Sacroiliitis
Original Editors - Charlotte Fastenaekels
Top Contributors - Annelies Noppe, Lucinda hampton, Kim Jackson, Stéphanie Dartevelle, Charlotte Fastenaekels, Matthias Bossche, Admin, Laura Ritchie, Sally Ngo, 127.0.0.1, WikiSysop, Claire Knott, Wanda van Niekerk, Nicole Hills, Shreya Pavaskar, Rachael Lowe and Kai A. Sigel
Introduction[edit | edit source]
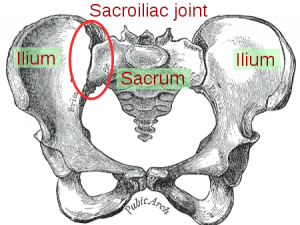
Sacroiliitis, is an inflammation of one or both sacroiliac (SI) joints, and a common cause of buttocks or lower back pain. Inflammation of the sacroiliac joint may occur secondary to osteoarthritis, pregnancy, spondyloarthropathies, and trauma.[1][2]
Etiology[edit | edit source]
Various conditions result in the inflammation of the SI joint, leading to significant pain.
- Osteoarthritis can cause degeneration of the joint resulting in pathologic articulation and motion leading to this condition.
- Spondyloarthropathies can cause significant inflammation of the joint itself eg Ankylosing spondylitis, Reactive arthritis, psoriatic arthritis, arthritis of chronic inflammatory bowel disease
- Pregnancy is another cause of the inflammation due to the hormone relaxin leading to the relaxation, stretching, and possible widening of the SI joint(s). The increased weight of pregnancy also causes extra mechanical stress on the joint, leading to further wear and tear.
- Trauma can cause direct or indirect stress and damage to the SI joint.
- Pyogenic sacroiliitis is the most frequently reported cause of acute sacroiliitis.
- Pain can originate from the synovial joint but can also originate from the posterior sacral ligaments[1]
Epidemiology[edit | edit source]
Reports on the prevalence of sacroiliac pain vary widely.
- Some studies report the prevalence as 10% to 25% of those with lower back pain.
- In those with a confirmed diagnosis, the presentation of pain was ipsilateral buttock (94% cases) and midline lower lumbar area (74%).
- Up to 50% of cases have radiation to the lower extremity: 6% to the upper lumbar area, 4% percent to the groin, and 2% percent to the lower abdomen[1]
- Symmetrical sacroiliitis is found in more than 90% of ankylosing spondylitis and 2/3 in reactive arthritis and psoriatic arthritis.
- It is less severe and more likely to be unilateral and asymmetrical in reactive arthritis, psoriatic arthritis, arthritis of chronic inflammatory bowel disease and undifferentiated spondyloarthropathy.[3][4]
- The hospital prevalence of sacroiliac diseases is 0,55%, the female sex predominates( 82,35%) and the mean age of 25,58 years. Gyneco-obstetric events are the predominant risk factors (47,05%). The etiologie found are bacterial arthritis (82,3%) mainly pyogenic (70,58%), osteoarthritis(11,7%) and ankylosing spondylitis (5,9%) .
Clinical Presentation[edit | edit source]
Symptoms of sacroiliitis can vary. People with sacroiliitis commonly present with ipsilateral or bilateral buttock and/or midline lower lumbar area pain. Up to 50% may have pain radiating to the lower extremity.
Sacroiliitis pain can be aggravated by:
- Prolonged standing
- Bearing more weight on one leg than the other
- Stair climbing
- Running
- Taking large strides[5]
Diagnosis[edit | edit source]
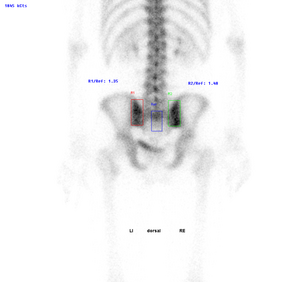
A medical history will be taken, including previous inflammatory disorders. Other tests include:
- Physical exam, movement tests - Spine is examined for proper alignment and rotation, and various physical movement tests are performed (see physio section below).
- Blood tests - looking for signs of inflammation.
