Cognitive Behavioural Therapy
Original Editor - Rachael Lowe
Top Contributors - Scott Buxton, Kim Jackson, Anthonia Abraham, Vidya Acharya, Patti Cavaleri, Shaimaa Eldib, Rachael Lowe, Mariam Hashem, WikiSysop and Claire Knott
What is Cognitive Behavioural Therapy?[edit | edit source]
Cognitive Behavioural Therapy (CBT) is a method that can help manage problems by changing the way patients would think and behave. It is not designed to remove any problems but help manage them in a positive manner [1][2].
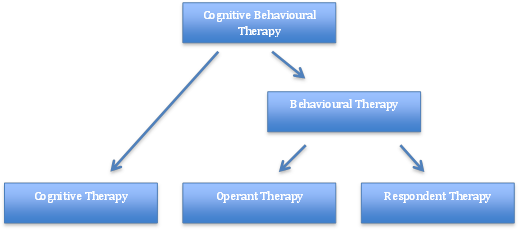
Behaviour therapy (BT) was developed in the 1950’s independently in three countries: South Africa, USA and England [3]. It was further developed to Cognitive Therapy (CT) in the 1970’s by Dr Aaron Beck with its main application on people with depression, anxiety and eating disorders [1][4]. However, the main evidence today focuses on CBT, after the merging of BT and CT in the late 80’s [5].
Fig.2 - Breakdown of CBT theory
The Cognitive Behavioural Therapy Model[edit | edit source]
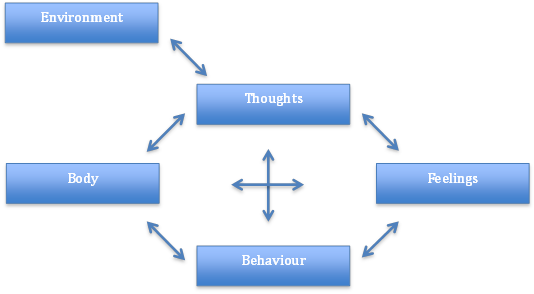
Fig.3 - Factors involved within the Cognitive Behavioural Therapy Model
Aaron Beck and Christine Padesky first recognised this CBT model in the 1970s [6].
How it is Used[edit | edit source]
Negative thoughts (e.g., "My back pain is uncontrollable" --> Negative feelings (e.g., depression, anger) and maladaptive health behaviours (e.g., skipping treatment sessions) --> Reinforcing negative cycle.
If one negative thought can be changed or better understood, then it can break down this negative cycle. This can be addressed through education and methods to manage symptoms [6]. This is address through various approaches including cognitive restructuring, behavior activation, exposure, and problem-solving strategies[7].
CBT can be delivered through individualized sessions or group sessions. A recent integrative review found that online formats of CBT may be comparable with traditional formats[8].
CBT and Chronic Pain[edit | edit source]
CBT has been increasingly studied and considered as an intervention as part of a multimodal approach for those with chronic pain. CBT has been studied to address activity pacing, sleep hygiene, pain perception, disability, mood, fatigue [9] and catastrophization[8]. Recent clinical trials and integrative reviews found 6-10 weeks of CBT had positive effects on pain intensity but further research is need to identify optimal dosage[8][9]
Cognitive behavioral therapy (CBT) can help people with chronic pain to improve their physical function by:
- Setting realistic goals: CBT can help people to set realistic goals for their activity level, such as walking for 30 minutes a day or doing some light stretching exercises. This can help people to gradually increase their activity level and to overcome fear of movement.
- Developing coping strategies: CBT can help people to develop strategies for managing pain during activity, such as using relaxation techniques or distraction techniques. This can help people to stay active and to avoid becoming more disabled by their pain.
Members of the Rehabilitation Team in the use of CBT[edit | edit source]
The roles of other members of the rehabilitation team in the use of cognitive behavioral therapy (CBT) can vary depending on the specific team and the needs of the individual patient. However, some common roles include:
- Therapist: The therapist is the primary provider of CBT and is responsible for conducting the therapy sessions. They will work with the patient to identify and challenge negative thoughts and beliefs, and develop coping strategies for managing difficult emotions.
- Physiatrist: The physiatrist is a doctor who specializes in physical medicine and rehabilitation. They can provide medical oversight for CBT and help to ensure that the patient is safe and progressing well.
- Occupational therapist: The occupational therapist can help the patient to develop adaptive strategies for daily living activities, such as dressing, bathing, and eating. They can also provide support and encouragement during the rehabilitation process.
- Physical therapist: The physical therapist can help the patient to improve their range of motion, strength, and balance. They can also provide exercises that can help to manage pain and improve function.
- Social worker: The social worker can provide support and counseling to the patient and their family. They can also help to connect the patient with community resources, such as financial assistance or transportation services.
