The Role of the Physiotherapist in Learning Disabilities
Welcome to Contemporary and Emerging Issues in Physiotherapy Practice. This page is being developed by participants of a project to populate the Spinal Cord Injury section of Physiopedia.
- Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!
- If you would like to get involved in this project and earn accreditation for your contributions, please get in touch!
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Catherine Speirs, Ting Hui Tan, Idris Al Balushi, Kerry Morris, Ioannis Dimitrios Valmas, Nicola carter, Rucha Gadgil, Kim Jackson, Kirenga Bamurange Liliane, Lauren Lopez, 127.0.0.1, Admin, Shaimaa Eldib, Chee Wee Tan, WikiSysop, Ines Musabyemariya and Michelle Lee
Introduction
[edit | edit source]
We are a group of 4th year BSc (Hons) Physiotherapy students at Queen Margaret University, Edinburgh. As part of our Contemporary and Emerging Issues in Physiotherapy Practice module, we have decided to complete an online learning resource. This resource is primarily aimed at senior physiotherapy students and newly qualified physiotherapists. This online wiki will explore the areas of communication and health literacy when working with patients who have learning disabilities. This resource will take approximately 10 hours to complete and will contribute to your CPD profile. Besides providing you with new information and researched evidence, there will be quizzes and opportunities for you to reflect.
In 2015, there were 27,218 adults with learning disabilities known to local authorities in Scotland[1]. Most people with learning disabilities have greater health needs than the general population. People with learning disabilities are more likely to experience mental illness and are more prone to chronic illnesses such as epilepsy, physical and sensory impairments. A systematic review carried out in the Netherlands discovered that people with learning disabilities are at an increased risk of fractures and musculoskeletal impairments[2]. 50-90% of people with learning disabilities also have communication difficulties[3].
Aims[edit | edit source]
The aims of this wiki are:
- To provide final year physiotherapy students and new graduates with an online learning resource which develops their knowledge of learning disabilities and the common associated conditions that may require physiotherapy interventions.
- To introduce final year physiotherapy students and newly qualified graduates to the skills and strategies which can be utilised within their practice to offer a more effective and comprehensive management of communication and health literacy to those with learning disabilities.
Learning Outcomes[edit | edit source]
By the end of this online activity you should be able to:
- Discuss the impact of learning disabilities on the person and their needs in relation to physiotherapy interventions.
- Critically appraise the evidence base and some of the key approaches surrounding communication and health literacy within learning disabilities.
- Summarise the characteristics of psychological impacts and the underlying neurophysiology of communication difficulties experienced by those with learning disabilities.
- Critically reflect upon the possible challenges faced by physiotherapists when communicating with people who have learning disabilities.
- Critically evaluate the role of the physiotherapist in the area of learning disabilities with reference to relevant literature.
- Formulate stronger patient-therapist relationship by applying these effective communication methods in the practice setting.
Learning styles[edit | edit source]
Different individuals have different learning styles, thus as part of our consideration for you to make the most of your learning through this wiki, various activities and resources will be included to cover the different learning types and styles.
Are you aware of the different learning styles and which best suits you?
If you are not aware of your ideal learning style but would be interested in finding out, you can fill in a short questionnaire here, which will take approximately 5 minutes. This will then reveal your ideal learning style and most suited learning methods, which would be useful to know, not only throughout this wiki, but also as part of your future learning.
The different learning styles are:
- Visual
- Aural/Auditory
- Read/write
- Kinesthetic
- Multimodality
Blooms Taxonomy[edit | edit source]
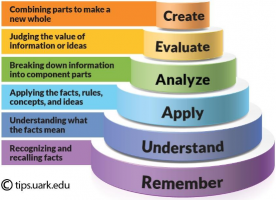
Blooms taxonomy uses a hierarchy to establish the different learning levels. Figure 1 demonstrates the pyramid structure and highlights that a foundation needs to be part of the learning process before this learning can be applied to everyday practices, and evaluations can be made.
Learning outcomes for this wiki have been based around Bloom's model, and the higher learning levels have been selected to be appropriate for final year students and newly qualified physiotherapists. This is to allow a deeper understanding of the topics covered and to be able to apply these to everyday situations.
