Behavioral problems in children
Original Editor - Redisha Jakibanjar, Top Contributors - Redisha Jakibanjar, Lucinda hampton and Kim Jackson
Introduction[edit | edit source]
All young children can be naughty, defiant and impulsive from time to time, which is perfectly normal. However, some children have extremely difficult and challenging behaviours that are outside the norm for their age.
These problems can result from temporary stressors in the child’s life, or they might represent more enduring disorders. The most common disruptive behaviour disorders include oppositional defiant disorder (ODD), conduct disorder (CD) and attention deficit hyperactivity disorder (ADHD). Boys are more likely than girls to suffer from behavioural disorders.
Treatment options include parent management training, cognitive behaviour therapy, medication and treatment for associated problems.[1]
Mental health and Emotional Disorders[edit | edit source]
Mental health disorders (MHD) are very common in childhood. They include emotional-obsessive-compulsive disorder (OCD), anxiety, depression, ODD, CD, ADHD)or developmental (speech/language delay, intellectual disability) disorders or autistic spectrum) disorders[2].
Emotional and behavioural problems (EBP) or disorders (EBD) can also be classified as either “internalizing” (emotional disorders eg depression and anxiety) or “externalizing” (eg ADHD and CD)[2].
Oppositional Defiant Disorder[edit | edit source]
Around one in ten children under the age of 12 years are thought to have oppositional defiant disorder (ODD), with boys outnumbering girls by two to one. Some of the typical behaviours of a child with ODD include:
- Easily angered, annoyed or irritated
- Frequenttemper tantrums
- Argues frequently with adults, particularly the most familiar adults in their lives, such as parents
- Refuses to obey rules
- Seems to deliberately try to annoy or aggravate others
- Low self-esteem
- Low frustration threshold
- Seeks to blame others for any misfortunes or misdeeds.[1]
Conduct Disorder[edit | edit source]
Children with conduct disorder (CD) are often judged as ‘bad kids’ because of their delinquent behaviour and refusal to accept rules. Around five per cent of 10 year olds are thought to have CD, with boys outnumbering girls by four to one. Around one-third of children with CD also have attention deficit hyperactivity disorder (ADHD).
Some of the typical behaviours of a child with CD may include:
- Frequent refusal to obey parents or other authority figures
- Repeated truancy
- Tendency to use drugs, including cigarettes and alcohol, at a very early age
- Lack of empathy for others
- Being aggressive to animals and other people or showing sadistic behaviours including bullying and physical or sexual abuse
- Keenness to start physical fights
- Using weapons in physical fights
- Frequent lying
- Criminal behaviour such as stealing, deliberately lighting fires, breaking into houses and vandalism
- A tendency to run away from home
- Suicidal tendencies – although these are more rare.
Risk factors[edit | edit source]
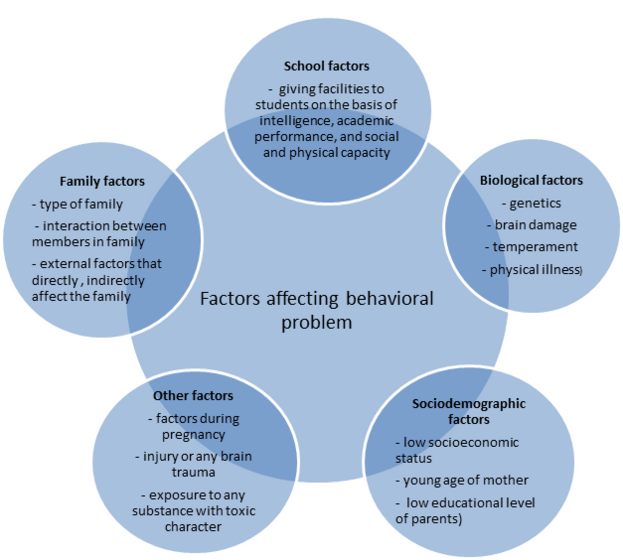
See diagram below
Preventive measures that have been researched for controlling the risk of childhood emotional and behaviour problems include breastfeeding, avoiding second-hand smoke exposure in non-smoker youths and intensive parenting interventions[2].
Consequences of Behavioural and Emotional Disorders[edit | edit source]
Childhood behavioural and emotional disorders (EBD) have significant negative impacts on the society, in the form of direct behavioural consequences and costs, and on the individual, in the form of poor academic, occupational and psychosocial functioning and on the family. The costs to society include the trauma, disruption and psychological problems caused to the victims of crime or aggression in homes, schools and communities, together with the financial costs of services to treat the affected individuals, including youth justice services, courts, prison services, social services, foster homes, psychiatric services, accident and emergency services, alcohol and drug misuse services, in addition to unemployment and other required state benefits.
Prevention and management of EBD is not easy and it requires an integrated multidisciplinary effort by healthcare providers at different levels to be involved in the assessment, prevention and management of affected individuals, and also to provide social, economic and psycho-emotional support to the affected families.
There is increasing evidence base for several psychosocial interventions but less so for pharmacological treatment apart from the use of stimulants for ADHD. [2]
Treatment[edit | edit source]
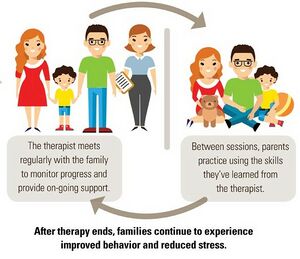
Treatment is usually multifaceted and depends on the particular disorder and factors contributing to it, but may include:
- Parental education – for example, teaching parents how to communicate with and manage their children.
- Family therapy – the entire family is helped to improve communication and problem-solving skills.
- Cognitive behavioural therapy – to help the child to control their thoughts and behaviour.
- Social training – the child is taught important social skills, such as how to have a conversation or play cooperatively with others.
- Anger management – the child is taught how to recognise the signs of their growing frustration and given a range of coping skills designed to defuse their anger and aggressive behaviour. Relaxation techniques and stress management skills are also taught.
- Support for associated problems – for example, a child with a learning difficulty will benefit from professional support.
- Encouragement – many children with behavioural disorders experience repeated failures at school and in their interactions with others. Encouraging the child to excel in their particular talents (such as sport) can help to build self-esteem.
- Medication – to help control impulsive behaviours[1].
Early Identification[edit | edit source]
Early detection is the important path for the early intervention of the problem.It helps improve the QOL of the individual and decrease burden created to family society and nation.
- Behavioral problem can be identified in preschool age group and the period around the transition to school has been identified as a particularly effective time to intervene for the behavioral problem.
- Early intervention programs for individuals with early signs of mental problem have been highlighted as crucial and effective strategies to prevent development of mental disorders[3].[4]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Better health Behavioural disorders in children Available: https://www.betterhealth.vic.gov.au/health/healthyliving/behavioural-disorders-in-children(accessed 8.10.2021)
- ↑ 2.0 2.1 2.2 2.3 Ogundele MO. Behavioural and emotional disorders in childhood: A brief overview for paediatricians. World journal of clinical pediatrics. 2018 Feb 8;7(1):9. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5803568/https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5803568/ (accessed 8.10.2021)
- ↑ Jetishi P. Evaluation Of Emotional And Behavioral Problems In Preschool Children Aged 2-5, In The City Of Pristina. European International Virtual Congress of Researchers. 2016:25-34
- ↑ Reid K, Littlefield L, Hammond SW. Early intervention for preschoolers with behaviour problems: Preliminary findings for the Exploring Together Preschool Program. Australian e-Journal for the Advancement of Mental Health (AeJAMH),. 2008;7(1):1-15.