Lacuna Infarcts ( Small Vessel Disease)
Introduction[edit | edit source]
A quarter of all ischaemic strokes (a fifth of all strokes) are lacunar type.
- Lacunar infarcts are small infarcts (2–20 mm in diameter) in the deep cerebral white matter, basal ganglia, or pons, presumed to result from the occlusion of a single small perforating artery supplying the subcortical areas of the brain.
- Although a recognised stroke subtype for over 50 years, the cause of lacunar ischaemic stroke, and whether it is different to cortical ischaemic stroke, remains under debate.
- Lacunar stroke is not benign; 30% of patients are left dependent, and scant long term data suggest that up to 25% of patients have a second stroke within 5 years.[1]
- Lacuna stroke are caused by Cerebral small vessel disease (cSVD) a term used for different pathological processes that affect the small vessels of the brain. cSVD has a crucial role in lacunar cerebral infarction and deep or cortical haemorrhages. In addition to cognitive decline and dementia, gait problems are also frequently associated with cSVD.[2]
This 3 minute video introduces the topic well
Clinically Relevant Anatomy[edit | edit source]
Lacunar infarctions are defined as small subcortical lesions with a size of less than 15 mm in diameter caused by occlusion of a penetrating artery from a large cerebral artery, most commonly from the Circle of Willis. These small arteries arise at sharp angles from major vessels and are anatomically prone to constriction and occlusion. Other common sources of these penetrating arteries include the middle cerebral artery and the basilar artery. For more information see Brain Anatomy
Image shows rotating brain, hypothalamus=red, amygdala=green, hippocampus/fornix=blue, pons=gold, pituitary gland=pink
The anatomic distribution of lacunar syndromes and infarctions is most commonly in the[4]
- Basal ganglia (globus pallidus, putamen, thalamus, and caudate)
- Pons,
- Subcortical white matter structures (internal capsule and corona radiate).
- These anatomical sites correspond to lesions at the lenticulostriate arteries, the anterior choroidal artery, thalamoperforant arteries, paramedian branches of the basilar artery, and the recurrent artery of Heubner from the anterior cerebral artery.
Lacunar Syndromes[4].[edit | edit source]
There are over 20 lacunar syndromes that have been described, but the most common ones are pure motor hemiparesis, pure sensory stroke, ataxic hemiparesis, sensorimotor stroke, and dysarthria-clumsy hand syndrome
Epidemiology[edit | edit source]
A US study found around 16% of first ischemic strokes in the United States are lacunar strokes and in the African-Americans communuties lacunar infarctions accounted for 22% of first-time ischemic stroke events.[4]
Another source reports that a quarter of all ischaemic strokes (a fifth of all strokes) are lacunar type[1].
Data comparing the frequency of lacunar strokes among different sexes, races, and worldwide populations are not readily accessible. One study in Japan does state that the frequency of lacunar infarcts has decreased since the 1960s due to more aggressive control of risk factors, primarily hypertension.[4]
Mechanism of Injury / Pathological Process[edit | edit source]
Dr. Miller Fisher first described arterial pathology under lacunes in the mid-1900s.
The pathophysiology of lacunar syndromes is inherently linked to 2 vascular pathologies of the penetrating arteries from major intracranial and extracranial arteries:
- thickening of the media resulting in decreased arterial diameter
- obstruction of the origins by microatheroma formation.
- Occlusive disease is caused by: chronic hypertension; diabetes, and other genetic factors. This causes medial thickening by fibrinoid necrosis, smooth muscle hypertrophy, and other connective tissue elements resulting in occlusion in these penetrating arteries (causing a small infarct in the region supplied by these small vessel).
- Collateral circulation in these distant pontine and subcortical areas is very limited, and multiple penetrating vessels are affected in these patients. Areas of infarct coalesce to form lake-like areas of infarcted/edematous brain tissue.
- Healing of this tissue ultimately forms "lacunes."[4]
Clinical Presentation[edit | edit source]
Most commonly, lacunar syndromes affect the elderly with long-standing hypertension. Otherwise, younger patients with lacunar syndromes may have a diagnosis of rare genetic conditions.[4]
The presenting complaint would usually not include cortical signs such as agnosia, aphasia, neglect, apraxia or hemianopsia.
These lacunar infarcts usually cause symptoms over minutes to hours but may progress with a stuttering course.