Why is there a need for this Physiopedia page[edit | edit source]
- There is a gap in the literature.
- There is no current module in the BSc/MSc pre-reg courses on learning disabilities.
- Literacy and communication difficulties are experienced by many people with learning disabilities.
Activities Provided[edit | edit source]
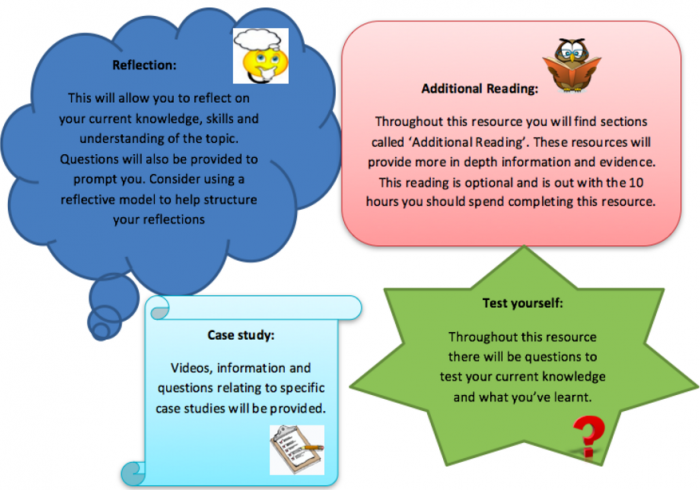
There will be different activities provided throughout this resource which are aimed at the different learning types.
How this resource relates to the Knowledge and Skills Framework (KSF)[edit | edit source]
The KSF is a competence framework that supports professional development and career progression for professionals working in the NHS. It ensures that staff are supported so that they can carry out their job effectively.This physiopedia page aims to address some of the core components of the KSF required of a Band 5 Physiotherapist. By completing this online resource it will help you to achieve some of the key indicators.
Here is a list of the key indicators that you will achieve in this wiki:
Communication:
- Improves the effectiveness of communication through communication skills.
- Constructively manages barriers to effective communication.
Personal and people development:
- Takes responsibility for own personal development and takes an active part in learning opportunities.
- Evaluates the effectiveness of learning opportunities and alerts others to benefits and problems.
Quality:
- Acts consistently with legislation, policies, procedures and other quality approaches and encourages others to do so.
- Uses and maintains resources efficiently and effectively and encourages others to do so.
Equality and diversity:
- Recognises people’s rights and acts in accordance with legislation, policies and procedures.
- Acts in ways that:
- Respect diversity.
- View people as individuals.
Assessment and treatment planning:
- Selects appropriate assessment approaches, methods, techniques and equipment, in line with
- Individual needs and characteristics.
- Evidence of effectiveness.
- The resources available.
- Monitors individuals during assessments and takes the appropriate action in relation to any significant changes or possible risks.
- Evaluates assessment findings/results and takes appropriate action when there are issues.
- identifies individuals whose needs fall outside protocols / pathways / models and makes referrals to the appropriate practitioners with the necessary degree of urgency.
For more information please navigate through the KSF website.
Understanding learning disabilities
[edit | edit source]
Definition and diagnostic criteria for learning disabilities[edit | edit source]
Learning disability VS learning difficulty[edit | edit source]
Prevalence and demographics of learnign disabilities [edit | edit source]
Different levels of learning disability[edit | edit source]
Factors resulting in learning disability[edit | edit source]
Common associated conditions[edit | edit source]
Impact of learning disability on the person and physiotherapist[edit | edit source]
Obstacles within health system[edit | edit source]
Role of the physiotherapist
[edit | edit source]
Introduction to the role[edit | edit source]
Mainstream or specialist physiotherapy services[edit | edit source]
Physiotherapy assessment[edit | edit source]
Physiotherapy management[edit | edit source]
24-hour postural care[edit | edit source]
Falls prevention[edit | edit source]
Physical Activity promotion[edit | edit source]
Education[edit | edit source]
Reflection[edit | edit source]
Communication
[edit | edit source]
Definition of communication[edit | edit source]
As mentioned earlier, 50 to 90% of the people with learning difficulties have communication difficulties (Chadwick & Jolliffe, 2009, Veselinova, 2012, and Jackson et al., 2014). According to Chadwick and Jolliffe in 2009, communication is defined as “a mutual interactive process involving adaptation by both the communicative partners”. It is not just a pure transaction of information, but also relationships can be formed and build up in the process (Higgs et al., 2009).
