Urinary Tract Infection
Introduction[edit | edit source]
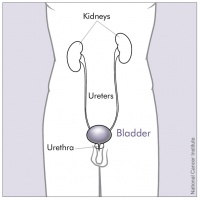
A urinary tract infection is an infection in any part of your urinary system, which includes the bladder, urethra, ureters (urine tubes) and kidneys. If untreated, UTIs can lead to kidney infection which can be very serious. UTIs are caused by microbes, mainly bacteria, but also fungi and viruses[1].
Normally, bacteria that enters the urinary tract is rapidly removed by the body before symptoms are present, but sometimes this bacteria overcomes the natural defences of the body, resulting in an infection. This infection may involve the lower urinary tract only, or both the lower and upper urinary tracts[2]. The upper urinary tract is made up of the kidneys and the ureters, while the lower urinary tract is made up of the bladder and urethra [2].
Types of urinary tract infections (UTIs)[edit | edit source]
The different types of UTI can include:
- Urethritis – infection of the urethra
- Cystitis – infection of the bladder
- Pyelonephritis – infection of the kidneys
- Vaginitis – infection of the vagina.[3]
Etiology[edit | edit source]
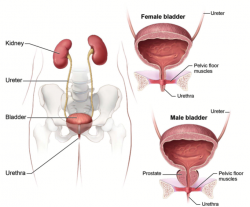
Pathogenic bacteria ascend from the perineum, causing the UTI. Women have shorter urethras than men and therefore are far more susceptible to UTI.
A major risk factor for UTI is catheter use. Sexual intercourse and the use of spermicides and diaphragms are also risk factors for UTI. Frequent pelvic exams and the presence of anatomical abnormalities of the urinary tract can also predispose one to a UTI.
UTIs are very common after a kidney transplant. The two triggers include the use of immunosuppressive drugs and vesicoureteral reflux. Other risk factors include the use of antibiotics and diabetes mellitus[4].
Epidemiology[edit | edit source]
An estimated 150 million UTIs occur every year world-wide, adding to $6 billion in health care costs [5].
Across all age groups, the incidence of UTI is higher in women than men, with a lifetime risk greater than 50% for women [2]. Women are especially prone due to anatomical reasons: the urethra is shorter allowing bacteria quicker access to the bladder and the urethral opening is near bacteria sources, such as the anus and vagina [6].
UTI is frequent in young and sexually active women with reported incidence rates ranging from 50-70% per person per year[2]. Pregnancy does not show an increased risk compared to typical women, but a UTI is more likely to travel to the kidneys in pregnant women due to hormonal and positional changes [6].
UTI is one of the most commonly diagnosed infections in older adults and the most frequently diagnosed infection in long-term care residents, with over 10% of women over 65 years old reported having a UTI within the past 12 months [2].
Characteristics/Clinical Presentation[edit | edit source]
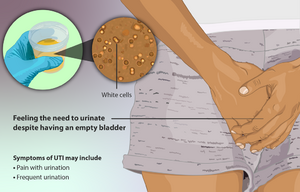
Some of the symptoms of UTIs include:
- Wanting to urinate more often and urgently, if only a few drops
- Burning pain or a ‘scalding’ sensation when urinating
- Feeling that the bladder is still full after urinating
- Pain above the pubic bone
- Cloudy, bloody or very smelly urine.
If infection reaches the kidneys, prompt medical attention is needed. In addition to the general symptoms of UTIs, a person with a kidney infection can also experience:
- Chills
- Fever
- Loin (lower abdominal) pain
- Pain in the back
- Vomiting.[3]
Associated Co-morbidities[edit | edit source]
Conditions or diseases that can be associated with UTIs include the following [6]:
- Diabetes Mellitus
- Hypertension
- Kidney stones
- Bowel incotinence
- Prostatic obstruction
- Immunological disorders
- Spinal cord injuries
- Congenitial urinary tract anomalies
Other risk factors include [7]:
- Urinary catheterization
- Residency in a nursing home or hospitalization
- Immobility
- Previous urologic surgery
- Obstructive urinary tract problems
- Gout
- Hypertension
- Sexual Activity
Urinary catheterization interferes with the body's ability to clear microbes from the urinary tract, therefore, increasing the risk for bacteria; to reduce the risk of a UTI, the Infectious Diseases Society of America recommends using catheters for the shortest time possible [6]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Due to bacteria possibly being found in urine of healthy individuals, a UTI is diagnosed based on symptoms of the individual and a laboratory test. The health care provider will request a "midstream" urine sample and then send it to a laboratory [6]. In the case of recurring infections or in a hospital environment, the urine sample may be cultured to identify the bacteria growing. Sensitivity tests may also be ordered by the health care provider to interpret the most efficient medication for treatment [6].
