or that the spinal canal is narrowed. <br> | ||
Type I = Dysplastic or congenital spondylolisthesis<ref>Newman et al, Classification of Spondylolisis and Spondylolisthesis, Clinical Orthopaedics &amp;amp;amp;amp;amp; Related Research, 1976</ref><br>While this type is rare, symptoms will not occur in childhood but wil start in adolescence. The cause mostly is a congenital defect of the lumbosacrale facet joints or the processus articularis. In some cases it can be caused by pars interarticularis that is too long.<br> | Type I = Dysplastic or congenital spondylolisthesis<ref>Newman et al, Classification of Spondylolisis and Spondylolisthesis, Clinical Orthopaedics &amp;amp;amp;amp;amp;amp;amp; Related Research, 1976</ref><br>While this type is rare, symptoms will not occur in childhood but wil start in adolescence. The cause mostly is a congenital defect of the lumbosacrale facet joints or the processus articularis. In some cases it can be caused by pars interarticularis that is too long.<br> | ||
Type II = Isthmic or spondylolylitic spondylolisthesis<br>This type is most common and can be divided into 3 subcategories: | Type II = Isthmic or spondylolylitic spondylolisthesis<br>This type is most common and can be divided into 3 subcategories: | ||
| Line 26: | Line 26: | ||
Type IV = Traumatic spondylolisthesis<br>This type is rather rare and involves an acute fracture of the posterior elements of the vertebra, excluding the pars interarticularis<br> | Type IV = Traumatic spondylolisthesis<br>This type is rather rare and involves an acute fracture of the posterior elements of the vertebra, excluding the pars interarticularis<br> | ||
Type V = Pathological spondylolisthesis | Type V = Pathological spondylolisthesis occurs because of a structural weakness of the bone secondary to a disease process such as a tumor or other bone diseases. | ||
[[Image:Spondylolisthesis.jpg]] | [[Image:Spondylolisthesis.jpg]] | ||
| Line 48: | Line 38: | ||
add text here relating to the mechanism of injury and/or pathology of the condition<br> | add text here relating to the mechanism of injury and/or pathology of the condition<br> | ||
== Clinical Presentation == | == Clinical Presentation<br> == | ||
Symptoms that can occur with spondylolisthesis are low back pain, pain in the legs or a combination of both. Patients complain of deep, dull pain typically situated in the lumbosacral region after exercise, especially with an extension of the lumbar spine. The range of motion is diminished and the hamstrings are tense. When there is a compression of a nerve, patients mostly develop numbness, pain or tingling. If the compression is very severe it may be possible that the patient develops the cauda equine syndrome. | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 98: | Line 88: | ||
== Resources <br> == | == Resources <br> == | ||
[http://orthoinfo.aaos.org/topic.cfm?topic=A00588 Information from the AAOS] | |||
== Case Studies == | == Case Studies == | ||
| Line 110: | Line 100: | ||
<references /> | <references /> | ||
[[Category:Vrije_Universiteit_Brussel_Project]][[Category:Musculoskeletal/Orthopaedics|Orthopaedics]][[Category:Lumbar]] | [[Category:Vrije_Universiteit_Brussel_Project]] [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] [[Category:Lumbar]] | ||
Revision as of 21:33, 19 October 2013
Original Editors - Margo De Mesmaeker
Top Contributors - Maëlle Cormond, Simisola Ajeyalemi, Evi Peeters, Margo De Mesmaeker, Kim Jackson, Admin, Chrysolite Jyothi Kommu, Shaimaa Eldib, Kenneth de Becker, Lucinda hampton, Rachael Lowe, Mike Myracle, Evan Thomas, Carlos De Coster, Johnathan Fahrner, Aminat Abolade, Mariam Hashem, Shreya Pavaskar, Camille Linussio, Claire Knott, Rucha Gadgil, Laura Ritchie, Jess Bell, Kirenga Bamurange Liliane and Scott Buxton
Definition / Description[edit | edit source]
Spondylolisthesis is a deviation of the spine when a shift of the vertebra occurs compared to the one just below. It is frequently situated at the fourth and fifth lumbar vertebra[1]. This shift is forward orientated, sometimes backwards, but this is rather uncommon.
A forward shift is called an anterolysthesis and a backward shift is called retrolysthesis. The degree of spondylolisthesis is generally mild, with a mean of 14%. Because of the shift it is possible that a nerve can be compressed or that the spinal canal is narrowed.
Type I = Dysplastic or congenital spondylolisthesis[2]
While this type is rare, symptoms will not occur in childhood but wil start in adolescence. The cause mostly is a congenital defect of the lumbosacrale facet joints or the processus articularis. In some cases it can be caused by pars interarticularis that is too long.
Type II = Isthmic or spondylolylitic spondylolisthesis
This type is most common and can be divided into 3 subcategories:
Type II A: Stressfracture of the pars interarticularis
Type II B: Elongation of the pars interarticularis by microtrauma
Type II C: Acute fracture of the pars interarticularis
Type III = Degenerative spondylolisthesis
Type IV = Traumatic spondylolisthesis
This type is rather rare and involves an acute fracture of the posterior elements of the vertebra, excluding the pars interarticularis
Type V = Pathological spondylolisthesis occurs because of a structural weakness of the bone secondary to a disease process such as a tumor or other bone diseases.