- Imaging tests - X-rays, CT scans, and/or MRI scans may be ordered.
- Steroid injection - An injection of steroids into the sacroiliac joint is both a diagnostic test (if it relieves pain) and a treatment[5]
Outcome Measures[edit | edit source]
- Oswestry Disability Index (ODI) is most effective for persistent, severe disability
- Roland-Morris is more appropriate for mild to moderate disability.[6]
- Short-form McGill Pain Questionnaire
- The Assessment of Pain and Occupational Performance may also be appropriate.
Examination[edit | edit source]
Examine pelvis for proper alignment and rotation, inspection can reveal pelvic asymmetry. Measurement of the limbs can rule out a leg-length discrepancy. Inspect the spine for any abnormal curvatures or rotational abnormalities.
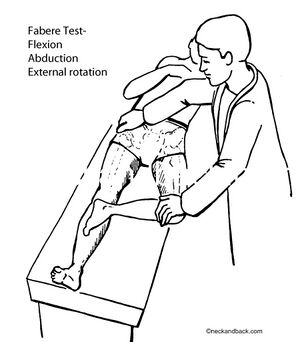
Special provocative tests can be very helpful in reproducing the patient’s pain:
- “Fortin finger sign”- reproduction of pain after applying a deep palpation with the four-hand fingers posteriorly at the patient's SI joint(s).
- FABER test- reproduction of pain after flexing the hip while also abducting and externally rotating the hip.
- Sacroiliac distraction test- reproduction of pain after applying pressure to the anterior superior iliac spine.
- SacroIliac compression test- reproduction of pain after applying pressure downward on the superior aspect of the iliac crest.
- Gaenslen test- reproduction of pain after having the patient flex the hip on the unaffected side and then dangle the affected leg off the examining table. Pressure is then directed downward on the leg to extend further the hip, which causes stress on the SI joint.
- Thigh thrust test- reproduction of pain after flexing the hip and applying a posterior shearing force to the SI joint.
- Sacral thrust test- reproduction of pain with the patient prone and then applying an anterior pressure through the sacrum.
The likelihood of SI joint mediated pain increases as the number of positive-provocative tests increase[1].
Management[edit | edit source]
Treatment depends on your signs and symptoms, as well as the cause of your sacroiliitis.
- Medications. Depending on the cause of your pain, the following may be recommended:
- Pain relievers. If over-the-counter pain medications don't provide enough relief stronger versions of these drugs may be ordered.
- Muscle relaxants. Medications such as cyclobenzaprine (Amrix, Fexmid) might help reduce the muscle spasms often associated with sacroiliitis.
- TNF inhibitors. Tumor necrosis factor (TNF) inhibitors [eg etanercept (Enbrel), adalimumab (Humira) and infliximab (Remicade)] often help relieve sacroiliitis that's associated with ankylosing spondylitis[5].
- Real-time image-guided intra-articular anesthetic/steroid injections can be performed for diagnostic and therapeutic effect. If the condition persists (6 to 8 weeks) with no improvement of at least 50 percent, repeat corticosteroid injections. Subsequently begin strengthening exercises including sit-ups and weighted side bends. Start with general conditioning of the back and increase slowly to low-impact walking or swimming. Take up normal activities with proper care of the back.[7]
- If the previous treatments do not provide adequate relief, then some providers will consider radiofrequency ablation[1].
- Joint fusion. Although surgery is rarely used to treat sacroiliitis, fusing the two bones together with metal hardware can sometimes relieve sacroiliitis pain.[5]
Physical Therapy Management[edit | edit source]
Physical therapy can be very helpful if the pain is due to hypermobility. Therapy can help to stabilize and strengthen lumbopelvic musculature. If the pain is due to immobility, then physical therapy can help increase mobilization of the SI joint. Depending on the diagnosis the following techniques may be used.
