Hand Pulleys
Top Contributors - Curtil Louis, Kim Jackson, Vidya Acharya, Lucinda hampton, Admin, Aya Alhindi, Candace Goh, WikiSysop and Aminat Abolade
Definition/Description[edit | edit source]
The pulley system is made of thickened areas of the flexor tendon sheath and plays an important role in:
- Flexion.
- Accurate tracking of tendons.
- Maintaining apposition of tendons and bones across joints preventing them from pulling away and bowstringing.
- Provides fulcrum to elicit movement (flexion and extension)[1]
Any damage to a part of flexor tendon pulley system can affect the motor performance of the digits. The pulley system plays a crucial role in maintaining an angle of approach of the flexor tendons onto its insertion site and retinacular restrainer.[1]
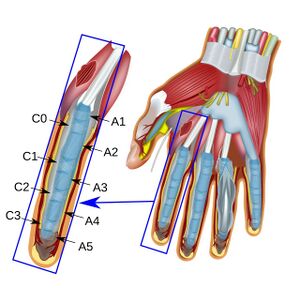
There are five flexor tendon pulleys in the fingers that are named A1-A5, and consists of annular ligament pulleys, and cruciate pulleys i.e. The flexor tendon pulley system. The thumb only has two pulleys that are described as A1 and A2.
Flexor pulley system consists of the following:
- Palmar Aponeurosis Pulley
- 5 Annular Pulleys
- 3 Cruciform pulleys.
Together, these form a fibro-osseous tunnel on the palmar aspect of the hand through which passes the deep and superficial flexor tendons.
Flexor tendon pulley system maintains flexor tendons close to joint’s axis of motion and prevents bowstringing.
NB Finger flexors attachments
- FDP: flexor digitorum profundus (the deeper of the two)
- FDS: flexor digitorum superficialis (the more superficial muscle)
Although the FDP is deep to the FDS over most of its course, it attaches to the skeleton more distally, because it passes through a split in the FDS tendon[2].
Clinically Relevant Anatomy[edit | edit source]
The flexor tendons of the fingers run through a complex structure called the digital flexor sheath. The sheath holds the flexor tendons near to the bone, enabling them to successfully "turn a corner" and convert the force generated in the muscle-tendon unit into movement at the phalanges.[3]
The sheath is composed of two distinct tissue components:[4]
- Synovial or membranous component.
- Retinacular or pulley component.
The membranous component is composed of a closed synovium lined tube and is most clearly seen between the flexor pulleys. It functions to stretch and compress with flexion and extension of the digits.
The pulley component of the sheath consists of fibrous tissue condensations which wrap around the flexor tendons.[4]The flexor pulley component is composed of visceral and parietal component extending from metacarpal bone to the distal inter-phalangeal joint. It is overlaid by a series of retinacular structures at 5 points on the flexor tendon sheath[1].
Annular Pulley System[1][edit | edit source]
The retinacular structures are focal, well-defined thickened areas of tendon sheath which are known as the Annular Pulley System.
- First Annular Pulley (A1): Arises: near palmar plate of MCP. Extends till the level of the base of MCP.
- Second Annular Pulley (A2): Arises from the volar aspect of the proximal part of the proximal phalanx. Extends to the junction of proximal 2/3rd and distal 1/3rd of the proximal phalanges.
- Third Annular Pulley (A3): Extends over the region of the proximal phalangeal joint and is small.
- Forth Annular Pulley (A4): It lies in the mid-portion of the middle phalanx.
- Fifth Annular Pulley (A5): Lies in the region of the distal interphalangeal joints.
The A2 and A4 are the major pulleys of the system (inserting directly to the bone) and are most prone to injury. The A1, A3, and A5 pulleys are more flexible and attach to the volar plate, a ligament that connects two phalanges together.[5] Also researches have suggested that the second Annular Pully (A2) is the strongest pulley followed by A1 and A4.[1]
Cruciate Pulley System[1][edit | edit source]
Additional crossing fibres between the components of the Annular Pulley System are called Cruciate Pulley System. They provide the necessary flexibility for approximation annular pulley at flexion and also maintaining integrity of the flexor sheaths.
