Spinal cord anatomy: Difference between revisions
No edit summary |
No edit summary |
(No difference)
| |
Latest revision as of 12:36, 1 July 2024
Original Editor - Naomi O'Reilly
Top Contributors - Naomi O'Reilly, Lucinda hampton, Kim Jackson, Jess Bell, Rucha Gadgil, Nikhil Benhur Abburi, Vidya Acharya, Tarina van der Stockt, Aminat Abolade, Stacy Schiurring, Admin and Ewa Jaraczewska
Introduction[edit | edit source]
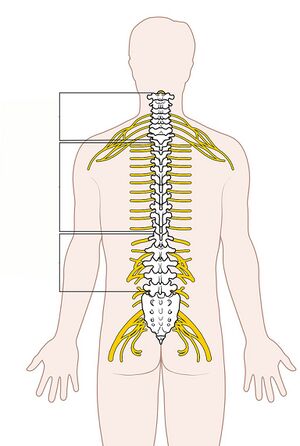
The spinal cord consists of a densely packed column of nerve tissue, which runs from the brainstem to around L1-2 in adults.[1] The terminal end of the spinal cord is the conus medullaris. The cauda equina extends from the conus medullaris.[2]
The spinal cord weighs around 35g and is only around 1cm in diameter.[3] It plays a vital role in facilitating functional activities as it sends information to and from the brain and periphery.[1]
Spinal Column Anatomy[edit | edit source]
The spinal cord sits inside the spinal or vertebral canal.[1] This canal also contains the meninges (membranes that protect the spinal cord), blood vessels, spinal nerve roots, and surrounding fatty and connective tissues.[5][6]
The spinal canal is formed by the vertebral foramina of the vertebral bodies. The anterior border of the canal is made up of the vertebral bodies, while the laminae (or vertebral arches) form the posterior border. The intervertebral discs and the anterior and posterior longitudinal ligaments provide lateral support. The diameter of the spinal canal varies, ranging from 12 to 22 mm in the cervical region and 22 to 25 mm in the lumbar region.
Adults typically have 33 vertebrae, including:
- seven cervical vertebrae
- twelve thoracic vertebrae
- five lumbar vertebrae
- five sacral vertebrae (fused in adults to form the sacrum)
- four coccygeal vertebrae (fused to form the coccyx)[6]
Each vertebra sits between a semi-rigid intervertebral disc. This provides a level of flexibility to the vertebral column. The cervical region is the most flexible area while the thoracic region is the least flexible.[6]
The spinal cord extends from the foramen magnum to the lowest border of the first lumbar vertebra. It is enlarged at two sites, the cervical (C3-T1) and lumbar (L1-S2) region.
Spinal Cord Internal Anatomy[edit | edit source]
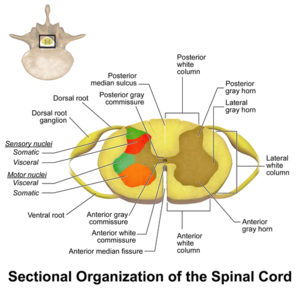
The spinal cord is the has grey matter and white matter:[8]
- grey matter is made up of the cell bodies of motor and sensory neurons, interneurons and neuropils[1]
- it is organised into regions called horns:
- anterior horn: location of motor nerves
- posterior horn: location of sensory nerves
- lareral horn: location of autonomic nerves
- it is organised into regions called horns:
- white matter surrounds the grey matter:[1]
- made up of interconnected fibre tracts
- these tracts are largely melinated sensory and motor axons
- ascending tracts: transmit information from the sensory receptors in the periphery for processing in the central nervous system
- descending tracts: transmit information to the periphery from the central nervous system
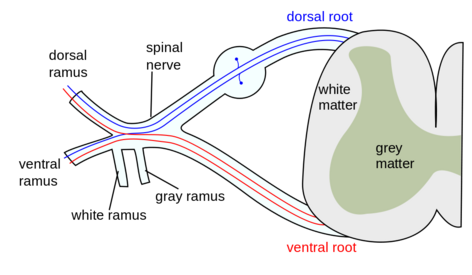
Spinal nerves:
- sensory nerve fibres enter the spinal cord via the posterior (dorsal) root - the cell bodies for these neurons are situated in the dorsal root ganglia
- motor and preganglionic autonomic fibres exit via the anterior (ventral) root
Spinal Cord[edit | edit source]
The spinal cord is the major conduit and reflex centre between the peripheral nerves and the brain and transmits motor information from the brain to the muscles, tissues and organs, and sensory information from these areas back to the brain. [9]In an adult, the spinal cord is approximately 45 cm long, cylindrical and slightly flattened anteriorly and posteriorly.[5].