In the early treatment stages heat, cold or alternating cold with heat are effective in reducing pain.[8]
SI Belt: In the early stage a pelvic belt or girdle during exercise and activities of daily living can be used. These SI belts provide compression and reduce SI mobility in hypermobile patients. The belt should be positioned posteriorly across the sacral base and anteriorly below the superior anterior iliac spines. This belt may also be used when this condition becomes chronic (10-12 weeks).[9] [10][11]
Flexibility Exercises: Once the acute symptoms are under control, the patient can start with flexibility exercises and specific stabilizing exercises. To maintain SI and lower back flexibility, stretching exercises are principal. These exercises include side-bends, knee chest pulls, and pelvic-rocks with the aim of stretching the paraspinal muscles, the gluteus muscles and the SI joint. After hyperacute symptoms have resolved these kinds of exercises should be started. Each stretch is performed in sets of 20. These exercises should never surpass the patient’s level of mild discomfort.[12]
Stabilisation exercises: Specific pelvic stabilising exercises, postural education and training muscles of the trunk and lower extremities, can be useful in patients with sacroiliac joint dysfunctions. See core strengthening
After rehabilitation, low-impact aerobic exercises such as light jogging and water aerobics are designated to prevent recurrence.[13] [14][15][16][17]
If the patient has a leg length discrepancy or an altered gait mechanism, the most reliable treatment would be to correct the underlying defect. Sacroiliitis is also a feature of spondyloarthropathies. In this case, this condition should also be treated.[18][19][20][21][22]
See also the physiotherapy section in Sacroiliac Joint Syndrome
Conclusion[edit | edit source]
The majority of patients with sacroiliitis have an excellent outcome. However, the recovery may take 2-4weeks. Recurrences are common if patients do not change their lifestyle. Some series report a recurrence rate of over 30%[1].
Sacroiliitis is best managed by an interprofessional team that consists of a physical therapist, physician rheumatologist, and dietitian. Patient education is the key to good outcomes. All patients should
- Be informed that the condition is benign and will improve with conservative measures.
- Be encouraged to participate in a regular exercise program, lose weight, eat healthily and if applicable quit smoking.
- Participate in a Home exercise program to help prevent deconditioning.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Buchanan BK, Varacallo M. Sacroiliitis. InStatPearls [Internet] 2019 Feb 15. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK448141/ (last accessed 13.6.2020)
- ↑ Radiopedia Sacroiliitis Available:https://radiopaedia.org/articles/sacroiliitis (accessed 4.6.2022)
- ↑ J. Braun, J. Sieper and M. Bollow, Review Article Imaging of Sacroiliitis, Section of Rheumatology, Department of Nephrology and Endocrinology, UK Benjamin Franklin, Free University, Berlin; Department of Radiology, UK Charite´ , Humboldt University, Berlin, Germany,©2000 Clinical Rheumatology (A1)
- ↑ Peter Huijbregts, PT, MSc, MHSc, DPT, OCS, MTC, FAAOMPT, FCAMT fckLRSacroiliac joint dysfunction: Evidence-based diagnosis,fckLRAssistant Online Professor, University of St. Augustine for Health Sciences, St. Augustine, FL, USA, Consultant, Shelbourne Physiotherapy Clinic, Victoria, BC, Canada,Rehabilitacja Medyczna (Vol. 8, No. 1, 2004)(C)
- ↑ 5.0 5.1 5.2 5.3 Mayo Clinic Sacroiliitis Available:https://www.mayoclinic.org/diseases-conditions/sacroiliitis/symptoms-causes/syc-20350747 (accessed 4.6.2022)
- ↑ Davies, Claire C.1; Nitz, Arthur J. Psychometric properties of the Roland-Morris Disability Questionnaire compared to the Oswestry Disability Index: a systematic review. Physical Therapy Reviews, Volume 14, Number 6, December 2009 , pp. 399-408(10)
- ↑ Kapura et al. - Cooled radiofrequency system for the treatment of chronic pain from sacroiliitis: the first case-series.