The clinical features and physical exam findings of lacunar syndromes are characteristic of the type of lacunar syndrome. The 5 most common of these are[4]
- Pure motor hemiparesis: weakness on one side of the body (face, arm, and leg) without cortical signs and sensory symptoms.
- Pure sensory stroke: unilateral numbness of the face, arm, and leg without cortical signs or motor deficits. All sensory modalities will be impaired.
- Ataxic hemiparesis: unilateral limb ataxia and weakness that is out of proportion to the strength/motor deficit. Possibly other ipsilateral cerebellar signs such has dysarthria, dysmetria, and nystagmus without exhibiting cortical signs.
- Sensorimotor stroke: weakness and numbness of the face, arm, and leg without cortical signs.
- Dysarthria-clumsy hand syndrome: This is the least common of all lacunar syndromes - facial weakness, dysarthria, dysphagia and dysmetria/clumsiness of one upper extremity.
Diagnostic Procedures[edit | edit source]
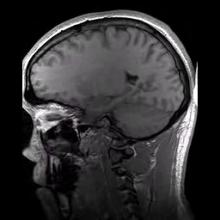
Initial evaluation of a suspected lacunar stroke involves brain imaging with a brain CT and MRI. Since small perforating arteries are hard to visualize with CTA and MRA, the diagnosis is made by matching a patient’s clinical features with a small, noncortical infarct seen on CT/MRI. The initial CT/MRI is also useful in ruling out life-threatening conditions such as intracerebral hemorrhage or herniation.
Usually recording a patient’s history of hypertension or diabetes and matching with clinical features and acute ischemia on brain imaging is all that is needed for diagnosis of lacunar infarcts. If the client is younger further investigation is warranted.[4]
Management / Interventions[edit | edit source]
The acute treatment of lacunar infarctions is like that of acute ischemic strokes.
Patients with lacunar infarctions are managed and seen by a care team including[4]
- Neurologist
- Physical medicine and rehabilitation physician
- physical, occupational, and social therapists
In the outpatient setting, a neurologist may treat neurologic deficits like ataxic and motor hemiparesis with muscle relaxants like baclofen, tizanidine, and/or botox.
Preventative measures with intense antihypertensive therapy, high dose statin therapy, and strict control of blood sugars must be initiated immediately after a lacunar ischemic event.
Outpatient rehabilitation therapy must be continued until a patient’s neurologic function can be returned to as close to his/her baseline prior to the infarction.
This 7 minute video nicely summarises Lacuna Strokes
Differential Diagnosis[edit | edit source]
Includes[4], not limited to
- large vessel ischemic strokes (most commonly in the middle cerebral artery territory)
- intracranial hemorrhages (subarachnoid bleeds, subdural bleeds, intracerebral hemorrhage)
- seizures,
- complicated migraine events.
Prognosis[edit | edit source]
The short-term prognosis of lacunar infarctions is better than other infarcts due to other stroke mechanisms. Multiple population-based epidemiological studies on lacunar infarcts have shown significantly better survival among patients who suffered from lacunar infarctions compared to those who suffered from non-lacunar infarcts.(case fatality of 0% to 3% within the first month and 3% to 9% within the first year, compared with 14% and 28%, respectively).[4]
References[edit | edit source]
- ↑ 1.0 1.1 Wardlaw JM. What causes lacunar stroke?.Available from: https://jnnp.bmj.com/content/76/5/617 (last accessed 28.12.2019)
- ↑ Cuadrado-Godia E, Dwivedi P, Sharma S, Santiago AO, Gonzalez JR, Balcells M, Laird J, Turk M, Suri HS, Nicolaides A, Saba L. Cerebral small vessel disease: a review focusing on pathophysiology, biomarkers, and machine learning strategies. Journal of stroke. 2018 Sep;20(3):302. Available from: https://www.j-stroke.org/journal/view.php?number=242 (last accessed 28.12.2019)
- ↑ Steve Jacques The lenticulostriate vessels and lacunar infarcts Available from: https://www.youtube.com/watch?v=7oTiprRp4dQ (last accessed 29.12.2019)
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 Venkataraman P, Lui F. Lacunar Syndromes. InStatPearls [Internet] 2018 Nov 15. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK534206/ (last accessed 28.12.2019)
- ↑ See hear say learn Lacuna Stokes Available from: https://www.youtube.com/watch?v=7-QmrnjC4gE (last accessed 29.12.2019)