Its upper end is continuous with the medulla, the transition is defined to occur just above the level of exit of the first pair of cervical nerves. There are fissures and sulci on the surface of the spinal cord which house the spinal nerves: anterior median fissure and posterior median fissure.[10]
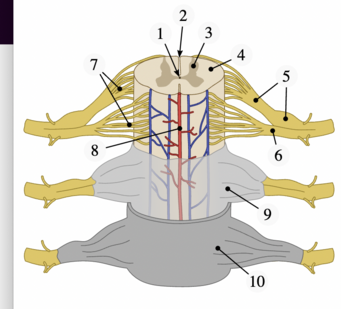
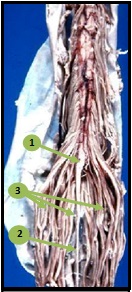
Its tapering lower end, the conus medullaris, terminates at the level of the L3 vertebra in neonates, and at the level of the L1-2 intervertebral disk in adults. It then becomes the cauda equina.[5]
The cauda equina[11]:
- Is the name given to the roots of the spinal nerves that extend beyond the termination of the spinal cord at the first lumbar vertebra in the form of a bundle of filaments within the spinal canal resembling a horse's tail.
- Has approximately 10 fiber pairs at its base: 3 to 5 lumbar fiber pairs; 5 sacral fiber pairs, and 1 coccygeal nerve.
- Primary function of the cauda equina is to send and receive messages between the lower limbs and the pelvic organs, which consist of the bladder, the rectum, and the internal genital organs.
Spinal Nerves[edit | edit source]
The term spinal nerve generally refers to a mixed spinal nerve that carries motor, sensory, and autonomic signals between the spinal cord and the body.
Humans have 31-pairs of spinal nerves, each roughly corresponding to a segment of the vertebral column. There are:
- eight cervical
- twelve thoracic
- five lumbar
- five sacral
- one coccygeal
While there are eight pairs of cervical spinal nerves there are only seven cervical vertebrae. This disparity occurs because the first pair of cervical spinal nerves exits above the first cervical vertebra just below the skull. However, the eighth pair of cervical spinal nerves exits below the last cervical vertebra. [5]
The spinal nerves are relatively large nerves that are formed by the merging of two nerve roots: a sensory nerve root and a motor nerve root.
- Sensory nerve roots emerge from the back of the spinal cord carrying sensory information via the posterolateral sulcus.
- Motor nerve roots emerge from the front of the spinal cord exit the spinal cord from the anterolateral sulcus. As they join, they form the spinal nerves on the sides of the spinal cord[12].
The anterior and posterior roots join to form two spinal nerves, one on either side of the spine, which then exit the vertebral canal through the intervertebral foramina. Once outside the intervertebral foramina they form peripheral nerves. [6]
Spinal Cord Muscle Innervation[edit | edit source]
For each spinal cord level and muscles innervated see Spinal Cord Muscle Innervation.
Spinal Motor Neurons[edit | edit source]
Alpha and Gamma motor neurons are both found in the anterior (ventral) horn.
- Alpha motor neurons are the largest motor neurons in the nervous system and innervate skeletal muscle.
- Gamma motor neurons innervate intrafusal muscle fibres of the muscle spindle.
Motor neurons are arranged somatotopically across the anterior horn. The more medially placed motor neurons innervate proximal muscles while laterally placed motor neurons innervate distal muscles. [5][6]
Associated Pathways[edit | edit source]
The central nervous system uses ascending and descending pathways to communicate with the external environment. The tracts and pathways complete the circuit in the spinal cord include:
Ascending Tracts:
- Dorsal column- medial lemniscus pathway
- Spinothalamic tracts
- Spinocerebellar tracts
Descending Tracts:
- Corticospinal Tract
- Corticonuclear tract
- Vestibulospinal tract
- Tectospinal tract
- Reticulospinal tract
- Rubrospinal tract
See Central Nervous System Pathways.
Clinical Pearls: Spinal Reflexes[edit | edit source]
Spinal Reflexes[13] are involuntary actions to stimuli involving simple circuits at the level of the spinal cord. They allow for near instantaneous responses because they can bypass the processing from the brain. Although spinal reflexes can bypass the cortical circuit, descending circuit of brainstem and cortex can still modulate the intensity of the response elicited.
These include:
- myotatic or stretch reflex (also known as the knee-jerk reflex): occur when muscle spindle stretch receptors are activated. Information is sent along the afferent neuron to the spinal cord where it synapses on the efferent neuron to the same muscle, causing that muscle to contract in response. At the same time, reciprocal inhibition occurs. The afferent neurons are also synapsing on inhibitory interneurons in the spinal cord that prevent contraction of the antagonistic muscles.
