Thoracic Anatomy
Introduction[edit | edit source]
This guide gives a general overview of the anatomy of the thoracic spine. It also includes some facts regarding pathophysiology in this region.
The sagittal plane alignment of the Thoracic spine is on average 35% (normal range is 20° to 50°).[1]
Important Structures
The important parts of the thoracic spine include:
Bones (vertebrae and ribs)[edit | edit source]
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to create the spinal column. The spinal column is the body’s main upright support. The cervical spine consists of 7 vertebrae, the lumbar spine has 5 vertebrae and other other bones of the spinal column are the sacrum and coccyx which both consist of fused vertebrae.
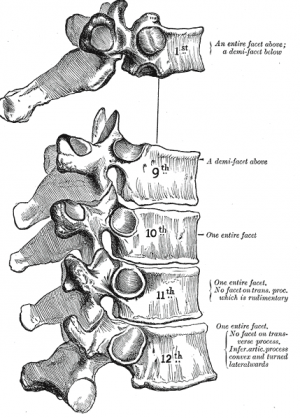
The middle 12 Thoracic vertebrae make up the thoracic spine and are made up of a combination of typical and atypical characteristics, each contributing to the unique structure and function of this region. The primary defining feature of the thoracic vertebrae is the presence of costal facets. These vertebrae exhibit six facets per vertebra: two on the transverse processes and four demifacets. The facets on the transverse processes connect to the tubercles on the associated ribs. The demifacets are on the superior and inferior posterolateral sides of the vertebrae and are paired on both sides. This arrangement enables the superior demifacet of inferior vertebrae to articulate with the head of the same rib that articulates with the inferior demifacet of a superior rib. For example, the inferior demifacets of T4 and the superior demifacets of T5 articulate with the head of rib 5. Understanding these typical characteristics sets the foundation for recognizing the unique features of both typical and atypical thoracic vertebrae.
While T5-T8 exhibit the most "typical" features shared by all thoracic vertebrae, including remarkable rotational ability, other vertebrae display distinctive attributes. T1 stands out with its complete superior costal facets and prominent spinous process, while T11 and T12 deviate from the norm by possessing singular pairs of costal facets and lacking facets on the transverse processes. Understanding these variations allows for a comprehensive understanding of the intricate anatomy and functionality of the thoracic spine:
Typical vertebrae:
- T5-T8 tend to be the most “typical” in that they contain features present in all thoracic vertebrae. T5-T8 have the greatest rotation ability of the thoracic region.
Atypical vertebrae:
- T1 - superior costal facets are “whole” costal facets. They alone articulate with the first rib; C7 has no costal facets. T1 does, however, have typical inferior demifacets for articulation with the second rib. Vertebral prominens name given to long prominent spinous process found at T1
- T11 and T12 are atypical - contain a single pair, “whole,” costal facet that articulate with the 11 and 12 ribs, respectively. They also lack facets on the transverse processes.[3]
- The primary characteristic of the thoracic vertebrae is the presence of costal facets. There are 6 facets per thoracic vertebrae: 2 on the transverse processes and 4 demifacets. The facets of the transverse processes articulate with the tubercle of the associated rib. The demifacets are bilaterally paired and located on the superior and inferior posterolateral aspects of the vertebrae. They are positioned so that the superior demifacet of inferior vertebrae articulates with the head of the same rib that articulates with the inferior demifacet of a superior rib. For example, the inferior demifacets of T4 and the superior demifacets of T5 articulate with the head of rib 5.
- The length of the transverse processes decreases as the column descends.
- The positioning of the ribs and spinous processes greatly limits flexion and extension of the thoracic vertebrae.
- Thoracic vertebrae have superior articular facets that face in a posterolateral direction.
- The spinous process is long, relative to other regions, and is directed posteroinferiorly. This projection gradually increases as the column descends before decreasing rapidly from T9-T12.[3]
- The intervertebral disc height, is, on average, the least of the vertebral regions.
- Vertebral body size: increases progressively from T1 to T12
- Spinal canal dimensions: varies from T1 to T12[1]
Ribs and sternum ( see link)
The ribs are the bony framework of the thoracic cavity.
- The ribs form the main structure of the thoracic cage protecting the thoracic organs, however their main function is to aid respiration.
- There are twelve pairs of ribs.
- Each rib articulates posteriorly with two thoracic vertebrae by the costovertebral joint. An exception to this rule is that the first rib articulates with the first thoracic vertebra only.
According to their attachment to the sternum, the ribs are classified into 3 groups: true, false, and floating ribs[4].