Confirmation of a diagnosis of UTI includes a positive urine culture (≥ 105 CFU/mL) with no more than 2 uropathogens and pyuria [8]. Dipstick tests are easy to perform in a clinic and used often when testing for UTI [8].
Typically, symptoms of a UTI will conclude within 24-48 hours after treatment. A UTI is considered recurrent if the condition presents more than twice in 6 months [1]. Additional tests include the following: kidney and bladder ultrasound, voiding cystourethrogram, computerized tomography (CT) scan, MRI, radionuclide scan, urodynamics, and cystoscopy [6].
Systemic Involvement[edit | edit source]
Urinary Tract infections that are left untreated may lead to many complications, including urosepsis, systemic inflammatory response syndrome (SIRS), and chronic kidney infections. Sepsis associated with UTIs often requires hospitalization[8]. Urosepsis spreads into the bloodstream from its origin in the urinary tract. Kidney infections also progress to the blood stream, referred to as septicemia[6]. This complication can be life threatening. Systemic inflammatory response syndrome can also become life threatening if treatment fails. SIRS is usually the first incidence of multi-organ failure[9].
Medical Management[edit | edit source]
The type of bacteria and the patient's history play a role in the choice of medication and length of treatment determined by the health care provider. As these infections are usually caused by bacteria, antibiotics are used to treat UTIs. Removing predisposing factors are also considered if possible- draining urine collections, removing or changing catheters[5]. Health care providers will sometimes perform a sensitivity test and analyze the results to select the most effective antibiotic specific to the patient based on the site of infection and severity of illness[5]. Urinary tract infections are most commonly treated by antibiotic prescription. Frequently prescribed antibiotics include[1]:
- Nitrofurantoin
- Amoxicillin
- Trimethoprim
- Fluoroquinolones
Antibiotics are usually taken anywhere from 3 days to 10 days, depending on severity of symptoms, comorbidities, complications of infection, and dosage [2] [1]. Overutilization of antibiotics is a common issue, particularly in hospitals and long term facilities, which may cause patients to develop resistance to the medication over time [2].
Alternative treatment includes the use of probiotics, ensuring proper hydration, drinking cranberry juice, and urinating frequently [10] [8][6]. Using a heating pad on the patient’s lower back or abdomen may also help the symptoms of the UTI[11]. Surgery may be required in the presence of an anatomical abnormality [1].
Physical Therapy Management[edit | edit source]
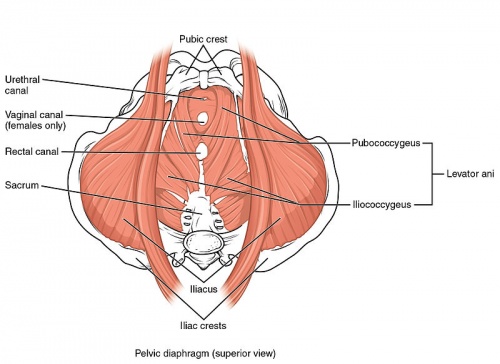
Physical therapists that are trained in pelvic floor dysfunction can greatly improve a UTI patient’s quality of life. A typical approach includes training pelvic floor musculature, manipulative techniques, local heat, breathing and relaxation techniques, postural education, muscle coordination reeducation, and behavioral therapy[12]. Therapists are also encouraged to educate the patient on drinking and voiding schedules to ensure consistency[13]. Treatments and patient education have been found to improve efficiency of emptying the bladder, create better bowel habits, and promote full relaxation of the pelvic-floor when voiding[12]. All of these factors may lead to a decreased incidence and reoccurrence of UTIs.
For those patients in the hospital, recent studies have shown that mobilization of patients with a catheter is safe and is not associated with urinary-related adverse effects, including urinary tract infections[14].