- First Cruciate Pulley (C1): Located between A2 and A3
- Second Cruciate Pulley (C2): Between A3 and A4
- Third Cruciate Pulley (C3): Lies between A4 and A5.
Function[edit | edit source]
- The primary role of the flexor pulley system is to convert linear translation and force in the muscle-tendon into rotation and torque at the finger joints.[1]
- Facilitates smooth gliding of the tendons.
- Pulleys from retinacular component provide a mechanical advantage to flexion.
- Synovial fluid bathes and provides nutrition.[6]
- The pulleys create efficient mechanics for your fingers by maximizing the amount of finger flexion gained per muscle contraction length. Without pulleys, the tendon would pull away from the joint’s axis of rotation during flexion and decrease the functionality of the system.[7]
- The pulleys allow us to selectively bend the PIP or DIP joints by fractionating movement at our finger.[5]
Pathology[edit | edit source]
The pulley system (as a part of the tendon sheath) and flexor tendons form a functional unit so injuries of the tendon sheath are often associated with flexor tendon injuries[8]
Rupture or injury to the A2 and A4 pulley results in a loss of torque at the DIP and PIP joints, These ruptures can occur when a sudden extension of the digit is preceded by a large external load onto the flexed digit, as in a rock climbing or martial arts accidents. A “bowstringing” action is seen, in which the affected finger fails to flex fully and is associated with pain or discomfort. This is accompanied by a significant decrease in work and excursion efficiency[9].
Around 40% of all reported rock climbing injuries occur at the A2 and A4 pulleys of the flexor tendons. The mechanism of injury is predictable and involves:
- Closed crimp hand position
- Repetitive motion
- Excessive force
- Acute loading[10]
Pulley injuries can be classified according to 3 grades:
Grade I: Sprain in the finger ligament.
- Symptoms: Locally pain, pain when squeezing or climbing
Grade II: Partial rupture of the pulley.
- Symptoms: locally pain at the pulley, pain while extending the finger and while climbing
Grade III: Complete rupture of the pulley causing bowstring of the tendon.
- Symptoms are: locally pain at the pulley, heard a pop or crack sound, swelling, pain when squeezing or climbing, pain during finger extension.
The annular pulleys are functionally important and commonly injured. They comprise a transversely orientated sheath of fibrous tissue that wraps over the flexor digitorum superficialis and the flexor digitorum profundus tendons.
Diagnostic Procedures[edit | edit source]
A fresh pulley injury results in local swelling, tenderness, and pain over the affected area. The main indicator to identify if a total rupture of a pulley has occurred is the appearance of the clinical bowstringing (In this case; when the finger is in flexion, the flexor tendon is taking the shortest line between the top and the base of the finger. Instead of following the phalange).
- Plain radiograph - Have no role in the diagnosis but may be requested in the acute setting of a finger injury. May shows soft tissue swelling.
- Ultrasound - Allows for dynamic testing with flexion stress on the affected digit. It is reported to be up to 100% accurate in identifying pulley injuries
A recent study about the diagnostic procedure of the pulley, was a comparison between the effectiveness of ultrasonography and MRI (Magnetic Resonance Imaging) scanning.
This study showed us that ultrasonography is a better diagnostic tool than the MRI. Not only because it’s an inexpensive method but also because you can have more precision and a better view with the ultrasonography.[11]
Medical Management[edit | edit source]
All A2 and a large proportion of A4 pulley ruptures require surgical repair. A1, A3 and A5 pulleys may be managed conservatively initially.
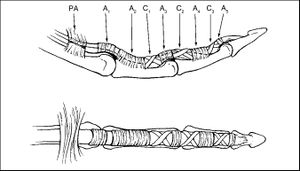
- Free extra synovial tendon grafts are the most common method currently in use for pulley reconstruction. The A2 and A4 are recommended to be reconstructed using multiple loops of free extra synovial tendon grafts in the same place where the original digital pulley was[12]. The strength of the repaired pulley is correlated with the number of loops in the tendon[13].
- Recent studies suggest that inter synovial donor tendons may be more efficient as free extra synovial tendon graft[14]. The inter synovial grafts had less frictions, what gives a better mobility in the digits.
- Another method is the use of the dorsal wrist retinaculum for the reconstruction of the annular digital pulleys[15]. The advantage of this technique is that the long pulley structure retains the flexor tendon in close proximity to the bone. It is a very efficient technique but has also been shown to be one of the weakest pulley reconstruction methods[16].