Joints[edit | edit source]
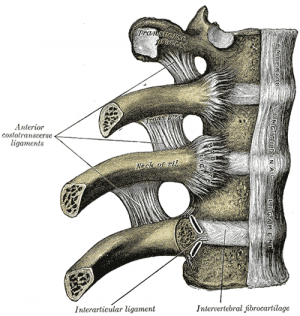
The thoracic spine mainly consists of costovertebral and costotransverse joints connecting the ribs to the vertebrae, and the intervertebral joints that join adjacent vertebrae. Understanding the specifics of these joints is crucial for rehabilitation professionals, particularly in diagnosing and treating thoracic spine issues.
- Costovertebral joints are unique to the thoracic spine. These are the joints where the head of each rib meets the vertebral body. They play a vital role in breathing mechanics.[5] Due to this ligament and the close articulation of components, only slight gliding movements can occur, further enhancing stability. The joints are also enveloped by a radiate ligament, which contributes to the restricted motion and overall stability.[5][6]It consists of:
- Superior costal facet of the corresponding vertebra
- Inferior costal facet of the superior vertebra
- Intervertebral disc separating the two vertebrae
- Costotransverse Joints connect the tubercle of the rib to the transverse process of the thoracic vertebrae. Like the costovertebral joints, these also contribute to the stability of the thoracic cage.[7]
- Intervertebral Joints are present between adjacent vertebral bodies and are essential for spine flexibility and stability. These joints can be categorised into two types:
- Between Vertebral Bodies: Adjacent vertebral bodies are joined by intervertebral discs made of fibrocartilage. This forms a type of cartilaginous joint known as a symphysis, which provides cushioning and allows slight movement.
- Between Vertebral Arches (Facet Joints): These are synovial joints formed by the articulation of superior and inferior articular processes from adjacent vertebrae. In the thoracic spine, the facet joints are angled at 60° to the transverse plane and 20° to the frontal plane. The superior facets face posteriorly, a little up and laterally, while the inferior facets face anteriorly, down, and medially. These joints allow for lateral flexion and rotation but restrict flexion and extension.
Structure and Function[edit | edit source]
The thoracic spine is a complex structure that serves multiple functions. Not only does it protect the spinal cord, but it also provides a frame for the ribcage and supports the upper body. Here are some key aspects:
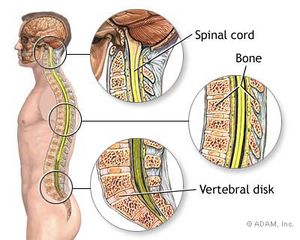
- Spinal Canal - The vertebral bodies and arches enclose a cavity known as the spinal canal, which houses and protects the spinal cord.
- Thoracic Cage - Comprised of the thoracic vertebrae, ribs, and sternum, the thoracic cage provides protection to vital organs such as the heart and lungs and plays a role in respiratory mechanics.
- Biomechanical Functions - The thoracic spine is less mobile than the cervical and lumbar regions due to the presence of the ribcage. However, it allows for limited flexion, extension, and rotation which are essential for various daily activities.
Ligaments[edit | edit source]
Ligaments play a crucial role in stabilising the thoracic spine and maintaining its structural integrity. Below are some of the significant ligaments in this area:
- Anterior Longitudinal Ligament - This ligament runs lengthwise down the front of the vertebral bodies and provides stability during extension movements.
- Posterior Longitudinal Ligament - Located on the back of the vertebral bodies, this ligament runs the full length within the spinal canal and helps resist hyperflexion.
- Ligamentum Flavum - This is a long elastic band that connects to the front surface of the lamina bones and also runs the full length within the spinal canal. It helps preserve the curvature of the spine.
- Supraspinous Ligament A strong fibrous cord that connects the apices of the spinous processes from the seventh cervical vertebra to the 3rd or 4th lumbar vertebrae.
- Ribs and Transverse Processes - Thick ligaments connect the ribs to the transverse processes of the thoracic spine, adding to the overall structural stability.
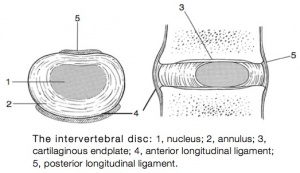
Intervertebral Disc[edit | edit source]
The intervertebral discs (IVD) Intervertebral discs act as cushions of fibrocartilage and are the main joints between adjacent vertebrae. In the thoracic region, there are 12 such discs. Their primary role is to provide flexibility and absorb shock, preventing vertebrae from grinding against each other.
Composition[edit | edit source]
Intervertebral discs consist of three major components: a tough outer layer called the annulus fibrosus (AF), a soft inner core known as the nucleus pulposus (NP), and cartilaginous endplates that anchor the discs to the adjacent vertebrae.