Differential Diagnosis[edit | edit source]
The American Urological Association has identified conditions that can cause symptoms similar to UTI, including[5]:
- STDs: Genital Herpes, Gonorrhea, Chlamydia, Trichomonas
- Inflammatory disorders: Vaginitis, Prostatitis, Urethritis
- Nephrolithiasis (Kidney Stones)
- Trauma
- Genitourinary Tuberculosis
- Genitourinary Neoplasm
- Intra-abdominal Abscess
- Yeast Infection
Variation in symptom presentation:
Post-menopausal women present with constitutional symptoms, such as abdominal pain, back pain, chills, and constipation [2].
Nursing home patients present with nonspecific symptoms, such as confusion and a decline in functional status.
Children are usually the hardest to diagnose due to the their vagueness of symptoms. The typical adult symptoms of frequency, urgency, and dysuria are usually absent in children. Young children sometimes present with irritability, poor feeding, vomiting, or jaundice. UTI should be considered in any child between two months and two years of age with fever that doesn't have an identifiable source of infection [10].Young children with incontinence and abdominal pain should also be checked [10].
Case Reports/ Case Studies[edit | edit source]
1. Physiotherapy For Women With Recurrent Urinary Tract Infection: A Promising Approach - http://www.ics.org/Abstracts/Publish/218/000223_poster.pdf
2. Pelvic floor therapy in girls with recurrent UTIs - http://www.ncbi.nlm.nih.gov/pubmed/9634033
Resources[edit | edit source]
American Urological Association
NYU School of Medicine Department of Urology
European Association of Neurology
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Rosenblum, N. Recurrent Urinary Tract Infections. Urology. Available at: http://www.med.nyu.edu/urology/patient-care-information/conditions-we-treat/recurrent-urinary-tract-infections
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Rowe, TA, Juthani-Mehta, M. Urinary tract infection in older adults. Aging Health. 2013;9(5).
- ↑ 3.0 3.1 Better Health UTIs Available:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/urinary-tract-infections-uti (accessed 13.5.2022)
- ↑ Bono MJ, Reygaert WC. Urinary tract infection. InStatPearls [Internet] 2021 Jun 23. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK470195/ (accessed 13.5.2022)
- ↑ 5.0 5.1 5.2 5.3 M, Pontari. Adult UTI. Advancing Urology. Available at: www.auanet.org/education/adult-uti.cfm
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Urinary Tract Infections in Adults. Urologic Diseases. 2013. Available at: http://www.niddk.nih.gov/health-information/health-topics/urologic-disease/urinary-tract-infections-in-adults/pages/ez.aspx.
- ↑ Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. 5th ed. St. Louis, MO: Elsevier/Saunders; 2012.
- ↑ 8.0 8.1 8.2 8.3 Mody, L, Juhani-Mehtta, M. Urinary Tract Infections in Older Women: A Clinical Review. JAMA. 2014;311:844–854.
- ↑ Grabe, M. Guidelines on Urological Infections. Urological Infections. Available at: http://uroweb.org/wp-content/uploads/19-urological-infections_lr2.pdf.
- ↑ 10.0 10.1 10.2 Becknell, B, Schober, M, Korbel, L, Spencer, JD. The Diagnosis, Evaluation and Treatment of Acute and Recurrent Pediatric Urinary Tract Infections. Expert Review of Anti-infective Therapy. 2015;13(1):81–90.
- ↑ Urinary Tract Infections in Adults. Urologic Diseases. 2013. Available at: http://www.niddk.nih.gov/health-information/health-topics/urologic-disease/urinary-tract-infections-in-adults/pages/ez.aspx.
- ↑ 12.0 12.1 Souza, EL, Figueiredo, EM, Velloso, FB, Geo, MS. Physiotherapy For Women with Recurrent Urinary Tract Infection: A Promising Approach. International Continence Society. 2013:223.
- ↑ De Paepe, H, Hoebeke, P, Renson, C, et al. Pelvic-floor therapy in girls with recurrent urinary tract infections and dysfunctional voiding. British Journal of Urology. 1998;3:10–9113.
- ↑ Lima, NP, Cardim da Silva, GM, Park, M, Pires-Neto, RC. Mobility therapy and central or peripheral catheter-related adverse events on an ICU in Brazil. J bras pneumol. 2015;41(3):225–230.