Clinically Relevant Anatomy
[edit | edit source]
add text here relating to clinically relevant anatomy of the condition
Mechanism of Injury / Pathological Process
[edit | edit source]
add text here relating to the mechanism of injury and/or pathology of the condition
Clinical Presentation
[edit | edit source]
Symptoms that can occur with spondylolisthesis are low back pain, pain in the legs or a combination of both. Patients complain of deep, dull pain typically situated in the lumbosacral region after exercise, especially with an extension of the lumbar spine. The range of motion is diminished and the hamstrings are tense. When there is a compression of a nerve, patients mostly develop numbness, pain or tingling. If the compression is very severe it may be possible that the patient develops the cauda equine syndrome.
Diagnostic Procedures[edit | edit source]
Spondylolisthesis is featured by the following characteristics. It is mostly clear that the patient has complaints of pain in the lower back and leg. In the history the majority of the people have had a fall or trauma. During the inspection and physical examination of the patient there are typically no visible signs of spondylolisthesis but there may be a tightness of the hamstrings. The abdominal muscles are weakened and there can be an increase of the lumbar lordosis[3]. The patient has trouble with flexion and extension of the spine because it hurts.
When the physiotherapist is not sure, an axial loaded MRI can always identify the disorder[4].
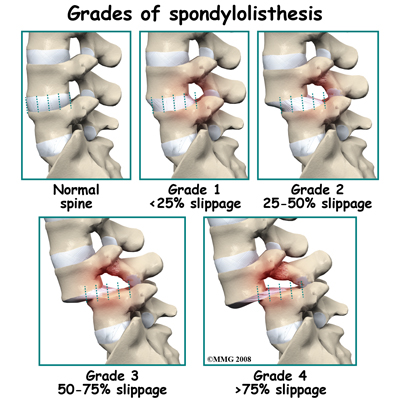
The severity of spondylolisthesis is expressed according to the Meyerding grading system. The system categorizes severity based upon measurements on lateral X-ray of the distance from the posterior edge of the superior vertebral body to the posterior edge of the adjacent inferior vertebral body. This distance is then reported as a percentage of the total superior vertebral body length.[5]
According the degree of shift, there are five grades:
- Grade 1: <25%
- Grade 2: 25% - 50%
- Grade 3: 51% - 75%
- Grade 4: >75%
(Over 100% is Spondyloptosis, when the vertebra completely falls off the supporting vertebra.)
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
General
• Initially resting and avoiding movements like lifting, bending and sports.
• Anti-inflammatory medicine to improve the infection and diminish the pain[6] .
• A corticosteroid injection can be used if patients have pain in the leg or numbness
• Sometimes a hyperextension brace can be used. This is useful because during the hyperextension of the lumbar spine the verterbrae get closer together.
• When the condition is very severe a surgical intervention may be necessary to attach the vertebras together.
• A surgical intervention has better results than a nonsurgical care in case of neurological symptoms[7].
Physical therapy
The initial therapy for spondylolisthesis is a conservative treatment done by the physiotherapist. Physical therapy is used to improve the range of motion of the lumbar spine and the hamstrings. Also improving the strength of the abdominal muscles is a very important part of the therapy, so that the spine can be stabilized.
The physiotherapist needs to give the patient information about the posture, lifting techniques and the use of heat to diminish the symptoms.
A brace can be used to reduce the pain, but it does not reduce the shift of the vertebra[8]. So it is a good aid during the painful periods but it is not to be used when the patients complaints are reduced.
Strengthening the deep abdominal muscles is a very important part of the physical therapy. Isometric and isotonic exercises for the main muscle groups of the trunk provide a stabilization of the spine and a reduction of the pain[9]. Also the hamstrings need to be stretched, so that their mobility can be improved.
An excellent exercise is stationary bicycling because it promotes the spine flexion. Impact sports like running should not be done because it provokes wear. Other sports that can be practiced are walking and swimming. They have no value in improving the shift, but these sports are good alternatives for cardiovascular exercises[8].
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit | edit source]
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ N.J. Rosenberg. Degenerative spondylolisthesis. Predisposing factors. The journal of Bone and Joint Surgery (1975) 57:467-474. (1C)
- ↑ Newman et al, Classification of Spondylolisis and Spondylolisthesis, Clinical Orthopaedics &amp;amp;amp;amp;amp;amp; Related Research, 1976
- ↑ B. Kalpakcioglu, T. Altinbilek, K. Senel. Determination of spondylolisthesis in low back pain by clinical evaluation. Jounal of Back a Musculoskeletal Rehabilitation 22 (2009) 27-32. (2B)
- ↑ P. Jayakumar et al. Dynamic degenerative lumbar spondylolisthesis: diagnosis with axial loaded magnetic resonance imaging, Spine. (Phila Pa 1976) 2006 May 1;31 (10): E298-301. (2B)
- ↑ H.W., Meyerding, Spondylolisthesis., Surg Gynecol Obsted. 1932
- ↑ M.W van Tulder et al. Nonsteroidal anti-inflammatory drugs for low back pain: a systematic review within the framework of the Cochrane collaboration back review group. Spine 2000 25:2501–2513. (1A)
- ↑ J.N. Weinstein et al. Surgical versus non-surgical treatment for lumbar degenerative spondylolisthesis. N. Engl. J. Med 2007 May 31;356 (22): 2557-2270. (1B)
- ↑ 8.0 8.1 L. Kalichman et al. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J (2008) 17;327 – 335. (2B)
- ↑ M. Sinaki et al. Lumbar spondylolisthesis: retrospective comparison and three year follow-up of two conservative treatment programs. Arch Phys Med Rehabil 1989 70:594-598. (1B)