Physical Therapy Management[edit | edit source]
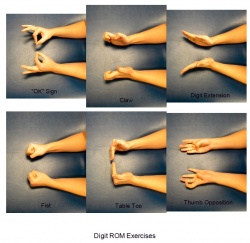
Grade 1: Pulley sprain[edit | edit source]
- A partial tear of a single pulley
- No need for immobilization. Begin gentle range-of-motion exercises—bend the finger until it feels tight, hold for 2–3 seconds, relax, and repeat 10 times for several sessions each day. Now perform the same exercise, only straighten the finger. Avoid pushing through pain.
Grade 2: Complete A4 or partial A2, A3 tear/rupture[edit | edit source]
- Either the A4 pulley is completely torn, or A2 and A3 are both partially torn
- One to two weeks of immobilization with a finger-immobilization splint or a pulley-protection splint, available online. Gentle range-of-motion exercises. Taping for three months while eg climbing.
Grade 3: Complete A2 or A3 tear/rupture[edit | edit source]
- A2 or A3 pulleys are fully torn
- One to two weeks of immobilization with a finger-immobilization splint or a pulley-protection splint, available online. Gentle range-of-motion exercises. Taping for six months.
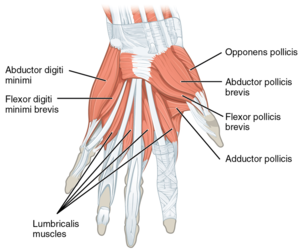
Grade 4: Annular Pulley Ruptures[edit | edit source]
- Single or multiple ruptures with possible lumbricalis muscle (the muscle between the metacarpal bones) or collateral ligament trauma
Surgical repair is recommended due to the increased risk of fixed flexion contractures, an inability to fully straighten the finger. (Some studies have also recommended surgical repair for grades 2 and 3, especially for elite-level climbers.) Consult with surgeon about rehab options, as they can vary depending on the damage.
- Rohrbough indicates that there remains some disagreement between researchers as to the treatment of pulley tears.[17]. Stretching is recognized as an important promoter of the formation of strong compacted scar tissue[18]. Stretching involves pulling the finger in the varus direction, effectively hyperextending the metacarpophalangeal joint and PIP joint[19]. An alternative therapy such a squeezing a ball may be useful. Such therapy is useful in promoting healing in the injury, it does not prevent atrophy of other healthy tissues.
- Minor A2 pulley injuries or partial tears with no evidence of bow stringing can be treated with either firm circumferential taping for 2 to 3 months to permit healing[20]. The effectiveness of pulley taping was tested and the effect was maximized (10% of bowstringing force) when the tape is positioned near the distal end of the proximal phalanx. The tape absorbed progressively less bowstringing force as the force produced at the fingertip increased[21]; non-stretch, zinc oxide tape of 1.3 cm width was used[20]. This result has two implications. Firstly, taping is likely to be most effective during the earlier stages of rehabilitation when the forces produced by the fingers are lower. Secondly, taping is unlikely to prevent pulley injuries, as these are likely to occur when forces on the pulley are maximal[22].
Key Research[edit | edit source]
- Digital Flexor Sheath: Repair and Reconstruction of the Annular Pulleys and Membranous Sheath
- Analysis of the gliding pattern of the canine flexor digitorum profundus tendon through the A2 pulley, Shigeharu Uchiyama1, Peter C. Amadio, Lawrence J. Berglund, Kai-Nan An Biomechanics Laboratory, Division of Orthopedic Research, Mayo Clinic, 200 First Street S.W., Rochester, MN 55905, USA Accepted 15 January 2008
- Zone II Combined Flexor Digitorum Superficialis and Flexor Digitorum Profundus Repair Distal to the A2 Pulley Jeffrey M. Pike, MD, Richard H. Gelberman, MD
Resources[edit | edit source]
Bron 1: http://www.orthobullets.com/hand/6004/flexor-pulley-system
Bron 2: http://edgar.brand.edgar-online.com/EFX_dll/EDGARpro.dll?FetchFilingHTML1?ID=5479903&SessionID=cg7xWq-zAf69x47
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Pedowitz R, Chung CB, Resnick D, editors. Magnetic resonance imaging in orthopedic sports medicine. Springer Science & Business Media; 2008 Oct 6. Accessed on 31.10.20
- ↑ Biomechanics of the hand Gwenda Sharp OTR and Dave Thompson PT Available from:https://ouhsc.edu/bserdac/dthompso/web/namics/hand.htm (last accessed 18.3.2020)
- ↑ Schöffl V, et al. Strength measurements and clinical outcome after pulley ruptures in climbers. Med Sci Sports Exerc. 2006;38(4):637–643. doi: 10.1249/01.mss.0000210199.87328.6a.