Language is a complex form of communication that involves written or spoken words to convey ideas and symbolise objects. Reading, writing, drawing, speaking, listening, adjusting one’s tone of voice, making eye contact are all involved on communication. Communication involves ‘expression’ and ‘comprehension’ with each aspect being related to a specific neural network.
Physiology of brain and how it affects communication[edit | edit source]
The language centres are located in the left hemisphere in approximately 95% of human beings. Broca’s area and Wernicke’s area are located in the left hemisphere of the brain.
Broca’s area is known as the motor-speech area and it is located adjacent to the precentral gyrus of the motor cortex in the frontal lobes. This area controls the movements required for articulation, facial expression and phonation.
Wernicke’s area includes the auditory comprehension centre. It lies in the posterior superior temporal lobe near the auditory cortex. It plays a role in understanding both spoken and written messages as well as being able to formulate coherent speech. Commands generated in Wernicke’s area are transferred via a fibre tract called the arcuate fasciculus to Broca’s area. Wernicke’s area receives input from both the visual cortex and the auditory cortex.
(TO INSERT BRAIN DIAGRAM HERE)
Types of communication difficulties[edit | edit source]
Aphasia
Damage to the language centres of the brain can result in aphasia. Aphasia can affect expression and comprehension of speech, reading and writing, gesture and the use of language. There are 3 types of aphasia - expressive, receptive and global.
- Expressive aphasia is when a person has difficulty translating their ideas into meaningful sounds which results in non-fluent speech. It is associated with damage in Broca’s area.
- Receptive aphasia is associated with damage in Wernicke’s area. People with receptive aphasia have difficulty in the comprehension of language.
- Global aphasia occurs where there is widespread brain damage including lesions in the left hemisphere. This results in impairment of both expressive and receptive language functions. There are also a range of other neurological signs such as hemianopia, hemiplegia, visual impairments, auditory impairments, attention and memory impairments and other cognitive impairments.
Dysarthria
Dysarthria refers to difficulty with executing speech. There are five sub-systems that are required in the coordination of speech. These include respiration, phonation, articulation, resonance and prosody. Weakness in any of these systems or incoordination of these systems can cause dysarthria.
Apraxia of Speech
This is an inability to programme speech movements. It is an impairment in the ability to coordinate the timing, force production and sequencing of movements for the production of speech.
Comprehension impairments
- A person may not understand some or all of the instructions that are given to them.
- A person’s non-verbal communication may suggest that they understand what you are saying but in fact they may not understand what you are saying. A person may mirror you, such that if you smile and nod they may do the same and they may also mirror your body language too.
Expressive impairments
Some people may have difficulty finding their words which will affect the way they answer your questions.
https://www.youtube.com/watch?v=IyV1v-nib38
https://www.youtube.com/watch?v=Hp4PW17U_h8
Impact of communication difficulties[edit | edit source]
Difficulty in communication can lower one’s self-esteem and result in low moods which will further impair communication (Jackson et al., 2014). This may result in “diagnostic overshadowing”, where people with learning disabilities are often misunderstood as having challenging behaviour when it is in fact their way of trying to communicate (Kingston & Bailey, 2009), and hence they are less likely to have chances to express their views (Lewer & Harding, 2013).
Barriers to communication[edit | edit source]
People with learning disability have limited vocabulary (Godsell & Scarborough, 2006, and Sperotto, 2016), problems expressing themselves (Godsell & Scarborough, 2006, and Chadwick & Jolliffe, 2009) and comprehending verbal and written information (Chadwick & Jolliffe, 2009). They may also feel apprehensive and stressed meeting strangers in new environments.
