Bursitis
Original EditorAndrea Nees
Top Contributors - Hamelryck Sascha, Aarti Sareen, Andrea Nees, Admin, Rachael Lowe, Kim Jackson, Wanda van Niekerk, Chloe Wilson, Blessed Denzel Vhudzijena and Rebecca Willis
Definition/Description[edit | edit source]
Bursitis is the inflammation of a bursa, a small fluid filled sac that sits between muscles, tendons and bones to reduce friction[1]. Common sites include[1]:
- Subacromial bursitis
- Olecranon bursitis - students elbow
- Prepatellar Bursitis - housemaid's knee
- Infrapatellar bursitis - clergyman's knee
- Popliteal bursitis - Baker's Cyst or popliteal cyst
- Trochanteric bursitis of hip
- Achilles bursitis
- Retrocalcaneal bursitis
- Ischial bursitis - weaver's bottom
- Iliopsoas bursitis
- Pes anserine bursitis
Clinically Relevant Anatomy[edit | edit source]
A Bursa appears at a junction of a tendon on the bone. A bursa is filled with a thin layer of synovial fluid. It protects and brakes the shocks of the joint and allows the structures near the bursa to move with minimal friction. They have different measures and are mostly flattened. Humans have approximately 160 bursae.[1]
Mechanism of Injury / Pathological Process[edit | edit source]
When a Bursa gets inflamed, it swells, develops friction and starts irritating the muscle tendon it is supposed to protect. This way the bursa and muscle tendon get more and more irritated.
These issues lead to bursitis and tendinitis.
Below is a summary of causes for bursitis, with the example for the olecranon bursa[1].
- Overuse of the joint: for example vacuuming for hours on end
- Repetitive strain: for example picking up and lifting heavy loads
- Trauma: by falling on your elbow or bumping it against something. This is the most common cause.
- Pressure: leaning on the elbow at a desk is a common cause of bursitis among students
- Bacterial infection: from an unattended wound (this is called septic bursitis)
- Other inflammatory diseases: e.g., Gout; the gout crystals can form in the bursa and cause the inflammation.
Epidemiology/Etiology[edit | edit source]
Bursitis can be acute, chronic or septic[2]. Bursitis may occur[2]:
- Mainly by constant friction, thumping or pressure
- The inflammation of the bursa frequently appears in combination with tendinitis
- By an overuse injury or a trauma, especially when pulling and pushing heavy items
- After a forced period of rest
- There also can be an underlying rheumatic condition
- Diabetes, osteoarthritis and disability of the thyroid gland can be associated with bursitis
Clinical Presentation[edit | edit source]
The presentation will depend on the location of the bursitis. There will likely be pain and discomfort over the affected area, and there will often be visible and/or palpable swelling[3].
Diagnostic Procedures[edit | edit source]
In most cases, bursitis can be diagnosed by physically examining the patient.
Inspection[3][edit | edit source]
- Redness and warmth can be signs of bursitis, but these symptoms are harder to spot when treating a Bursa that is not located superficially under the skin.
- Local tenderness or stiffness.
- Swelling can occur when inflammation gets worse.
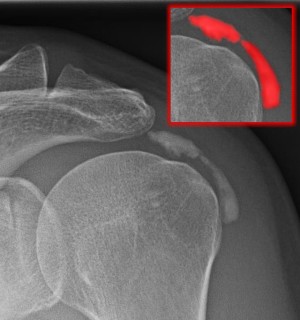
X-ray[edit | edit source]
- Can rule out arthritis and bone deformities[2]
- Can sometimes confirm the presence of following substances inside the bursa (By which it become visible in X-ray)
- Gout crystals
- Calcifications: When the condition is chronic or recurrent.
Bursa Fluid Punction[edit | edit source]
- Can rule out infections.
Management / Interventions[4][5][edit | edit source]
Bursitis Due to Movement/Activity (Without Infection)[edit | edit source]
- Rest the affected joint/ bursa
- Ice packages
- NSAID’s ( non steroid anti inflammatory drugs)
- Injections with steroid agents
- When improvement is noticeable, a gradual increase in exercise and activities is recommended.
Note: Resting the affected joint does not mean immobilizing it, this could hold a risk towards adhesive capsulitis (especially in the shoulder).
Bursitis Due to Infection (= Septic Bursitis)[edit | edit source]
- Antibiotics
- Aspiration of the infected bursa fluid with the use of a sterile needle should be repeated approximately every 3 days
- Never inject with steroids!
Note: When the measures mentioned above are inadequate surgical interventions may be necessary
in case of the following factors:
- Surgical removal of the bursa is recommended in case of tuberculous bursitis
- Surgical incision and drainage are recommended in case of :
- Failure of adequately aspirating by needle
- Bursa site inaccessible to multiple needle aspirations
- Forming of abscess or necrosis
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Johar, S., Bursitis. In: Bracker, MD., Achaar SA., Pana, AL., Taylor KS., editors. 5 Minute Sports Medicine Consult [Internet]. Wolters Kluwer Health; 2011. p. 56-57
- ↑ 2.0 2.1 2.2 Reilly, D., Kamineni, S., Olecranon bursitis. J Shoulder Elbow Surg [Internet]. 2016 [cited 2023 May 22]; 25:158-167
- ↑ 3.0 3.1 NHS. Bursitis [Internet]. 2020 [cited 2023 May 22]
- ↑ Ce´dric Perez1 ET AL. Infectious olecranon and patellar bursitis: short-course adjuvant antibiotic therapy is not a risk factor for recurrence in adult hospitalized patients: Journal of Antimicrob Chemotherapy 2010; 65: 1008–1014 (Evidence level B)
- ↑ S. P. Cohen ET AL. Corticosteroid injections for trochanteric bursitis: is fluoroscopy necessary? A pilot study. : British Journal of Anaesthesia 94 (1): 100–6 (2005)(Evidence level C)