- ↑ 4.0 4.1 Doyle JR. Palmar and digital flexor tendon pulleys. Clin Orthop Relat Res. 2001;383:84–96. doi: 10.1097/00003086-200102000-00011.
- ↑ 5.0 5.1 Pulley injuries explained - part 1. The Climbing Doctor. (2022, November 20). Retrieved December 20, 2022, from https://theclimbingdoctor.com/pulley-injuries-explained-part-1/
- ↑ Bone spine Pulley system of hand Available from:https://boneandspine.com/flexor-tendon-pulley-system-of-hand/ (last accessed 17.3.2020)
- ↑ Neumann DA, Kelly ER, Kiefer CL, Martens K, Grosz CM. Kinesiology of the Musculoskeletal System : Foundations for Rehabilitation.
- ↑ Schöffl V, Heid A, Küpper T. Tendon injuries of the hand. World Journal of orthopedics. 2012 Jun 18;3(6):62.
- ↑ Bhatt F, Batul A, Schwartz-Fernandes F. A Potentially Inexpensive Diagnostic Method for A2 Pulley Ruptures. Cureus. 2019 Sep;11(9).
- ↑ Anytime physio Finger pulley injury Available from:https://anytimephysio.com.au/finger-pulley-tear-treatment/ (last accessed 17.3.2020)
- ↑ Martinoli, C., Bianchi, S., Nebolio, M., Derchi, L. E., Garcia, J. F. (2000) Sonographic evaluation of digital annular pulley tears. Skeletal Radiol. 29. 387-391
- ↑ Bunnell S. Repair of tendons in the fingers and descriptions of two new instruments. Surg Gynecol Obstet 26:103-110, 1918
- ↑ Widstrom CJ, Doyle JR, Johnson G. A mechanical study of the effectiveness of 6 digital pulley reconstruction techniques. Part 2. Strength of individual reconstructions. J Hand Surg Am 4:826-829,1989
- ↑ Nishida J, Amadio PC, Bettinger PC, et al. Excursion properties of tendon graft sources. interaction between tendon and A2 pulley. J Hand Surg Am 23:274-278, 1998
- ↑ Lister GD. Reconstruction of pulleys employing extensor retinaculum. J Hand Surg Am 4:461-464, 1979
- ↑ Kleinert HE, Bennett JB. Digital pulley reconstruction employing the always present rim of the other previous pulley. J Hand Surg Am 3:297-298, 1978
- ↑ Rohrbough, J. T., Mudge, M. K., Schilling, R. C. (2000) Overuse injuries in the elite rock climber. Med. Sci Sports Exerc. 32(8): 1369-1372
- ↑ R. S., Raya, M. A. (2001) Manual Modalities. in: Gonzalez, E. G., Myers, S. J., Edelstein, J. E., Lieberman, J. S., Downey, J. A. Physiological basis of rehabilitation medicine. 3rd ed. Butterworth Heinemann
- ↑ Gresham, N. (1996) High performance: warming up. High. 166: 14-15
- ↑ 20.0 20.1 Hand Injuries in Rock Climbing. Reaching the Right Treatment Peter J. L. Jebson, MD; Curtis M. Steyers, MD The Physician and Sportsmedicine – Vol 25: No5, May 1997
- ↑ Schweizer, A. (2000) Biomechanical effectiveness of taping the A2 pulley in rock climbers. J. Hand Surg. 25B. 102-107
- ↑ Warme, W. J., Brooks, D. (2000) The Effect of circumferential taping on flexor tendon pulley failure in rock climbers. Am. J. Sports Med. 28(5): 674-678