Function[edit | edit source]
These discs allow the spine to maintain flexibility without sacrificing strength. They also serve a shock-absorbing function, particularly vital in daily activities and physical exertion.
Variations in Thickness[edit | edit source]
The thickness of these discs varies along the spine, generally increasing from the upper to lower regions. However, in the thoracic area, their relative thickness to the size of the vertebral bodies is the smallest, reflecting the decreased range of motion in this region.
Changes with Age and Pathology[edit | edit source]
As people age, these discs may lose hydration and elasticity, leading to conditions like disc degeneration. Common disc-related issues include herniation and degeneration, affecting function and causing pain.
Muscles[edit | edit source]
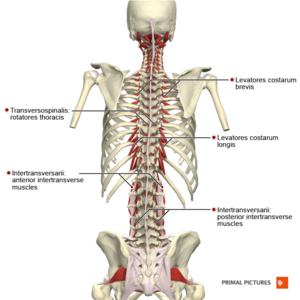
The muscles of the thoracic spine enable movement and provide stability. They are organised in layers, with each layer having specific roles and muscle groups.
Superficial Layer[edit | edit source]
Closes to the skin, muscles like Trapezius,Rhomboids, Latissimus Dorsi run from the vertebrae to the Scapula. Others like the Serratus anterior, Serratus Posterior, Pectoralis minor wrap around the ribcage, connecting to the shoulders.[8]
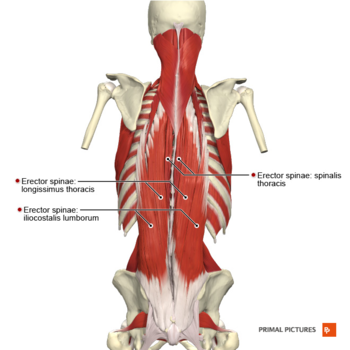
Middle Layer - Erector Spinae[edit | edit source]
Comprising the iliocostalis, longissimus and spinalis, these intrinsic back muscles form a column known as the erector spinae. They run over the lower ribs and thorax, crossing to the lower back.
Deep Layer - Transversospinalis[edit | edit source]
Underneath the erector spinae are the deep intrinsic muscles, collectively known as the transversospinales. Major muscles include the semispinalis, multifidus and rotatores, connecting the vertebrae and aiding in spinal rotation and stability.
Specialised Connective Tissue and Respiratory Muscles[edit | edit source]
The Thoracolumbar Fasciais an extensive area of connective tissue enclosing the intrinsic back muscles, important for thoracic musculature. Muscles connecting one rib to another, such as those involved in respiration, are also present.
Nerves[edit | edit source]
There are twelve pairs of thoracic spinal nerves that branch off from the spinal cord, one on the left and one on the right. These nerves exit between the vertebrae through the neural foramina. In the thoracic region, the spinal canal is notably narrower, leaving limited space for the spinal cord.
Functions of Thoracic Nerves[edit | edit source]
The thoracic nerves do not form plexuses. They supply the skin (dermatomes), and send sensory and motor fibres to deeper muscular structures, and various internal organs. They also carry both preganglionic and postganglionic sympathetic nerve fibres. These nerves serve as accessory respiratory muscles, particularly in situations of impaired breathing like dyspnea or phrenic nerve impairment.[2][9]
- T1 and the Brachial Plexus - The first thoracic nerve (T1) is part of the brachial plexus and plays a role in controlling the upper limbs.
- Sympathetic Chain - This chain runs alongside the spinal column and is essential for autonomic functions such as the fight-or-flight response.
- Intercostal Nerves - Branching from the spinal nerves, these run along the ribs and are key for sensation and muscle control in the thoracic region.
- Vagus Nerve - Although it doesn't originate in the thoracic region, the vagus nerve traverses it and is vital for functions like heart rate and digestion.
Pathophysiology[edit | edit source]
- Thoracic Radiculopathy - Thoracic nerve root lesions account for less than 2% of all radiculopathies and are most commonly caused by diabetes and thoracic disk herniation[10]
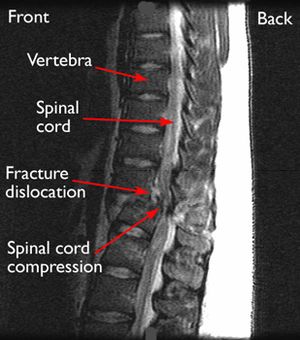
- Osteoporosis increases the risk for thoracic spinal fracture. A common type is a vertebral compression fracture (VCF) that can cause one or more bony bodies to flatten or become wedge shaped resulting in spinal cord and/or nerve compression. Sudden and acute back pain is associated with a VCF.[11]
- Different types of scoliosis—an abnormal side to side curvature of the spine—is well known to develop in the thoracic spine and may cause spinal deformity. eg Scheuermann’s disease, Posture related, Age related hyperkyphosis, Thoracic Hyperkyphosis, Forward Head posture,
- Ankylosing Spondylitis (Axial Spondyloarthritis)
- Spinal tumors can occur anywhere along the spine, but most occur in the thoracic (mid-to-upper back) region - About 70% of metastatic spinal tumors occur in the thoracic region, 20% occur in the lumbar (lower back) region, fewer occur in the cervical region.[12]
- More than half of spinal cord injuries occur in the cervical area, a third occur in the thoracic area, and the remainder occur mostly in the lumbar region.[13]
- T4 syndrome or upper thoracic syndrome was described as “a pattern that involves upper extremity paraesthesia”. It can be caused by thoracic hypomobility but can also have a sympathetic origin.