- Nurse: The nurse can provide education and support to the patient and their family. They can also monitor the patient's physical health and provide medication management.
In addition to these specific roles, all members of the rehabilitation team can play a role in supporting the patient's overall well-being and helping them to achieve their rehabilitation goals. They can do this by providing encouragement, listening to the patient's concerns, and helping them to stay motivated.
It is important to note that the roles of the different members of the rehabilitation team may overlap. For example, the therapist may also provide support and counseling to the patient, and the social worker may also help to coordinate the patient's care. The specific roles of each team member will be determined by the needs of the individual patient and the goals of the rehabilitation team.[10]
The role of the physiotherapist in CBT[edit | edit source]
Physiotherapists can play a key role in the delivery of CBT for pain management. They can:
- Provide education about pain: Physiotherapists can educate people about the nature of pain and how it can affect their physical function. This can help people to understand their pain and to develop realistic expectations for their recovery.
- Teach relaxation techniques: Physiotherapists can teach people relaxation techniques, such as deep breathing or progressive muscle relaxation. These techniques can help people to manage pain and to reduce stress, which can also improve physical function.
- Help people to develop coping strategies: Physiotherapists can help people to develop coping strategies for managing pain during activity. This can include teaching people how to use relaxation techniques, distraction techniques, or other strategies that have been found to be helpful.
Effectiveness of CBT for pain management[edit | edit source]
There is a growing body of evidence to support the effectiveness of CBT for pain management. A systematic review of 60 randomized controlled trials found that CBT was effective in reducing pain intensity, improving function, and reducing disability in people with chronic pain.[11]
Limitations of CBT for pain management[edit | edit source]
CBT is not a miracle cure for pain, and it is not effective for everyone. However, it is a safe and effective treatment option for many people with chronic pain. Some of the limitations of CBT include:
- It can be time-consuming and expensive.
- It requires a motivated and committed patient.
- It may not be effective for all types of pain.[12]
Overall, CBT is a safe and effective treatment option for many people with chronic pain. It can help to reduce pain intensity, improve function, and reduce disability[13]. Physiotherapists can play a key role in the delivery of CBT for pain management by providing education, teaching relaxation techniques, and helping people to develop coping strategies.
References[edit | edit source]
- ↑ 1.0 1.1 Beck, J., 1995. Cognitive Therapy: Basics and Beyond. Guildford Press: New York
- ↑ NHS Choices, 2012. Cognitive behavioural therapy. [online] Available at:http://www.nhs.uk/conditions/cognitive-behavioural-therapy/Pages/Introduction.aspx[Accessed 8th Jan 2014]
- ↑ Öst, L.G., 2008. Efficacy of the third wave of behavioral therapies: a systematic review and meta-analysis. Behaviour research and therapy, 46(3): 296–321
- ↑ Hayes, S.C., 2004. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy, 35: 639–665
- ↑ Roth, A., Fonagy, P. “What works for whom? A critical review of psychotherapy research”. 2nd ed. Guilford Press: New York 2005
- ↑ 6.0 6.1 Beck, A.T., 1976. Cognitive Therapy and the Emotional Disorders. New York: International Universities Press
- ↑ Wenzel A. Basic Strategies of Cognitive Behavioral Therapy. Psychiatr Clin North Am. 2017 Dec;40(4):597-609. doi: 10.1016/j.psc.2017.07.001. Epub 2017 Aug 18.
- ↑ 8.0 8.1 8.2 Knoerl, R., Lavoie Smith, E. M. and Weisberg, J. (2016) ‘Chronic Pain and Cognitive Behavioral Therapy: An Integrative Review’, Western Journal of Nursing Research, 38(5), pp. 596–628. doi: 10.1177/0193945915615869.
- ↑ 9.0 9.1 Chong HY, McNamee P, Bachmair EM, Martin K, Aucott L, Dhaun N, Dures E, Emsley R, Gray SR, Kidd E, Kumar V. Cost-effectiveness of cognitive behavioural and personalised exercise interventions for reducing fatigue in inflammatory rheumatic diseases. Rheumatology. 2023 Feb 27.
- ↑ Chand SP, Kuckel DP, Huecker MR. Cognitive Behavior Therapy. [Updated 2023 May 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470241/
- ↑ Morley, S., Williams, A., & Eccleston, C. (1999). Systematic review and meta-analysis of randomised controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults. Pain, 80(3), 159-169.
- ↑ Eccleston, C., Crombez, G., & Williams, A. (2006). Psychological therapies for chronic pain. The Cochrane Database of Systematic Reviews, 3, CD003968.
- ↑ Morley, S. (2010). Cognitive behaviour therapy for chronic pain: A guide for practitioners. London: Routledge