Types of barriers:
http://www.yourarticlelibrary.com/business-communication/4-different-types-of-barriers-to-effective-communication/1004/ http://managementstudyguide.com/communication_barriers.htm#
http://www.skillsyouneed.com/ips/barriers-communication.html
Language/Cultural/Perceptual Differences
- Different languages/tongues
- Unfamiliar accents
- Use of jargon
- Multiple meanings of a word - easy to misinterpret
Psychological/Emotional
- Difficulty expressing emotions
- Low self-esteem
- Personal taboo topics
- Poor mood - less receptive to communication
Physical disabilities
- Hearing problems
- Speech difficulties
- Visual problems
- Limited memory space - information overload, poor retention of information
Attitudinal
- Inattention
- Resistance to change
- Lack of motivation
- Unwilling to communicate
Distractions
- Louds noises
- Bright lightings
- Crowded area
Strategies/methods/tools for effective communication[edit | edit source]
When speaking to people with learning disabilities, easy and simplified language should be used at a slow comfortable pace to promote positive interactions, but it should not appear supercilious (Veselinova, 2012).
Common subtle indicators of pain you can watch out for include changes in behaviour, noise level, body language or facial expressions and holding the part of the body that hurts (Beacroft & Dodd, 2011).
In 2009, Kingston and Bailey recommended tools such as the “pain diary” (Figure 1), which is “a tick chart designed for the person with a learning disability to complete”, as well as the “pain story” (Figure 2), which is “a templated designed to help individuals talk about their pain” and “included aspects of a person’s history, their previous experiences of pain, and the current influences upon their behaviour”. These simple tools with pictures and symbols have been found to enhance communication and assessment, as they not only “help with identifying the location, type, severity and duration of pain” (Beacroft & Dodd, 2011), but also allowed people with learning disabilities the opportunity and freedom to talk and describe their pain, and it is highly reassuring for them when the health professionals like physiotherapists are able to understand and believe their words (Kingston & Bailey, 2009).
(TO INSERT PAIN DIARY DIAGRAM AND PAIN STORY DIAGRAM HERE)
For those with more complex communication difficulties, there are “augmentative and alternative communication strategies (AACs)” (Godsell & Scarborough, 2006) that physiotherapists can use, such as “Makaton, British sign language, braille and the use of assistive technology” (Veselinova, 2012). Makaton is a language programme that uses signs and symbols to help people communicate (Let’s Talk Makaton, 2016). The signs and symbols are used in spoken word order and help develop the communication skills of the person (Let’s Talk Makaton, 2016). Furthermore, according to the Royal College of Speech and Language Therapists in 2006, “manual signing continues to be used as an intervention strategy” for the people with learning disabilities (Chadwick & Jolliffe, 2009), thus if physiotherapists are able to pick up simple signing, it will greatly aid in their communication with their clients with learning disabilities.
Inclusive Communication
Inclusive communication is a means of sharing information so that everybody can understand it. For service providers, it means that you understand that people understand and express themselves in different ways. Inclusive communication refers to:
- Written information
- Face to face
- Telephone
- Online information
Inclusive communication aims to ensure that people with communication support needs are able to live independently, access services easily and are able to participate in the wider community.
A person with communication support needs may need support with understanding, expressing themselves and interacting with others. As physiotherapists we need to use other methods of communication so that our patients understand what we are saying to them and are able to express themselves.
A person with communication support need may:
- Avoid services completely.
- Not turn up for an appointment.
- Respond only to some advice given or nodding their head as though they understand.
- Ask lots of repeated questions.
- Give irrelevant, rambling or unclear sentences.
- Have challenging behaviours.
- Appear bored or unable to maintain attention.
- Have difficulty describing feelings or events, may be explained in sentences that do not make sense.
- Express very strong emotions that may seem inappropriate to the situation such as anger or frustration (The Scottish Government 2011)
- (TO INSERT COMMUNICATION FORUM SCOTLAND DIAGRAM HERE)
The six principles of inclusive communication are:
(TO INSERT 6 PRINCIPLES DIAGRAM)
Acquiring informed consent[edit | edit source]
It is imperative to always acquire informed consent from the patients before commencing assessments or treatments. Informed consent is defined as: ‘an individual is always presumed to be competent, or to have mental capacity to enter into a particular transaction, until the contrary is proved’ (Law Society – BMA 1995). Therefore, you should bear in mind that no one, even the parents, can consent to or refuse treatment on behalf of another adult who lacks capacity to consent. Some people will never be able to make decisions, but judgement must not be made until all practicable steps have been taken to help the patient. You must only regard a patient as lacking capacity once it is clear that after all appropriate help and support, they cannot understand, retain, use or weigh up the information needed to make that decision, or communicate their wishes.