- flexor withdrawal reflex: occur in response to noxious stimuli. For example: when you touch a hot object, a pain receptor in your hand picks up the noxious stimulus and the afferent neuron carries the impulse to the spinal cord where it synapses on an interneuron. The interneuron then synapses with the efferent neuron which sends a signal to muscle in order to withdraw your hand.
Blood Supply[edit | edit source]
The majority of the spinal cord blood supply[14] is provided by the segmental spinal arteries, with further supply coming from the vertebral arteries via a single anterior spinal artery and paired posterior spinal arteries. The segmental and spinal arteries are linked by numerous anastomoses. [5][6]
Segmental Arteries: The segmental arteries give off radicular branches, cervical and thoracolumbar, which enter the intervertebral foramen and supply the anterior and posterior roots and spinal ganglion of the corresponding level. The spinal cord itself is supplied by unpaired medullary arteries that originate from segmental arteries. [5][6]
Spinal Arteries: The spinal arteries, arising from the vertebral artery, run longitudinally down the spinal cord.
- The unpaired anterior spinal artery lies in the anterior median fissure of the spinal cord and extends from the level of the lower brainstem to the tip of the conus medullaris, with the diameter steadily increasing below the T2 level. It supplies the ventral medial surface of the medulla and anterior 2/3 of the spinal cord.
- The paired posterior spinal arteries supply the dorsal columns and the all but the base of the dorsal horns bilaterally.
There are reinforcing branches from other arteries along the length of the cord and numerous anastomoses of the spinal arteries produce a vasocorona around the spinal cord. If occlusion occurs, it is normally of the anterior spinal artery, producing loss of power and spinothalamic sensory deficit, but dorsal column sensory capabilities are maintained. [5][6]
Spinal Veins: Blood from within the spinal cord travels through the intramedullary veins, to the anterior and posterior spinal veins, which form a reticulated network in the pia mater around the circumference of the cord throughout its length.
- The anterior two-thirds of the gray matter drain via the anterior spinal vein
- The posterior and lateral spinal veins drain the rest of the spinal cord. These vessels empty by way of the radicular veins into the external and internal vertebral venous plexuses, groups of valveless veins that extend from the coccyx to the base of the skull.
- The vertebral and deep cervical veins drain venous blood from the cervical spine into the superior vena cava; the posterior intercostal and lumbar veins drain venous supply from the thoracic and lumbar spine into the azygos and hemiazygos veins; and the median and lateral sacral veins drain venous supply from the sacrum into the common iliac vein. [5][6]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Harrow-Mortelliti M, Reddy V, Jimsheleishvili G. Physiology, Spinal Cord. [Updated 2023 Mar 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544267/
- ↑ DeSai C, Reddy V, Agarwal A. Anatomy, Back, Vertebral Column. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525969/
- ↑ Queensland Brain Institute. The spinal cord. Available from: https://qbi.uq.edu.au/brain/brain-anatomy/spinal-cord (last accessed 22 June 2024).
- ↑ Designed by Freepik at http://www.freepik.com
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 Moore KL, Agur AM, Dalley AF. Essential Clinical Anatomy. Philadelphia: Lippincott Williams & Wilkins; 2002 Mar.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Rohkamm Reinhard. Color Atlas of Neurology. Thieme; 2014 Sep 2.
- ↑ Spinal Cord. Blausen Medical. Retrieved on 26 January 2016.
- ↑ Henmar S, Simonsen EB, Berg RW. What are the gray and white matter volumes of the human spinal cord? J Neurophysiol. 2020 Dec 1;124(6):1792-1797.
- ↑ Francisco de Assis Aquino Gondim et al., Topographic and Functional Anatomy of the Spinal Cord, Medshape, 2015.
- ↑ Ganapathy MK, Reddy V, Tadi P. Neuroanatomy, Spinal Cord Morphology. [Updated 2022 Oct 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
- ↑ Rider LS, Marra EM. Cauda Equina and Conus Medullaris Syndromes. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
- ↑ Kaiser JT, Lugo-Pico JG. Neuroanatomy, Spinal Nerves. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from:
- ↑ Hultborn H. Spinal reflexes, mechanisms and concepts: from Eccles to Lundberg and beyond. Progress in neurobiology. 2006 Feb 1;78(3-5):215-32.
- ↑ Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Neuroscience. 2nd edition. Sunderland (MA): Sinauer Associates; 2001. The Blood Supply of the Brain and Spinal Cord.