Muscle Strain
Original Editor - The Open Physio project.
Top Contributors - Chrysolite Jyothi Kommu, Admin, Yesmine Gouddi, Kim Jackson, Uchechukwu Chukwuemeka, Lucinda hampton, 127.0.0.1, Rachael Lowe and WikiSysop
Introduction[edit | edit source]
A strain to the muscle or muscle tendon is the equivalent of a sprain to ligaments. A muscle strain occurs when muscle fibers cannot cope with the demands placed on them by exercise overload and leads to tearing of the fibers. It is a contraction-induced injury in which muscle fibers tear due to extensive mechanical stress. This mostly occurs as a result of a powerful eccentric contraction or over-stretching of the muscle. Therefore, it is typical for non-contact sports with dynamic characteristics such as sprinting and jumping.[1].
Muscle Injury Classification[edit | edit source]
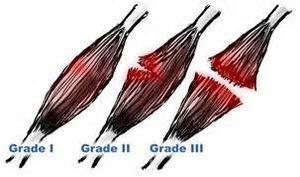
Muscle lesions are classified as grade I, II, and III based on the number of fibers disrupted according to clinical and imaging investigations[2][3]:
Grade I (mild) strains affect only a limited number of fibers in the muscle. There is no decrease in strength and there is a fully active and passive range of motion. Pain and tenderness are often delayed to the next day.
Grade II (moderate) strains have nearly half of muscle fibers torn. Acute and significant pain is accompanied by swelling and a minor decrease in muscle strength.
Grade III (severe) strains represent the complete rupture of the muscle. This means either the tendon is separated from the muscle belly or the muscle belly is actually torn in 2 parts. Severe swelling and pain and a complete loss of function are characteristic of this type of strain.
The above classification is the traditional muscle injury injury grading by consensus in Munich.[4] Read the full article here:
The table provides an overview of some of the newer muscle injury classification systems.
Comparison of recent muscle injury classification systems[edit | edit source] | ||||
| Chan et al., 2012[5] | Mueller-Wolfahrt et al., 2013[4] | Pollock et al., 2014[6] | Valle et al., 2017[7] | Prakash et al., 2018[8] |
Grading based in radiological finding and site of lesion
|
A. Indirect muscle disorder/injury
Functional muscle disorder Type 1:
Type 2:
Structural muscle injury Type 3:
B. Direct muscle injury
|
|
|
MRI-based grading
|
Predisposing Factors[edit | edit source]
Three types of muscle are at possible risk of injury:[1]
- Two-joint muscles. Specifically, the motion at one joint increases the passive tension of the muscle and leads to an overstretching injury.
- Muscles contracting eccentrically. Eccentric contractions, frequent during the deceleration phase of activity, may change the muscle tension and induce myofibre overload injury10.
- Muscles with a higher percentage of type II fibers. These are fast-twitch muscles that develop high- speed contractions. In this way, the muscle is more predisposed to injury. Most of the muscle activity in running and sprinting is eccentric, explaining why such strains most often occur in sprinters or ‘speed athletes’. The hamstrings, gastrocnemius, quadriceps, hip flexors, hip adductors, Erector Spinae, deltoid, and rotator cuff are most commonly injured.
The video below gives a good summary of the salient points
Signs and Symptoms[edit | edit source]
Symptoms of muscle strain include:[10]
- Swelling, bruising, or redness due to the injury
- Pain at rest
- Inability to use the muscle at all
- The weakness of the muscle or tendons
Risk Factors[edit | edit source]
Strains are not restricted to athletes and can happen while doing everyday tasks, Athletes are more at risk for developing a strain. It is common for an injury to occur when there is a sudden increase in duration, intensity, or frequency of activity.[11]
Treatment of Acute Strains[edit | edit source]
Muscle strain treatment depends upon an accurate diagnosis from your health professional. The severity of your muscle strain, and what function or loads your injured muscle will need to cope with, will impact the length of your healing and rehabilitation process.
The first-line treatment for a muscular strain in the acute phase includes five steps commonly known as P.R.I.C.E.[12]
- Protection: Apply soft padding to minimize impact with objects.
- Rest: Rest is necessary to accelerate healing and reduce the potential for re-injury.
- Ice: Apply ice to induce vasoconstriction, which will reduce blood flow to the site of injury. Never ice for more than 20 minutes at a time.
- Compression: Wrap the strained area with a soft-wrapped bandage to reduce further diapedesis and promote lymphatic drainage.
- Elevation: Keep the strained area as close to the level of the heart as is possible in order to promote venous blood return to the systemic circulation.
The first treatment is usually an adjunctive therapy of NSAIDs and Cold compression therapy. Cold compression therapy acts to reduce swelling and pain by reducing leukocyte extravasation into the injured area.[14] NSAIDs such as Ibuprofen/paracetamol work to reduce the immediate inflammation.