Therefore, consent can be waived, but only under certain conditions:
- To preserve life, health or well being of the person e.g. in emergency situations
- If the patient is being held under the Mental Health Act
- It is agreed during a formal ‘Best Interests’ meeting (a multidisciplinary meeting including all professionals/ carers/family/patient involved in the care of the patient) that a particular intervention was in accordance with best practice, which includes best medical interests and the patient’s general being, wishes, and needs.
Who can give informed consent? Individuals who received an understandable explanation of the following:
- What will happen and why it is necessary in very simple terms
- The benefits and risks of the treatment and what alternatives are available
- What will happen if the patient does not consent, and
- Being able to retain what you have discussed with them and able to make a decision
Never ever coerce a patient into making decisions, just because you believe that the patient should have the treatment. If controversial circumstances are involved, decisions around best interests should be made via the court.
To find out whether the individual has the capacity to give informed consent, it is essential to:
- Elicit what skills or knowledge the patient may require to exercise capacity
- Find out what support and information the patient requires to achieve capacity, and
- Involve someone who knows the patient well and their level of communication
What does capacity to give informed consent mean?
Capacity refers to the ability to use and understand information to make a particular decision at a particular time, and can vary in the same person for different decisions. Understanding depends on cognitive abilities, effective communication and accessible information. A person with capacity has the right to refuse treatment, whereas in the case of an adult who lacks capacity, the health professional has a duty to provide treatment and care in the best interests of that adult, even if the person does not agree.
Where the patient has never been competent, relatives, carers and friends may be best placed to advise on the patient's needs and preferences. It is good practice to consult with people close to the patient to gain agreement unless the person had good reasons that they would not wish those people to be consulted, or the situation is urgent. If an incompetent patient has clearly indicated in the past, while competent, that they would refuse treatment in certain circumstances (an 'advance refusal'), and those circumstances arise, you must abide by that refusal.
http://www.dvh.nhs.uk/for-patients-and-visitors/learning-disabilities/consent/
http://www.gmc-uk.org/learningdisabilities/237.aspx http://www.intellectualdisability.info/how-to-guides/articles/consent-and-people-with-intellectual-disabilities-the-basics
Someone with severe learning disability is thought to be unable to make a decision if they can't:
- understand information about the decision
- remember that information
- use that information to make a decision
- communicate their decision by talking, using sign language or by any other means
http://www.nhs.uk/Conditions/Consent-to-treatment/Pages/Capacity.aspx
Health literacy
[edit | edit source]
Definition of health literacy[edit | edit source]
The need for health literacy[edit | edit source]
Health literacy in numbers[edit | edit source]
National and international actions[edit | edit source]
Techniques and tools/strategies[edit | edit source]
Impact of disability on general population[edit | edit source]
Policies and guidelines
[edit | edit source]
Case study
[edit | edit source]
Conclusion
[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Scottish Commission for Learning Disabilities. Learning disability statistics scotland, 2015. SCLD: Glasgow, 2016.fckLRhttp://www.scld.org.uk/wp-content/uploads/2016/08/2015-Learning-Disability-Statistics-Scotland-report-1.pdf (accessed 2 Jan 2017).
- ↑ Jansen DEMC, Krol B, Goothroff W, Post D. People with intellectual disability and their health problems: a review of comparative studies. Journal of intellectual disability research. 2004:48;2;93-102. Available from:http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2788.2004.00483.x/epdf (accessed 18 Jan 2017).
- ↑ Chadwick DD, Jolliffe J. A pilot investigation into the efficacy of a signing training strategy for staff working with adults with intellectual disabilities. British Journal of Learning Disabilities. 2009,37:1; 34–42.