Oxalosis
Original Editors - Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Oscar Lewis, Shelby Kissel, Lucinda hampton, 127.0.0.1, Elaine Lonnemann, Tomer Yona, WikiSysop and Kim Jackson
Introduction[edit | edit source]
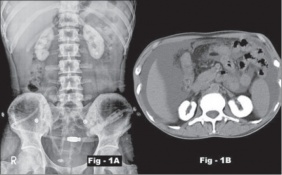
Oxalosis is supersaturation of calcium oxalate in the urine (hyperoxaluria), which in turn results in kidney stones and cortical nephrocalcinosis. It can be a hereditary or secondary condition.
Oxalate is a by-product of normal metabolism. There are no enzymes in the human body that can break down oxalate. Oxalate must be excreted from the body through urine. The excess crystals then collect in other parts of the body, accumulating first in the blood, then the eyes, bones, muscles, blood vessels, heart and other major organs. If untreated Oxalosis can lead to death.[1]
Epidemiolgy[edit | edit source]
Hyperoxaluria is an autosomal recessive disorder and is more common in Mediterranean countries. The most common subtype is primary hyperoxaluria type 1 which is responsible for approximately 80% of cases[2]. Secondary Hyperoxaluria is less common and the prevalence of Oxalosis due to this diagnosis is unknown.[3]
Etiology[edit | edit source]
Calcium oxalate deposition most commonly affects the bone, bone marrow, blood vessels, central nervous system, peripheral nerves, retina, skin, and thyroid. There are two forms of this condition:
Primary: an autosomal recessive disease that is expressed in childhood. In this type, the liver doesn't create enough of an enzyme that prevents overproduction of oxalate, or the enzyme doesn't work properly. Excess oxalate is eliminated through the kidneys, in the urine. The extra oxalate can combine with calcium to create kidney stones and crystals, which can damage the kidneys and cause renal failure.
Secondary: usually related to an over ingestion of oxalic acids or its precursors (e.g. vitamin C) in patients with kidney or hepatic chronic diseases, especially during long-term dialysis[2]
- Dietary Hyperoxaluria: Consuming foods high in oxalate content can increase levels of oxalate in the urine and increase the risk of kidney stones. Foods that are high in oxalic acids include rhubarb, spinach, celery and cocoa[4]
- Enteric Hyperoxaluria: Certain intestinal diseases (Crohn's_Disease and Short Bowel Syndrome) can cause an increase in absorption of oxalate from foods therefore increasing the oxalate excreted in the urine.
- Kidney failure due to reasons other than Hyperoxaluria in which oxalate can no longer be excreted from the body[5].
Characteristics/Clinical Presentation[edit | edit source]
Typical presentation is kidney stones and global (cortical and medullary) nephrocalcinosis (is a disorder that occurs when too much calcium is deposited in the kidneys) at an early age[2].
A common symptoms that appear during the initial stages of the disease an infection of the urinary tract or passing of a kidney stone. Although only reported in a minimal number of cases, the presence of the condition may first present as kidney failure. Also, others may not present with overwhelming symptoms initially and may be unaware until the third to fifth decades of life. [6]
Treatment[edit | edit source]
When left untreated, hyperoxaluria will ultimately lead to renal failure, which in turn results in oxalosis: a condition in which calcium oxalate crystals are deposited in extrarenal organs.
Renal transplant is the only treatment for patients with renal failure and systemic oxalosis as dialysis is not sufficient to prevent disease progression.[2]
Systemic Involvement[edit | edit source]
Once the kidneys are no longer able to keep up with excretion of oxalate, the crystals begin to accumulate in the blood. Once the oxalate crystals begin circulating in the blood stream, they are free to deposit into other structures of the body. Most bodily systems can be affected by oxalate accumulation. Due to the vast structures that can be affected by oxalosis, the disease can become fatal when accumulation becomes excessive.
Physical Therapy Management[edit | edit source]
Physical therapy is currently not recognized as a primary method of treatment for oxalosis. However, physical therapy treatment may be indicated to address the functional limitations and impairments that a patient develops from excessive oxalate accumulation.
- Physical therapy treatment would be needed to rehabilitate patients post surgical bone correction.
- Patients who are apprehensive to movement, displaying reduced range of motion and strength deficits, would benefit from physical therapy to address such limitations.
- Physical therapy treatment may focus on joint protection strategies, as well as energy conservation techniques.
References[edit | edit source]
- ↑ Oxalosis - Rare Metabolic Condition that Affects Children's the Kidneys and Liver | St. Louis Children's Hospital [Internet]. Stlouischildrens.org. 2016 [cited 7 April 2016]. Available from: http://www.stlouischildrens.org/diseases-conditions/oxalosis
- ↑ 2.0 2.1 2.2 2.3 Radiopedia Oxalosis Available:https://radiopaedia.org/articles/oxalosis (accessed 2.4.2022)
- ↑ Kelly E. Encyclopedia of Human Genetics and Disease [2 volumes] [Internet]. Google Books. 2016 [cited 7 April 2016]. Available from: https://books.google.com/books?id=SjfKybobUIYC&pg=PA621&lpg=PA621&dq=prevalence+oxalosis&source=bl&ots=V0ysYYxVIr&sig=pdQ1gGzyCzs_Bu2PpOAncYR67e0&hl=en&sa=X&ved=0ahUKEwiv_Ni5tf3LAhWK7iYKHajDCaw4ChDoAQgeMAI#v=onepage&q=prevalence%20oxalosis&f=false
- ↑ Foods High in Oxalate-Topic Overview [Internet]. WebMD. 2016 [cited 7 April 2016]. Available from: http://www.webmd.com/kidney-stones/tc/foods-high-in-oxylate-topic-overview
- ↑ Oxalosis & Hyperoxaluria Foundation » Learn [Internet]. Ohf.org. 2016 [cited 7 April 2016]. Available from: http://ohf.org/overview/
- ↑ Plumhoff, Masoner, Lieske, Milliner. Communiqué - Primary Hyperoxaluria and Oxalosis: New Methods for Diagnosis - Mayo Medical Laboratories [Internet]. Mayomedicallaboratories.com. 2016 [cited 7 April 2016]. Available from: http://www.mayomedicallaboratories.com/articles/communique/2013/07-hyperoxaluria-oxalosis/index.html