- The Slipping Rib Syndrome is an infrequent cause of thoracic and upper abdominal intermittent pain and is thought to arise from hypermobility of the rib cartilage of the false and floating ribs (these are the most involved in this syndrome)[14]
- Rib Stress Fracture is a frequently occurring pathology in the rower’s community, with an incidence of 6 to 12%.[15]
Conclusion[edit | edit source]
The thoracic region includes vertebrae, ligaments, intervertebral discs, muscles, and nerves. Understanding the anatomy can assist with effective diagnosis and treatment planning. You can find out more about assessment and examination on this Physiopedia page Thoracic Examination
References[edit | edit source]
- ↑ 1.0 1.1 Othrobullets Thoracic spine Anatomy Available from:https://www.orthobullets.com/spine/2070/thoracic-spine-anatomy (last accessed 12.4.2020)
- ↑ 2.0 2.1 eOrthopod Thoracic spine anatomy Available from:https://eorthopod.com/thoracic-spine-anatomy/ (last accessed 12.4.2020)
- ↑ 3.0 3.1 Waxenbaum JA, Futterman B. Anatomy, Back, Thoracic Vertebrae.Available from:https://www.statpearls.com/kb/viewarticle/32138 (last accessed 12.4.2020)
- ↑ Safarini OA, Bordoni B. Anatomy, Thorax, Ribs. InStatPearls [Internet] 2019 Feb 19. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK538328/ (last accessed 14.4.2020)
- ↑ 5.0 5.1 Putz R, Pabst R. Sobotta Atlas of Human Anatomy. 23rd ed. Munich: Elsevier; 2008
- ↑ Teach me anatomy The Thoracic Spine Available from:https://teachmeanatomy.info/thorax/bones/thoracic-spine/ (last accessed 12.4.2020)
- ↑ Cramer GD, Darby SA. Clinical Anatomy of the Spine, Spinal Cord, and Ans. 3rd ed. St. Louis: Elsevier Health Sciences; 2014
- ↑ Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. Journal of orthopaedic & sports physical therapy. 2005 Apr;35(4):227-38.Available from:https://www.ncbi.nlm.nih.gov/books/NBK538319/ (last accessed 13.4.2020)
- ↑ David L. Felten MD, PhD, ... Mary Summo Maida PhD, in Netter's Atlas of Neuroscience (Third Edition), 2016 Available from:https://www.sciencedirect.com/topics/neuroscience/thoracic-nerves (last accessed 13.4.2020)
- ↑ John-Michael Li, Jinny Tavee, in Handbook of Clinical Neurology, 2019 Available from:https://www.sciencedirect.com/topics/neuroscience/thoracic-nerves (last accessed 13.4.2020)
- ↑ Spine universe. Thoracic spine. Available from:https://www.spineuniverse.com/anatomy/thoracic-spine (last accessed 13.4.2020)
- ↑ Spine health. Metastatic tumours Available from:https://www.spine-health.com/conditions/spinal-tumor/metastatic-spine-tumors (last accessed 13.4.2020)
- ↑ Reeve foundation SCI Available from:https://www.christopherreeve.org/living-with-paralysis/health/causes-of-paralysis/spinal-cord-injury (last accessed 13.4.2020)
- ↑ Slipping Rib Syndrome: An elusive diagnosis; [/www.sciencedirect.com.ezproxy.vub.ac.be%3A2048/science/journal/15260542 Paediatric Respiratory Reviews] [/www.sciencedirect.com.ezproxy.vub.ac.be%3A2048/science/journal/15260542/22/supp/C Volume 22], March 2017, Pages 44–46
- ↑ Warden SJ, Gutschlag FR, Wajswelner H, et al. Aetiology of rib stress fractures in rowers. Sports Med 2002; 32 (13): 819-36 (last accessed 13.4.2020)