- ↑ Davies, Claire C.1; Nitz, Arthur J. Psychometric properties of the Roland-Morris Disability Questionnaire compared to the Oswestry Disability Index: a systematic review. Physical Therapy Reviews, Volume 14, Number 6, December 2009 , pp. 399-408(10)
- ↑ Daniel L Riddle, Janet K Freburger, Symptomatic efficacy of stabilizing treatment versus laser therapy for sub-acute low back pain with positive tests for sacroiliac dysfunction: a randomized clinical controlled trial with 1 year follow-up, North American Orthopaedic Rehabilitation Research Network*, EUR MED PHYS 2004
- ↑ Davies, Claire C.1; Nitz, Arthur J. Psychometric properties of the Roland-Morris Disability Questionnaire compared to the Oswestry Disability Index: a systematic review. Physical Therapy Reviews, Volume 14, Number 6, December 2009 , pp. 399-408(10)
- ↑ Cusi MF; Paradigm for assessment and treatment of SIJ mechanical dysfuntion.; J Bodyw Mov Ther.; 2010;14(2):152-161.
- ↑ Davies, Claire C.1; Nitz, Arthur J. Psychometric properties of the Roland-Morris Disability Questionnaire compared to the Oswestry Disability Index: a systematic review. Physical Therapy Reviews, Volume 14, Number 6, December 2009 , pp. 399-408(10)
- ↑ Daniel L Riddle, Janet K Freburger, Symptomatic efficacy of stabilizing treatment versus laser therapy for sub-acute low back pain with positive tests for sacroiliac dysfunction: a randomized clinical controlled trial with 1 year follow-up, North American Orthopaedic Rehabilitation Research Network*, EUR MED PHYS 2004
- ↑ Carolyn A. Richardson, Chris J. Snijders, Julie A. Hides, Le´onie Damen, Martijn S. Pas, and Joop Storm. The Relation Between the Transversus Abdominis Muscles, Sacroiliac Joint Mechanics, and Low Back Pain. SPINE 2002; Vol. 27, No.4, p 399–405
- ↑ Davies, Claire C.1; Nitz, Arthur J. Psychometric properties of the Roland-Morris Disability Questionnaire compared to the Oswestry Disability Index: a systematic review. Physical Therapy Reviews, Volume 14, Number 6, December 2009 , pp. 399-408(10)
- ↑ C.A. Richardson; Muscle control-pain control. What would you prescribe?; Manual therapy;1995;2-10
- ↑ J.J.M. Pel; Biomechanical Analysis of Reducing Sacroiliac Joint Shear Load by Optimization of Pelvic Muscle and Ligament Forces; Annals of biomedical engineering; 2008; 36(3): 415–424.
- ↑ J. J. M. PEL, C. W. SPOOR, A. L. POOL-GOUDZWAARD, G. A. HOEK VAN DIJKE, and C. J. SNIJDERS, Biomechanical Analysis of Reducing Sacroiliac Joint Shear Load by Optimization of Pelvic Muscle and Ligament Forces, Department of Biomedical Physics and Technology, Erasmus MC, PO Box 2040, Rotterdam 3000 CA, The Netherlands, Annals of Biomedical Engineering, Vol. 36, No. 3, March 2008 (© 2008) pp. 415–424
- ↑ Steven P. Cohen, REVIEW ARTICLE Sacroiliac Joint Pain: A Comprehensive Review of Anatomy, Diagnosis, and Treatment, MD, Pain Management Divisions, Departments of Anesthesiology and Critical Care Medicine, Johns Hopkins Medical Institutions, Baltimore, MD and Walter Reed Army Medical Center, Washington, DC, ©2005 by the International Anesthesia Research Society
- ↑ Cusi, M.F., Paradigm for assessment and treatment of SIJ mechanical dysfunction, Journal of Bodywork & Movement Therapies (2010), doi:10.1016/j.jbmt.2009.12.004fckLR©2009 Elsevier Ltd. All rights reserved.
- ↑ Stacy L. Forst, PA-C, Michael T. Wheeler, DO, Joseph D. Fortin, DO, and Joel A. Vilensky, PhD, A Focused Review The Sacroiliac Joint: fckLRAnatomy, Physiology and Clinical Significance, Pain Physician. 2006;9:61-68, ISSN 1533-3159
- ↑ Stuart Porter; Tidy’s physiotherapy; Churchill Livingstone Elsevier; 14th edition; 2008; p513-530 (BOOK)