Neurofibromatosis Type II
Original Editor - Wendy Walker
Lead Editors - Wendy Walker, Kim Jackson, WikiSysop, Rishika Babburu and Lucinda hampton
Clinically Relevant Anatomy
[edit | edit source]
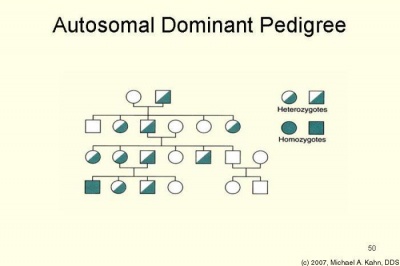
Neurofibromatosis Type II, AKA NF2 is inherited as an autosomal dominant condition, although half of affected individuals have NF2 as a result of a new (de novo) gene mutation. The manifestations of NF2 result from mutations in (or, occasionally, deletion of) the NF2 gene, located on the long arm of chromosome 22. Affected individuals need only 1 mutated or deleted NF2 gene to exhibit signs of the condition.
The NF2 gene product known as merlin
Mechanism of Injury / Pathological Process[edit | edit source]
NF2 is an autosomal dominant genetic disorder caused by mutations on chromosome 22[1]. Patients usually have multiple Central Nervous System tumours; most typically a patient will be found to have bilateral Acoustic Neuromas (AKA Vestibular Schwannomas).
NF2 is caused by mutations of the "Merlin" gene[2] which influences the form and movement of cells, and acts as a tumour suppressor; so reduced action of this protein, or decreased production of it causes tumours in both the central and peripheral nervous systems to develop.
Histological findings in NF2 tumours show distinct characteristics which differ from non-NF2 Acoustic Neuromas. Depending on the severity of the underlying mutation, multiple other CNS tumours can also be found, especially meningiomas, schwannomas, and gliomas, some of them involving cranial nerves.
Clinical Presentation[edit | edit source]
Presenting symptoms[edit | edit source]
These may include the following:
- Hearing loss, ringing in the ears, and balance problems associated with vestibular nerve lesions
- Visual deficits
- Cranial nerve palsies
NF2 is associated with significant morbidity and decreased life span. Furthermore, diagnosis in childhood is often difficult because of the absence of central nervous system (CNS) involvement at a young age[3].
Although the genetic change causing NF2 is present at conception, the clinical manifestations occur over many years. The typical age of onset of symptoms is in the late teens to early 20s, but the age range covers the entire life span.
Complications of NF2[edit | edit source]
The following complications frequently occur:
Unilateral or, frequently, bilateral vestibular schwannomas leading to tinnitus, hearing loss, and/or problems with balance
Spinal cord schwannomas are quite common in NF2 and result in significant morbidity. Intracranial meningiomas are common. Spinal cord ependymomas, astrocytomas, and meningiomas also occur, but less frequently.
Gliomas, ependymomas, and other cerebral, cerebellar, or spinal cord lesions that may result in neurologic deficits, seizures, and/or hydrocephalus
Peripheral nerve schwannomas, mixed tumors, and, occasionally, neurofibromas
Peripheral neuropathies
Visually significant juvenile cataracts
Nonvestibular schwannomas occur in more than half of patients, and are often diagnosed in patients with an earlier age at diagnosis of NF2. Cranial nerves 3 and 5 are most commonly involved.
Diagnostic Procedures[edit | edit source]
Clinical diagnosis of NF2 requires that an individual present with at least 1 of the 3 following disease indications:
- Bilateral eighth nerve tumours visualized on MRI scan
- First-degree relative with documented NF2 for an individual with a unilateral eighth nerve mass
- First-degree relative with documented NF2 for an individual with at least 2 of the following findings: meningioma, schwannoma, glioma, juvenile cataract.
However, because approximately half of cases result from new mutations, family history is often negative.
Diagnosis of NF2 involves the following:
Genetic testing
Imaging studies
Auditory, ophthalmic, and histologic examinations
Management / Interventions[edit | edit source]
Medical care for patients with NF2 consists of routine examinations focusing on early detection of some of the potential complications related to CNS or spinal cord lesions[4].
Guidelines for the care of the patient with NF2:
Annual testing as follows:
- Neurologic examination to identify changes in neurologic status which suggest progression of the disease
- Hearing test and when indicated, referral to an audiologist
- Ophthalmologic testing
- MRI to monitor existing lesions and/or look for new lesions
Treatment of symptomatic tumours, including:
Surgical resection is most common, especially for acoustic neuromas.
Occasionally, radiation and/or chemotherapy may be recommended.
Differential Diagnosis[edit | edit source]
Neurofibromatosis Type 1 (NF1) differs from NF2 in that NF1 patients have large numbers of skin lesions, whereas NF2 patients generally have fewer skin lesions.
Brainstem Gliomas
Intracranial Ependymomas
Physiotherapy[edit | edit source]
Customized vestibular rehabilitation incorporating adaptation, habituation, balance and mobility has been demonstrated to improve balance in patients with Acoustic Neuroma[5].
If the Facial Nerve is affected, causing facial palsy, then physiotherapy is indicated, as set out on the Facial Palsy page.
References[edit | edit source]
- ↑ Evans DG, Huson SM, Donnai D, Neary W, Blair V, Teare D, et al. A genetic study of type 2 neurofibromatosis in the United Kingdom. I. Prevalence, mutation rate, fitness, and confirmation of maternal transmission effect on severity. J Med Genet 1992;29:841-6
- ↑ Striedinger K, VandenBerg SR, Baia GS, McDermott MW, Gutmann DH, Lal A (November 2008). "The neurofibromatosis 2 tumor suppressor gene product, merlin, regulates human meningioma cell growth by signaling through YAP". Neoplasia 10 (11): 1204–12
- ↑ Matsuo M, Ohno K, Ohtsuka F. Characterization of early onset neurofibromatosis type 2. Brain Dev. Feb 13 2013
- ↑ Aboukais R, Baroncini M, Zairi F, Bonne NX, Schapira S, Vincent C, et al. Prognostic value and management of spinal tumors in neurofibromatosis type 2 patients. Acta Neurochir (Wien). May 2013;155(5):771-7.
- ↑ Vereeck L, Wuyts FL, Truijen S, De Valck C, Van de Heyning PH. The effect of early customized vestibular rehabilitation on balance after acoustic neuroma resection.. Clin Rehabil. 2008 Aug;22(8):698-713