New treatments are an expanding area. A growing number of health care professionals are using biological factors to favor the healing of muscle injuries. However despite relatively widespread use, the scientific evidence behind such products is scanty, and the results probably less dramatic than what reported in the lay literature.[15] The use of platelet-rich- plasma (PRP) injections which have been shown to accelerate recovery from non-surgical muscular injuries.[16]
In the second phase, mobilization must begin as soon as possible but gradually and within the limits of pain, Mobilisation has shown to improve injured skeletal muscle regeneration.
The cardiovascular conditioning program should be performed with a low impact. Since core stability programs have been shown to improve results in terms of lower re-injury rates and enhanced return to play, they must be introduced along with the specific rehabilitation program of the injured muscle.
After 2 or 3 weeks of injury, tension should be applied in the line of normal stresses for proper remodeling anatomically and functionally.
Proprioceptive and endurance training is used in the advanced stages of rehabilitation. After the athlete has regained full, pain-free active ROM and over 90% strength bilaterally, full participation is allowed. The maintenance programs should be continued to avoid any dysfunctional adaptation or compensation.[17].
References[edit | edit source]
- ↑ 1.0 1.1 Garrett WE. Muscle strain injuries. Am J Sports Med. 1996; 24:S2-88
- ↑ Järvinen M, Tero AH. Muscle strain injuries. Rheumatology. 2010(2); 12: 155-161
- ↑ Kneeland JP. MR imaging of muscle and tendon injury. Eur J Radiol. Nov 1997; 25(3):198-208
- ↑ 4.0 4.1 Mueller-Wohlfahrt HW, Haensel L, Mithoefer K, Ekstrand J, English B, McNally S, Orchard J, van Dijk CN, Kerkhoffs GM, Schamasch P, Blottner D. Terminology and classification of muscle injuries in sport: the Munich consensus statement. British journal of sports medicine. 2013 Apr 1;47(6):342-50.
- ↑ Chan O, Del Buono A, Best TM, Maffulli N. Acute muscle strain injuries: a proposed new classification system. Knee Surgery, Sports Traumatology, Arthroscopy. 2012 Nov;20(11):2356-62.
- ↑ Pollock N, James SL, Lee JC, Chakraverty R. British athletics muscle injury classification: a new grading system. British journal of sports medicine. 2014 Sep 1;48(18):1347-51.
- ↑ Valle X, Alentorn-Geli E, Tol JL, Hamilton B, Garrett WE, Pruna R, Til L, Gutierrez JA, Alomar X, Balius R, Malliaropoulos N. Muscle injuries in sports: a new evidence-informed and expert consensus-based classification with clinical application. Sports medicine. 2017 Jul;47(7):1241-53.
- ↑ Prakash A, Entwisle T, Schneider M, Brukner P, Connell D. Connective tissue injury in calf muscle tears and return to play: MRI correlation. British journal of sports medicine. 2018 Jul 1;52(14):929-33.
- ↑ tech insider What happens when you pull a muscle Available from: https://www.youtube.com/watch?v=nMZVIb5U5fI (last accessed 2.6.2019)
- ↑ Brumitt, Jason; Cuddeford, Tyler "CURRENT CONCEPTS OF MUSCLE AND TENDON ADAPTATION TO STRENGTH AND CONDITIONING". International Journal of Sports Physical Therapy. (2015).748–759.
- ↑ American Academy of Orthopedic Surgeons. Available from: orthoinfo.aaos.org. (accessed 26 February 2019).
- ↑ T. A. Järvinen, et al., "Muscle injuries: optimising recovery" , Best Pract Res Clin Rheumatol., 21 (2) April 2007, pp. 317-31.
- ↑ Steward Health Care System,RICE:Rest,Ice,Compress&Elevate Available from: https://youtu.be/1RRZkGm8Gyk (Assessed 31 July 2020)
- ↑ American Academy of Pain Management: ).Archived from the original (PDF) on 2017-10-31. (Accessed 25 Feb 2019)
- ↑ Maffulli N, Oliva F, Frizziero A, Nanni G, Barazzuol M, Via AG, Ramponi C, Brancaccio P, Lisitano G, Rizzo D, Freschi M. ISMuLT Guidelines for muscle injuries. Muscles, ligaments and tendons journal. 2013 Oct;3(4):241. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3940495/ (last accessed 2.6.2019)
- ↑ Halpern, B ; Chaudhury S; Scott A. "The role of platelet-rich plasma in inducing musculoskeletal tissue healing". HSS journal;2012;37–145.
- ↑ Page P. Pathophysiology of acute exercise-induced muscular injury: clinical implications. 1995; 29-34.